A previously healthy 13-year-old female patient presented with a nine-month history of weight loss (20% of body weight), lethargy, anorexia, and iron-deficiency anemia. The symptoms were associated with brief intermittent chest pain and palpitations but not with exertional dyspnea or a chronic cough. On examination, she had mild conjunctival pallor. The patient’s weight was 32 kg (below the 3rd percentile), the height was 151 cm (at the 25th percentile), and the body mass index was 14 kg/m2 (below the 3rd percentile). The patient had a resting tachycardia at 120 beats/min, with all other vital signs within normal ranges. Eye examination revealed bilateral intermediate uveitis. Cardiovascular and chest examinations were unremarkable.
Blood investigations revealed a low hemoglobin level of 10 g/dL (reference range = 11–14.5 g/dL) with microcytic hypochromic anemia and an increased red-cell distribution width. The platelet count was high at 800 × 109/L (reference range = 150–450 × 109/L). There was a mildly elevated total white cell count of 18 × 109/L, with a predominant neutrophilia of 12.3 × 109 (reference range = 2.4–9.5 × 109/L). The eosinophil count was also elevated at 1.2 × 109/L (reference range = 0.2–0.8 × 109/L). She had elevated C-reactive protein and erythrocyte sedimentation rate levels of 7 mg/L (reference range = 0–5 mg/L) and 32 mm/hour, respectively. Additionally, she had iron-deficiency anemia, low vitamin D levels of 9 ng/mL (reference range = 50–100 ng/mL), and normal vitamin B12 and folate levels. Albumin levels were low at 26 g/L (reference range = 38–54 g/L), with normal liver transaminases.
The patient underwent esophagogastroduod-enoscopy and colonoscopy. The esophagogastro-duodenoscopy was normal, but colonoscopy revealed moderate pancolitis involving the left side of the colon. Histological examination of a colonic biopsy was consistent with ulcerative colitis. Magnetic resonance enterography showed a mild circumferential mural thickening with hyperenhancement of the left colon. However, the visualized lung bases showed a few bilateral nodules. The chest computed tomography (CT) revealed multiple bilateral irregular pulmonary nodules with halo and feeding vessel signs [Figure 1]. Informed consent was obtained from the patient’s father.
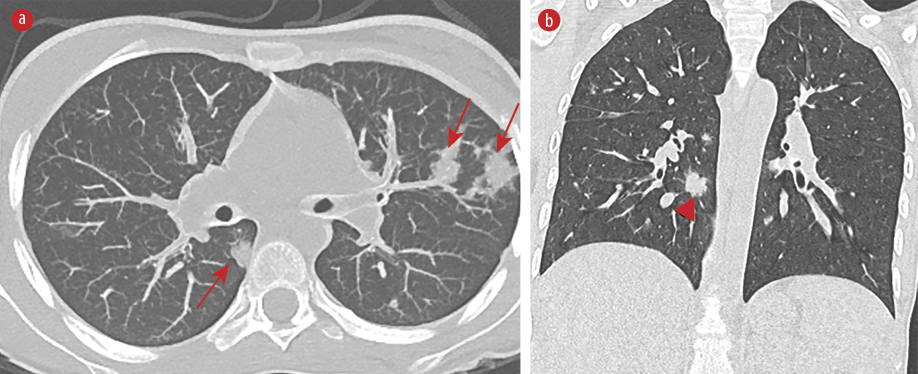 Figure 1: High-resolution CT scan of lungs with (a) axial image showing multiple bilateral nodular opacities, most of which are peripheral and subpleural (red arrows). (b) Coronal image showing nodules with ill-defined borders with ground-glass halo (arrowhead).
Figure 1: High-resolution CT scan of lungs with (a) axial image showing multiple bilateral nodular opacities, most of which are peripheral and subpleural (red arrows). (b) Coronal image showing nodules with ill-defined borders with ground-glass halo (arrowhead).
Questions
- What is the likely diagnosis?
- How would you confirm the diagnosis?
- How would you manage the patient?
Answers
- Extra-intestinal manifestation of inflammatory bowel disease (IBD).
- CT-guided lung biopsy.
- Systemic or inhaled corticosteroids and/or infliximab
Discussion
The nature of these nodules raised concerns about whether they were due to an infectious or inflammatory process, such as systemic vasculitis. Before initiating immunosuppressive therapy, the patient underwent a CT-guided lung biopsy to rule out any infectious causes. Histology of the lungs revealed expanded alveolar spaces filled with fibroblastic plugs formed by spindle-shaped fibroblasts set in a matrix of loose collagen. The inter-alveolar septa were expanded by mixed inflammatory cells in areas showing perivascular accentuation. No fibrinoid necrosis, fibrin thrombi, or granulomas were observed, and the biopsy was negative for fungal organisms. After excluding infectious causes and systemic vasculitis, the lung findings were attributed to a rare extraintestinal manifestation of IBD, suggestive of organizing pneumonia.
The patient was started on oral prednisolone and mesalazine for the IBD. However, the symptoms continued along with elevated inflammatory markers, so an infliximab infusion was initiated, which led to significant clinical and biochemical improvements. Since then, the patient has been on a regular eight-weekly infliximab infusion. A repeated chest CT revealed the resolution of the lung nodules [Figure 2].
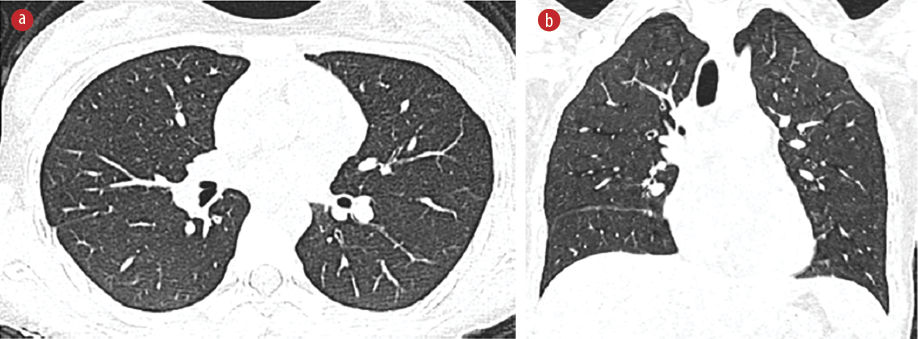 Figure 2: High-resolution CT scan of lungs with (a) axial and (b) coronal images in lung-window settings showing interval resolution of previously seen multifocal lung nodules.
Figure 2: High-resolution CT scan of lungs with (a) axial and (b) coronal images in lung-window settings showing interval resolution of previously seen multifocal lung nodules.
Pediatric IBD (PIBD) is generally classified into three main subcategories: ulcerative colitis (UC), Crohn’s disease (CD), and IBD unclassified.1 Up to 41% of IBD patients may present with extra-intestinal manifestations, including skin manifestations (e.g., erythema nodosum), eye involvement (e.g., anterior uveitis), hepatic manifestations (e.g., autoimmune liver disease and fatty liver), and joint involvement (e.g., arthropathies). However, lung involvement is rare in PIBD.2
The respiratory manifestations of IBD can be classified into airway diseases (including large and small airways), parenchymal lung diseases, thromboembolic diseases, and enteropulmonary fistulas.2,3 Patients with lung involvement may present with clear chest symptoms, or it may be subclinical and detected only by lung function tests or imaging.2 Lung involvement can precede gut symptoms but can occur any time after diagnosis.2,3
Parenchymal lung disease is the most common respiratory manifestation of PIBD and is found more frequently in patients with UC than in CD patients, with a female predominance.2,3 The most common parenchymal lung disease is bronchiolitis obliterans organizing pneumonia, followed by eosinophilic pneumonia and nonspecific interstitial pneumonitis.2
Pulmonary involvement in IBD is likely due to intricate interactions between the gut and lungs, known as the gut-lung axis. The gut and lungs share mucosal immunologic features and a mutual need for microbial homeostasis, suggesting that this cross-talk is mediated by the mucosal immune system’s interaction with the microbiotic environment. Recent studies showed that the alteration of gut microbiota may activate immune cells in the intestinal mucosa, potentially causing an inflammatory response in the lungs when exposed to common allergens.4
Lung involvement is more common in adults with CD; however, few studies have reported such lesions in children with UC. It could be underreported due to decreased awareness and the heterogeneity of clinical presentations.3,5 These patients tend to present with general symptoms, including malaise, fever, arthralgia, and weight loss. Additionally, respiratory symptoms, such as dry cough, shortness of breath, and chest tightness, have been reported.6 Radiological investigations, especially chest CT, play an important role in diagnosing IBD-related lung involvement. IBD-related parenchymal lung diseases respond well to systemic or inhaled corticosteroids, or both, or infliximab.2,3 It is important to rule out other diagnoses with similar radiological manifestations, such as tuberculosis, aspergillosis, or granulomatosis with polyangiitis (Wegener’s granulomatosis).
Early recognition and treatment of pulmonary involvement in IBD are essential to prevent long-term sequelae.
Disclosure
The authors declare no conflicts of interest.
references
- 1. Turner D, Ruemmele FM, Orlanski-Meyer E, Griffiths AM, de Carpi JM, Bronsky J, et al. Management of paediatric ulcerative colitis, part 1: ambulatory care-an evidence-based guideline from European crohn’s and colitis organization and European society of paediatric gastroenterology, hepatology and nutrition. J Pediatr Gastroenterol Nutr 2018 Aug;67(2):257-291.
- 2. Ji XQ, Wang LX, Lu DG. Pulmonary manifestations of inflammatory bowel disease. World J Gastroenterol 2014 Oct;20(37):13501-13511.
- 3. Jochmann A, Trachsel D, Hammer J. Inflammatory bowel disease and the lung in paediatric patients. Breathe (Sheff) 2021 Mar;17(1):200269.
- 4. Ghosh S, Deshwal H, Haraf R, Raju S, Saeedan M, Sarkar P, et al. Pulmonary manifestations of inflammatory bowel disease and treatment strategies. CHEST Pulmonary 2023:100018.
- 5. Pain-Prado E, Rais A, Madhi F, Orzechowski C, Dubern B, Epaud R. Pulmonary and hepatic nodular lesions precede the diagnosis of Crohn’s disease in an 8-year-old girl: a case study and review of the literature. Acta Paediatr 2012 Feb;101(2):e86-e89.
- 6. Majewski S, Piotrowski W. Pulmonary manifestations of inflammatory bowel disease. Arch Med Sci 2015 Dec;11(6):1179-1188.