Sarcoidosis is an inflammatory multisystemic disease of unknown origin characterized by noncaseating granulomas. Pulmonary involvement occurs in over 90% of cases, often with concurrent lesions in other organs.1 Isolated extrapulmonary presentations are uncommon, posing diagnostic challenges.
We present the case of a 43-year-old female patient who experienced prolonged fever, malignant hypercalcemia, and massive splenomegaly, initially suggestive of a neoplastic condition. The diagnosis of sarcoidosis was confirmed after a significant delay.
Case Report
A 43-year-old Tunisian woman was referred to our department due to a five-month history of vomiting, anorexia, constipation, and a 16 kg weight loss. Physical examination revealed an ill-appearing patient with a high fever. Abdominal examination showed an enlarged, firm spleen palpable below the umbilicus and hepatomegaly. Laboratory tests revealed hypercalcemia (3.25 mmol/L; reference range: 2.25–2.62 mmol/L), pancytopenia with microcytic anemia (8.6 g/dL; reference range: 12–16 g/dL), leucopenia (3730/mm3; reference range: 4000–10 000/mm3), lymphopenia (620/mm3; reference range: 1500–4000/mm3), and thrombocytopenia (135 000/mm3; reference range: 150 000–450 000/mm3). Neutrophil polynuclear count was 2420/mm3 (reference range: 1500–7000/mm3). The ferritin level was at 105 ng/mL (reference range: 20–200 ng/mL). Laboratory markers of inflammation were elevated: erythrocyte sedimentation rate (85 mm) and C-reactive protein (46 mg/L; reference range: < 8 mg/L). Serum protein electrophoresis revealed a polyclonal hypergammaglobulinemia at 28.8 g/L (normal range: 9–13.5 g/L). Renal and hepatic functions were within the normal range. Computed tomography (CT) of the thorax, abdomen, and pelvis revealed multiple, enlarged homogenous mediastinal and abdominal lymph nodes, hepatomegaly measuring nearly 22 cm, and a massive homogenous splenomegaly of 23 cm.
To treat hypercalcemia, the patient received intravenous fluids and 20 mg of oral prednisone per day, resulting in a reduction of calcium levels to < 2.5 mmol/L within the following days.
Histopathological examination of 10 mediastinal lymph nodes revealed tuberculoid lymphadenitis, characterized by multiple non-caseating granulomas, with no evidence of malignancy. Despite a negative tuberculin skin test, we initiated the national anti-tubercular protocol treatment: two months of isoniazid, rifampin, pyrazinamide, and ethambutol followed by four months of isoniazid and rifampin. This decision was based on the high prevalence of tuberculosis in our country and the persistence of high fever.
Six months later, the patient’s clinical condition continued to deteriorate. Physical examination revealed an even larger spleen and multiple erythematous maculo-papular lesions on the arms [Figure 1a], back [Figure 1b], and neck, consistent with cutaneous sarcoidosis. Laboratory tests indicated microcytic anemia without leucopenia or thrombocytopenia. Ferritin levels decreased to 22 ng/mL. The markers of inflammatory syndrome were slightly reduced (erythrocyte sedimentation rate: 45 mm; C-reactive protein: 8.8 mg/L). Calcemia was within the normal range, and polyclonal hypergammaglobulinemia remained relatively stable at 24.2 g/L. A skin biopsy revealed a non-caseating granuloma, suggestive of sarcoidosis. A CT scan showed an increase in the number and volume of the mediastinal lymph nodes, with splenomegaly measuring 26 cm and hepatomegaly measuring 25 cm. Further investigation revealed an elevated angiotensin-converting enzyme level at 106 U/L (normal range: 20–70 U/L). Given this new information, we discontinued anti-tubercular treatment and confirmed the diagnosis of sarcoidosis. The patient received oral corticosteroids at a dosage of 1 mg/kg/day, resulting in significant clinical and biological improvement within the next few weeks. An abdominal echography performed at six weeks of treatment showed a decrease in spleen and liver size (19 cm for both). A CT scan performed at six months revealed a complete regression of the splenomegaly and hepatomegaly. Informed consent was obtained from the patient.
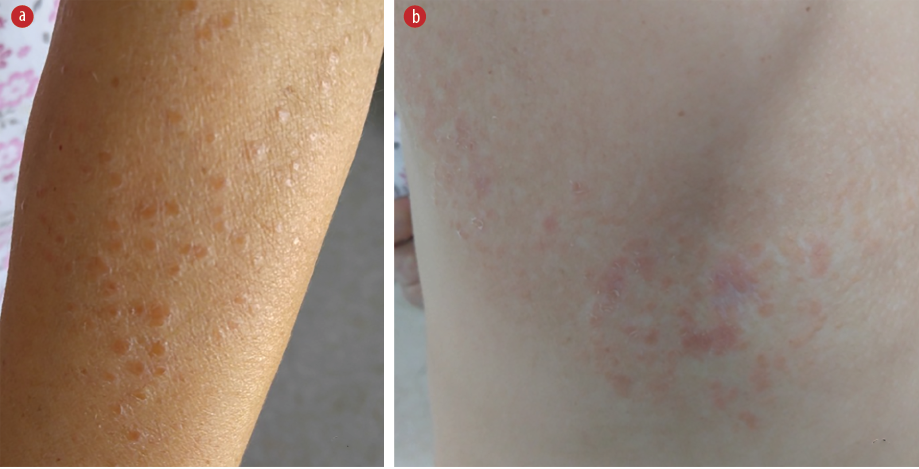 Figure 1: (a) Erythematous maculo-papular lesions on the arms related to cutaneous sarcoidosis.
Figure 1: (a) Erythematous maculo-papular lesions on the arms related to cutaneous sarcoidosis.
(b) Erythematous maculo-papular lesions on the back related to cutaneous sarcoidosis.
Discussion
Sarcoidosis is a chronic granulomatous disease that can affect various organs with varying frequency. Diagnosis relies on three criteria: clinical and radiological presentation, evidence of non-caseating granulomas, and exclusion of alternative disease.2 These criteria underscore the heterogeneity of clinical and radiological manifestations in sarcoidosis, which can mimic a wide range of other granulomatous conditions.
Our case stands out due to prolonged fever in the context of profound deterioration of the patient’s general condition, significant hypercalcemia, and clinical tumor syndrome. Apart from Lofgren syndrome, fever may be present in up to 10% of affected patients, especially in those with extensive involvement of the retroperitoneal lymph nodes, liver, or spleen.3,4 In our patient, the prolonged fever can be attributed to substantial lymph node involvement in the abdominal region, as well as marked hepatomegaly and splenomegaly.
Clinical hepatosplenic involvement is infrequent in sarcoidosis. In some instances, patients may experience left upper abdominal pain along with systemic symptoms such as malaise, fever, fatigue, and weight loss,1 similar to our patient’s presentation. Palpable clinical splenomegaly is found in only 2–42% of cases, and massive splenomegaly extending below the umbilicus, as seen in our case, is rarely described in the literature.1,5 Hypersplenism leading to anemia and thrombocytopenia, as observed in our patient, is also an uncommon finding, as is splenic rupture.1,2,5–7
In our case, the significant hepatomegaly did not coincide with abnormalities in liver function tests and did not provide clear diagnostic guidance.
Although hypercalciuria is a classic sign of sarcoidosis, hypercalcemia is less common, occurring in approximately 5% of cases.8 However, some studies reported a higher incidence of up to 25%.8 Significantly elevated calcium levels, as observed in our patient, are exceptionally rare.9
In our scenario, a lymph node biopsy ruled out malignancy, and tuberculosis remained the primary differential diagnosis. Given the high prevalence of tuberculosis in our region and the concomitant hypercalcemia, anti-tubercular treatment was initiated.10
The lack of response to anti-tubercular treatment and the appearance of cutaneous sarcoids supported the diagnosis of sarcoidosis, leading to the initiation of appropriate treatment with corticosteroids. The favorable response to corticosteroid therapy provided strong evidence confirming the diagnosis of sarcoidosis.
Conclusion
While sarcoidosis is not a common cause of prolonged fever associated with severe hypercalcemia and a clinical tumor syndrome, it should be considered when non-caseating granulomas are present after the exclusion of tuberculosis.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Giovinale M, Fonnesu C, Soriano A, Cerquaglia C, Curigliano V, Verrecchia E, et al. Atypical sarcoidosis: case reports and review of the literature. Eur Rev Med Pharmacol Sci 2009 Mar;13(Suppl 1):37-44.
- 2. Valeyre D, Prasse A, Nunes H, Uzunhan Y, Brillet PY, Müller-Quernheim J. Sarcoidosis. Lancet 2014 Mar;383(9923):1155-1167.
- 3. DeRemee RA. Sarcoidosis. Mayo Clin Proc 1995 Feb;70(2):177-181.
- 4. Madaule S, Lauque D, Sailler L, Arlet P, Carles P. [Splenomegaly in sarcoidosis: clinical features and outcome. Analysis of 17 cases]. Rev Med Interne 2004 May;25(5):348-356.
- 5. Zaarour M, Weerasinghe C, Moussaly E, Hussein S, Atallah JP. “The great mimicker”: an unusual etiology of cytopenia, diffuse lymphadenopathy, and massive splenomegaly. Case Rep Med 2015;2015:637965.
- 6. Pavlović-Popović Z, Zarić B, Kosjerina Z, Petrović D. Splenomegaly in sarcoidosis: frequency, treatment, prognosis and long-term follow up. Srp Arh Celok Lek 2015;143(5-6):279-283.
- 7. Paul S, Gupta V, Gonsalves WI, Kochuparambil ST, Gangat N. Sarcoidosis presenting with pancytopenia. Am J Med 2014 Sep;127(9):e9-e10.
- 8. Baughman RP, Papanikolaou I. Current concepts regarding calcium metabolism and bone health in sarcoidosis. Curr Opin Pulm Med 2017 Sep;23(5):476-481.
- 9. Romine PE, Eaton KD, Paulson KG, Hadi R, Paauw DS. Sarcoidosis presenting as isolated anasarca and hypercalcemia. Am J Med 2019 Jan;132(1):e13-e14.
- 10. Wada T, Hanibuchi M, Saijo A. Acute hypercalcemia and hypervitaminosis D associated with pulmonary tuberculosis in an elderly patient: a case report and review of the literature. J Med Invest 2019;66(3.4):351-354.