Chilblain lupus erythematosus (CHLE), also known as Hutchinson lupus, is a rare and chronic form of cutaneous lupus erythematosus. It manifests as lesions occurring during cold periods, which tend to be pruritic erythematous to purplish papular, nodular, and/or plaque-tender lesions on the ears, nose, fingers, and toes.1 According to the Mayo Clinic Diagnostic Criteria, the diagnosis is made based on the presence of two major criteria: skin lesions in acral locations induced by exposure to cold or a drop in temperature, and evidence of lupus erythematosus in the skin lesions by histopathologic examination or indirect immunofluorescence study. In addition, there are four minor criteria: coexistence of systemic lupus erythematosus or other skin lesions of discoid lupus erythematosus, response to anti-lupus erythematosus treatment, negative results of cryoglobulin, and cold agglutinin studies.2 To diagnose CHLE, both major criteria and one minor criterion must be met, as was the case in our patient. This report describes the experience of a young man who received multiple initial diagnoses and treatments before being diagnosed with CHLE.
Case Report
A previously healthy 22-year-old Jordanian male began experiencing a scaly rash with peeled-off skin patches involving the fingers and feet in December 2019. This rash was associated with nail changes and bluish-to-purplish discoloration of the toes. The symptoms initially presented mildly, involving the tips of the digits, and gradually progressed to involve the fingers and feet, eventually leading to ulcer formation at the tips of the toes and heels [Figure 1]. Cold exposure triggered the symptoms. The patient had a family history significant for psoriasis in his sister, who was commenced on biologic therapy. He denied recurrent fever, photosensitivity, malar rash, unintentional weight loss, night sweats, history of acute uveitis, scarring alopecia, recurrent oral or genital ulcers, dysphagia, cough, wheezing, hemoptysis, recurrent abdominal pain, heartburn, change in bowel habits, urinary symptoms, numbness or tingling extremities, weakness in extremities, pitting distal ulcers, peripheral joint pain, swelling, or stiffness. On examination, he had warm extremities with slightly dusky to erythematous purple patches on the fingers of both hands and feet. These patches were more prominent bilaterally on the toes and were associated with subungual hyperkeratosis and dystrophic nail changes [Figure 2]. Throughout 2020, he consulted multiple dermatologists. Initially, he was diagnosed with eczema and commenced on topical glucocorticoids, which did not lead to notable improvement. Later, he was diagnosed with a fungal infection, despite negative nail cultures, and prescribed topical glucocorticoids, which did not lead to any notable improvement. Subsequently, he was diagnosed with possible psoriasis and prescribed topical glucocorticoids, without any improvement. In December 2020, he was reevaluated by another dermatologist who referred him to a rheumatologist to rule out an underlying connective tissue disease due to the discoloration of the affected areas.
 Figure 1: Feet before treatment. Red to violaceous pigmented patches around the toes and nails of both feet are associated with superficial ulceration and scarring. The nail plate is partially destroyed in some toenails with subungual hyperkeratosis and petechiae. Nailfold capillaroscopy of the toes showing tortuous capillaries.
Figure 1: Feet before treatment. Red to violaceous pigmented patches around the toes and nails of both feet are associated with superficial ulceration and scarring. The nail plate is partially destroyed in some toenails with subungual hyperkeratosis and petechiae. Nailfold capillaroscopy of the toes showing tortuous capillaries.
 Figure 2: Right thumb before treatment showing a longitudinal wedge-shaped nail overgrowth.
Figure 2: Right thumb before treatment showing a longitudinal wedge-shaped nail overgrowth.
He underwent a skin biopsy of the right toe in December 2020, which showed interface dermatitis with vasculitis-like changes consistent with CHLE [Figure 3]. Laboratory investigations at that time revealed a borderline elevation of the erythrocyte sedimentation rate (29 mm/hr) and a low titer positive immunofluorescence antinuclear antibody (1:80 with nucleolar pattern). Otherwise, the rest of autoimmune work-up was unremarkable, including Sjogren's syndrome A and B antibodies, Smith antibody, topoisomerase 1 antibody, ribonucleoprotein antibody, anticentromere antibody, p- and c-antineutrophil cytoplasmic antibodies, C3, C4, cryoglobulins, antiphospholipid antibody profile, including negative anticardiolipin immunoglobulin (Ig) G and IgM antibodies, beta-2 glycoprotein I IgM and IgG antibodies, and lupus anticoagulant. In January 2021, he was commenced on a tapering dose of glucocorticoids starting at 20 mg with taper of 5 mg per week. He also received hydroxychloroquine 200 mg twice daily, nifedipine 20 mg daily, aspirin 75 mg daily, topical clobetasol cream, tacrolimus ointment, and topical nitroglycerin, resulting in a significant improvement of his skin lesions [Figures 4 and 5]. He continues to follow-up regularly with rheumatology as an outpatient on topical clobetasol cream without needing for oral glucocorticoids.
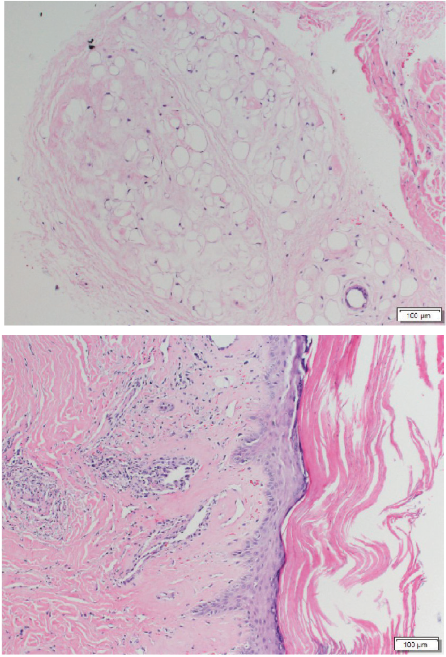 Figure 3: Right toe skin biopsy confirming chilblain lupus. The epidermis shows a thick layer of surface hyperkeratosis with associated keratin plugging of hair follicles. The underlying epidermis is thinned with focal lymphocytic infiltration in the basal layer. There is limited basal hydropic change. The basement membrane zone appears to be mildly thickened. In the underlying dermis, the stroma appears hyalinized in association with a sparse perivascular lymphocytic infiltrate around ectatic dermal vessels and in the intervening stroma. The infiltrate extends to a lesser extent around deep dermal vessels. The subcutis shows adipose tissue with some changes in myxoid degeneration.
Figure 3: Right toe skin biopsy confirming chilblain lupus. The epidermis shows a thick layer of surface hyperkeratosis with associated keratin plugging of hair follicles. The underlying epidermis is thinned with focal lymphocytic infiltration in the basal layer. There is limited basal hydropic change. The basement membrane zone appears to be mildly thickened. In the underlying dermis, the stroma appears hyalinized in association with a sparse perivascular lymphocytic infiltrate around ectatic dermal vessels and in the intervening stroma. The infiltrate extends to a lesser extent around deep dermal vessels. The subcutis shows adipose tissue with some changes in myxoid degeneration.
 Figure 4: A Significant improvement of the lesions of both feet after one year of treatment.
Figure 4: A Significant improvement of the lesions of both feet after one year of treatment.
 Figure 5: The right thumb after treatment. Significant improvement in the previously noted nail changes.
Figure 5: The right thumb after treatment. Significant improvement in the previously noted nail changes.
Discussion
In a review article published in 2008, approximately 70 cases have been reported in the literature, with only a few in the adolescent age group.1 Additionally, no reports were found in the literature regarding CHLE in the Middle East, making our case report the first from the region. This case report emphasized the importance of skin biopsy in establishing the CHLE diagnosis to avoid incorrect diagnoses and unnecessary, potentially harmful treatment. The first-line measures is protecting the acral sites from low temperatures and cold weather to prevent recurrences.1 Other treatment options include topical steroids, which have been shown to be beneficial in up to half of the patients, as well as topical calcineurin inhibitors and calcium channel blockers.1
Conclusion
This case highlighted the importance of skin biopsy in establishing the correct diagnosis of chilblain lupus and avoiding unnecessary treatment, as this disease can be mistaken for several other cutaneous conditions.
Disclosure
The authors declare no conflicts of interest. Informed written consent was obtained from the patient.
References
- 1. Hedrich CM, Fiebig B, Hauck FH, Sallmann S, Hahn G, Pfeiffer C, et al. Chilblain lupus erythematosus–a review of literature. Clin Rheumatol 2008 Aug;27(8):949-954.
- 2. Su WP, Perniciaro C, Rogers RS III, White JW Jr. Chilblain lupus erythematosus (lupus pernio): clinical review of the Mayo Clinic experience and proposal of diagnostic criteria. Cutis 1994 Dec;54(6):395-399.