Hemangiolymphangioma is a rare type of venolymphatic vascular malformation containing a network of blood vessels and lymphatics.1,2 This condition presents on the body surface of infants and young children and is extremely rare in adults.3 In adults, most cases of hemangiolymphangioma occur in the head and neck, while a few have been reported in the pancreas,4 spleen,5 small intestine,6 rectum,7 chest wall,8 and extremities.9 To date, nine cases of small bowel hemangiolymphangioma have been reported worldwide.2 Here, we report a small bowel mesentery hemangiolymphangioma case with characteristic imaging features that differentiate it from other more sinister conditions.
Case Report
A 23-year-old woman presented with a five-day history of intermittent generalized colicky abdominal pain, constipation, and vomiting. Six years earlier, she had undergone a laparoscopic appendectomy. An abdominal examination showed a tense abdomen with diffuse tenderness. Laboratory investigations revealed hemoglobin of 10.8 g/dL, erythrocyte sedimentation rate of 58 mm/h, and C-reactive protein of 83 mg/dL. Other blood tests, tumor markers (human chorionic gonadotropin, cancer antigen (CA) 15-3, CA 19-9, CA 125, carcinoembryonic antigen, alpha-fetoprotein), and microbiological tests (tuberculosis, HIV, hepatitis B/C) yielded normal results. Initial bedside B-mode ultrasonography showed cysts anterior to the uterus.
A contrast-enhanced abdominopelvic computed tomography (CT) image showed extensive mesenteric involvement by soft tissue masses and several widespread fluid-attenuation cystic lesions of variable sizes, the largest of which measured 5.0 × 4.6 cm with adjacent nodular calcifications and was located in the left upper quadrant. The lesions were engulfing the mesenteric vasculature, which was attenuated but patent. There were alternating areas of the small bowel narrowing and dilatation with mural hyperenhancement within the engulfed segments. Mild segmental dilatation of the proximal jejunal loops was noted, reaching up to 3.3 cm in diameter with associated mild diffuse wall thickening and enhancement of the proximal non-dilated jejunal loops reaching up to 0.6 cm in thickness. A few scattered calcific foci were identified within the cystic lesions. There were multiple prominent mesenteric lymph nodes, the largest measuring 0.8 cm in the short axis [Figure 1]. The CT findings were initially thought to represent possible secondary mesenteric and peritoneal metastatic deposits. However, no primary tumor was identified.
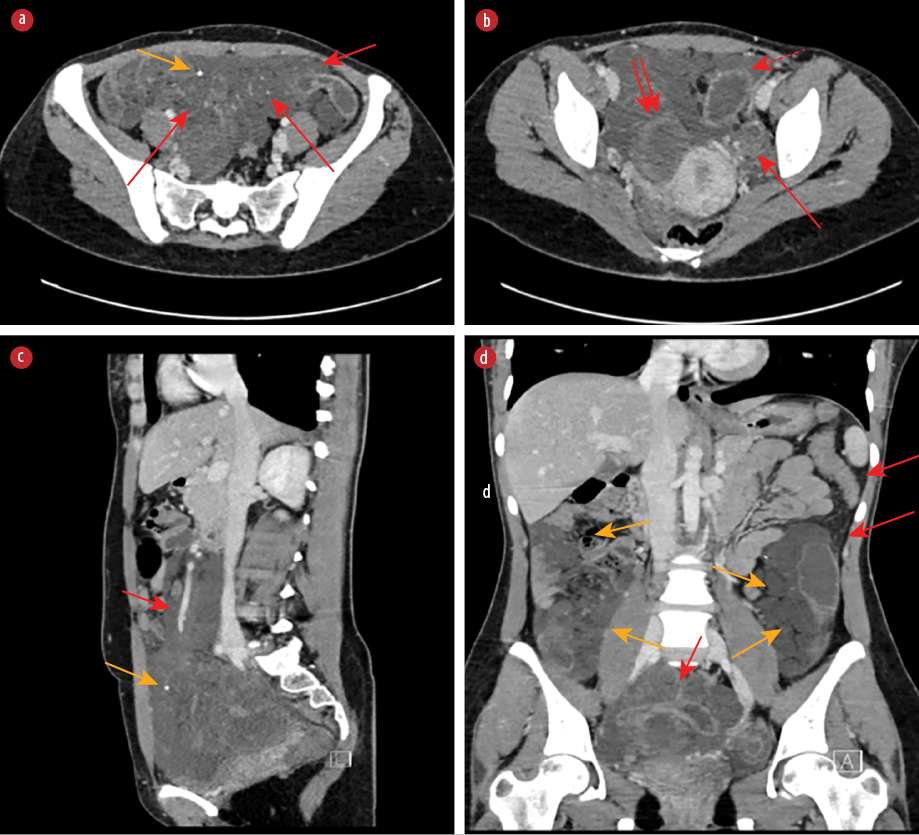 Figure 1: CT image with intravenous contrast in the portal venous phase images. (a) Axial image showing soft tissue densities engulfing the mesenteric vascular branches (long red arrows), with adjacent nodular calcifications (yellow arrow) and the small bowel narrowing (short red arrow). (b) Axial image showing hemorrhagic cyst (double arrow) with a dilated small bowel segment proximal to the hemorrhagic cyst (dotted red arrow) and normal left ovary (long red arrow). (c) Sagittal images showing the distribution of the abnormality within the lower half of the abdomen with sparing of the upper half with encasement of the patent superior mesenteric vein without luminal narrowing (short red arrow) and calcific focus (yellow arrow). (d) Coronal image showing distribution of the cystic changes along the mesentery (yellow arrows) with relative sparing of the peritoneal regions (long red arrows) and compression of the ileal loop resulting in partial low-grade small bowel obstruction (short red arrow).
Figure 1: CT image with intravenous contrast in the portal venous phase images. (a) Axial image showing soft tissue densities engulfing the mesenteric vascular branches (long red arrows), with adjacent nodular calcifications (yellow arrow) and the small bowel narrowing (short red arrow). (b) Axial image showing hemorrhagic cyst (double arrow) with a dilated small bowel segment proximal to the hemorrhagic cyst (dotted red arrow) and normal left ovary (long red arrow). (c) Sagittal images showing the distribution of the abnormality within the lower half of the abdomen with sparing of the upper half with encasement of the patent superior mesenteric vein without luminal narrowing (short red arrow) and calcific focus (yellow arrow). (d) Coronal image showing distribution of the cystic changes along the mesentery (yellow arrows) with relative sparing of the peritoneal regions (long red arrows) and compression of the ileal loop resulting in partial low-grade small bowel obstruction (short red arrow).
Pelvis magnetic resonance imaging confirmed the presence of extensive innumerable cystic changes within the small bowel mesentery, encasing the branches of the superior mesenteric artery and superior mesenteric vein without significant luminal stenosis. The cystic changes demonstrated a hyperintense signal on T2-weighted images and a hypointense signal on T1-weighted images with numerous thin septations. However, one of the cystic lesions within the right side of the pelvis measuring about 4.6 × 3.3 × 3.2 cm showed peripheral T1 hyperintensity and diffuse T2 hypointensity suggestive of hemorrhagic content. That hemorrhagic cystic lesion had a tubular extension superiorly and was compressing one of the distal ileal loops, resulting in partial obstruction of the small intestine. Proximal to this, the small intestinal loops were dilated, up to 3.4 cm in maximum diameter. This was suggested to represent an associated band causing the obstruction. There was a small amount of pelvic free fluid. No definite peritoneal nodules were seen. Apart from thin enhancing septations, no soft tissue masses were identified. In addition, the distribution of the abnormality involved the lower abdomen and pelvis, with relative sparing of the upper abdomen [Figure 2]. Considering the extensive small bowel mesenteric involvement, presence of hemorrhage and calcifications, lack of solid component, and absence of mass effect on the mesenteric vessels despite the large size, it was favored to represent extensive mesenteric lymphangiomatosis.
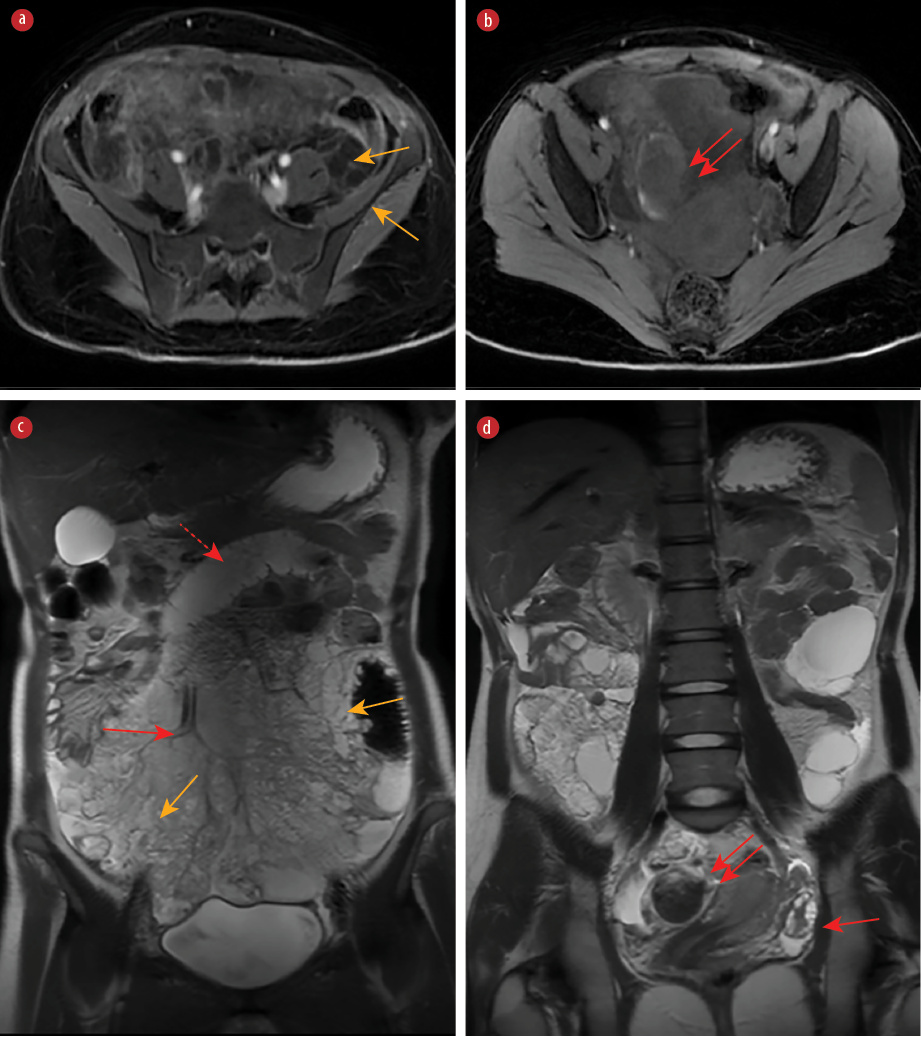 Figure 2: Magnetic resonance imaging images. (a) Axial T1-weighted image post-contrast venous phase showing multiple enhancing septations without solid mass (yellow arrows). (b) Axial T1-weighted image without intravenous contrast showing hyperintense periphery of hemorrhagic component (double arrow).
Figure 2: Magnetic resonance imaging images. (a) Axial T1-weighted image post-contrast venous phase showing multiple enhancing septations without solid mass (yellow arrows). (b) Axial T1-weighted image without intravenous contrast showing hyperintense periphery of hemorrhagic component (double arrow).
(c) Coronal T2-weighted image showing mesenteric hyperintense cysts with variable signal intensity of different locules with numerous thin septations (yellow arrows), normal flow void mesenteric vessels passing through the cystic structures without luminal narrowing (long red arrow), and dilated small bowel (dotted red arrow). (d) Coronal T2-weighted image showing hypointense hemorrhagic cyst (double arrow) and normal left ovary (single red arrow).
A diagnostic laparoscopy with omental and cystic wall biopsy was done. There was hemoserous fluid in the pelvis, left and right paracolic gutters, and between the bowel loops. Multiple clumped cystic lesions arose from the mesentery and omentum and adhered to the small bowel loops. Some of those cysts were filled with serous fluid and others with what appeared grossly to be mucin. There were scattered mucin-like deposits within the mesentery. Peritoneal fluid was aspirated and sent for cytology, microbiology culture, sensitivity, and tuberculosis. Omental and cyst wall biopsies were taken from the deposits. Adhesiolysis was performed, hemostasis was secured, and suction irrigation was performed.
Histological examination of the biopsies revealed omentum with many irregular dilated vascular channels. Most of those vascular channels had a smooth muscle layer in their walls. Immunohistochemically, the lining endothelial cells were positive for CD34 and CD31, while D2-40 was positive in a few thin-walled vessels [Figure 3]. Smears and cell blocks showed reactive mesothelial cells, macrophages, and inflammatory cells. No mucin or malignant cells were seen.
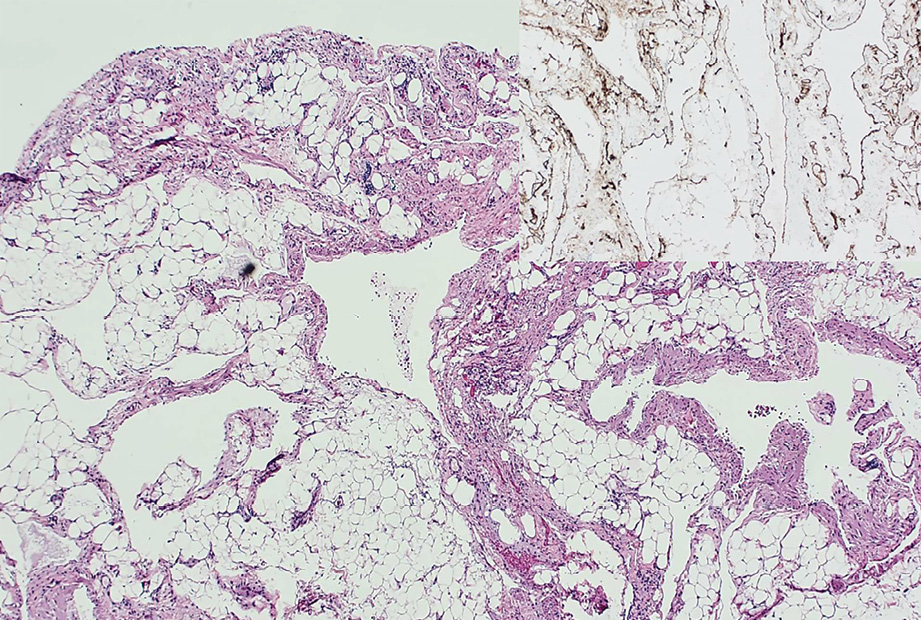 Figure 3: Histological examination shows fibrofatty tissue with dilated irregular vessels, some with prominent smooth muscle layers (hematoxylin and eosin staining, magnification = 40 ×). Inset: positive staining for the vascular marker CD31 in the endothelial cells (magnification = 100 ×).
Figure 3: Histological examination shows fibrofatty tissue with dilated irregular vessels, some with prominent smooth muscle layers (hematoxylin and eosin staining, magnification = 40 ×). Inset: positive staining for the vascular marker CD31 in the endothelial cells (magnification = 100 ×).
The hospital tumor board reached their final diagnosis of hemangiolymphangioma of the small bowel mesentery and noted that due to the extensive involvement of mesentery and peritoneum with a vascular malformation, the tumor was unresectable. Given the patient’s youth and the extreme rarity of her condition, she was referred to a specialized center for a second opinion. An informed consent was obtained from the patient.
Discussion
Hemangiolymphangioma of the small bowel mesentery is extremely rare.10 Our literature search yielded nine cases of hemangiolymphangioma of the small bowel, of which only three cases involved hemangiolymphangioma of the small bowel mesentery.3
Our patient presented with intermittent abdominal pain and signs of small bowel obstruction. Blood results were normal, apart from a mild decrease in hemoglobin and slightly elevated C-reactive protein or erythrocyte sedimentation rate. Several radiological features can help differentiate hemangiolymphangioma of the small bowel mesentery from metastatic deposits in the peritoneum. These findings can aid with the preoperative diagnosis, but they primarily depend on the composition of the cysts and the number of blood vessels in them. First, in nonenhanced abdominal CT, hemangiolymphangioma appears as mesenteric cystic or cystic-solid masses and deposits that are isodense but may show increased enhancement in venous and delayed phases. Enhancement may not be evident if the cystic blood vessels are in a small proportion. Mural and septal enhancement may be present, depending on the thickness of the tissue. Second, these malformed vessels may thrombose and cause necrosis, which might appear like calcium deposits. Calcific foci may overlap with the possibility of mucinous tumors. Third, the lesions may engulf the mesenteric vascular branches without causing a mass effect, so these vessels remain patent. Lastly, on magnetic resonance imaging, T1-weighted images of the cystic lesions appear hypointense, while on T2-weighted images, they appear as homogeneously hyperintense with a thin enhancement of the septations.4,11,12 A useful clue to the diagnosis in our case was the distribution of the abnormality along the small bowel mesentery and the fact that the abnormality was confined to the lower half of the abdomen with a sparing of the upper part. On the other hand, metastatic deposits usually spread along the peritoneum and are distributed throughout the abdominal and pelvic cavity. In addition, isolated mesenteric metastatic deposits are rare without peritoneal involvement.
Hemangiolymphangioma diagnosis needs to be confirmed pathologically as it is a rare condition and because its imaging appearance may overlap with other diagnostic possibilities. The mainstay of treatment is complete surgical resection. Other options include sclerotherapy, laser therapy, cryosurgery, electrocautery, and radium implantation.13 Postoperative follow-up is crucial for early and timely detection of recurrence.14
Conclusion
Hemangiolymphangioma of the small bowel mesentery is an extremely rare entity, makeing it diagnostically challenging. This case report has covered several imaging features that might help clinicians differentiate hemangiolymphangioma of the small bowel mesentery from metastatic deposits in the peritoneum and aid radiologists/clinicians in reaching the correct preoperative diagnosis.
Disclosure
The authors declare no conflicts of interest.
references
- 1. Donnelly LF, Adams DM, Bisset GS III. Vascular malformations and hemangiomas: a practical approach in a multidisciplinary clinic. AJR Am J Roentgenol 2000 Mar;174(3):597-608.
- 2. Lim HJ, Shin KS, Lee JE, You SK, Kim KH. Rare case of large hemolymphangioma in the small bowel mesentery: a case report. J Korean Soc Radiol 2023 Mar;84(2):504-511.
- 3. Du Y, Zhang JN, Zhu LL, Wang Y, Li WP. Haemolymphangioma of the small bowel mesentery in adults: two case reports and a literature review. BMC Gastroenterol 2021 Jul;21(1):273.
- 4. Pan L, Jian-Bo G, Javier PT. CT findings and clinical features of pancreatic hemolymphangioma: a case report and review of the literature. Medicine (Baltimore) 2015 Jan;94(3):e437.
- 5. Mei Y, Peng CJ, Chen L, Li XX, Li WN, Shu DJ, et al. Hemolymphangioma of the spleen: a report of a rare case. World J Gastroenterol 2015 May;21(17):5442-5444.
- 6. Xiao N-J, Ning S-B, Li T, Li B-R, Sun T. Small intestinal hemolymphangioma treated with enteroscopic injection sclerotherapy: a case report and review of literature. World J Gastroenterol 2020 Apr;26(13):1540-1545.
- 7. Chen G, Cui W, Ji XQ, Du JF. Diffuse hemolymphangioma of the rectum: a report of a rare case. World J Gastroenterol 2013 Mar;19(9):1494-1497.
- 8. Zhang X, Sheng X, Liu F, Jian R, Li L, Luo R. Hemolymphangioma of the chest wall: a rare case report. Oncol Lett 2012 Apr;3(4):816-818.
- 9. Kosmidis I, Vlachou M, Koutroufinis A, Filiopoulos K. Hemolymphangioma of the lower extremities in children: two case reports. J Orthop Surg Res 2010 Aug;5(1):56.
- 10. Ohsawa M, Kohashi T, Hihara J, Mukaida H, Kaneko M, Hirabayashi N. A rare case of retroperitoneal hemolymphangioma. Int J Surg Case Rep 2018;51:107-111.
- 11. Li O, Sallam YT, Kwan KF, Qiabi M, Paul NS, Abdelrazek MA. Resection of a large hemorrhagic mediastinal lymphangioma in an adult patient: a radiologic-pathologic correlation. Radiol Cardiothorac Imaging 2022 Feb;4(1):e210043.
- 12. Mao CP, Jin YF, Yang QX, Zhang QJ, Li XH. Radiographic findings of hemolymphangioma in four patients: a case report. Oncol Lett 2018 Jan;15(1):69-74.
- 13. Antonino A, Gragnano E, Sangiuliano N, Rosato A, Maglio M, De Palma M. A very rare case of duodenal hemolymphangioma presenting with iron deficiency anemia. Int J Surg Case Rep 2014;5(3):118-121.
- 14. Zhang D-Y, Lu Z, Ma X, Wang Q-Y, Sun W-L, Wu W, et al. Multiple hemolymphangioma of the visceral organs. Medicine (Baltimore) 2015 Jul;94(27):e1126.