Successful Revascularization of Near Total Amputation of
the Upper Limb at the Sultan Qaboos Hospital, Salalah
Uday Gokhale, G. Rajasekharan Pillai
ABSTRACT
Severe crush injuries to the upper limb may require a formal amputation with devastating consequences to the patient. We report a patient with a near total amputation at the level of mid-forearm who underwent revascularization and salvage of his hand. The operative details of this case are described. It is the first time that such a patient has been treated successfully by plastic surgeons and orthopedic surgeons at the Sultan Qaboos Hospital, Salalah. Awareness of the possibility of salvage should be spread among health care personnel as well as the need for immediate attention by a multispeciality team. Literature related to the operative technique, contraindications and long term results is reviewed.
From the 1Departments of Plastic Surgery, 2Department of Orthopedics, Sultan Qaboos Hospital, Salalah.
Received: 14 Sep 2008
Accepted: 29 Nov 2008
Address correspondence and reprint requests to: Dr. Vipul Nanda, Senior Specialist, and Head Department of Plastic Surgery, Sultan Qaboos Hospital, Salalah, Sultanate of Oman
E-mail: vipulnanda@rediffmail.com
INTRODUCTION
Replantation is defined as reattachment of the amputated limb using the neurovascular and musculoskeletal structures in order to obtain the recovery of the limb. Revascularization involves all the above steps in a case of limb injury that results in an amputation that is near total.
During the last four decades, technological advances and the use of the microscope have made possible and improved the results of treatment in such injuries. The goal of revascularization after near total traumatic amputation is successful salvage of the limb in both form and function. The decision to attempt salvage in such an injury has evolved and is influenced by many factors, including the importance of the part, level of injury, expected return of function, and mechanism of injury. The absolute contraindications to attempt salvage are existence of associated injuries or preexisting illnesses which preclude a prolonged operation. Relative contraindications include vascular/nerve injuries at multiple levels and patients who are mentally unstable. Success rates are expected to be poor when there is a crush/avulsion injury as compared with a guillotine type of injury.1,2
Functional outcomes following replantation/revascularization vary with the level of injury. Replants of the fingers distal to the flexor superficialis insertion, the hand at the wrist, and the upper extremity at the distal forearm can achieve good function.3,4,5,6,7 The mechanism of injury may be the most predictive variable for success; studies have demonstrated significantly higher success rates with replantations of guillotine versus avulsion amputations.2 Results are better in younger patients.
In this case report, we describe a young male patient with a severe crush injury at the mid forearm level and the successful salvage of his hand by a multispecialty team at SQH, Salalah.
CASE REPORT
A 41-year-old patient sustained an injury when a hydraulic drill machine he was working with caught his sleeve and fell on his forearm. A bandage and splint were applied and he was rushed to the Accident and Emergency (A&E) where he arrived within one hour of the injury. He was conscious, oriented, appeared pale and had a Blood Pressure (BP) of 90/60 mmHg. His right forearm showed evidence of crush injury with obvious fracture of both bones of the forearm. There was a circumferential laceration with loss of volar skin. The muscles of the middle third appeared crushed and discontinuous. The only continuity was in the form of a contused muscle on the ulnar aspect of the forearm which appeared to be the flexor carpi ulnaris. The hand was pale, cold, with no capillary refill and no blood on pinprick. Sensory testing was equivocal. A decision to attempt salvage was taken jointly with the orthopedic team and the consent was obtained from the patient after explaining the pros and cons. The patient was resuscitated,
x-rays were obtained and he was taken up for surgery under
General Anesthisia (GA). X-ray showed fracture of both the radius and the ulna in the middle third and also fracture of the ulnar styloid. (Figure 1)

Figure 1: Preop X-ray showing Fracture BB Forearm and Fracture Ulnar Styloid
The multiple fractures gave an estimate of the severity and extent of injury. The operation involved shortening of both bones by about 3 cm and passing of K-wires by the orthopedic surgeon. (Figure 2 and Figure 3)

Figure 2: Injured forearm after passing K-wires
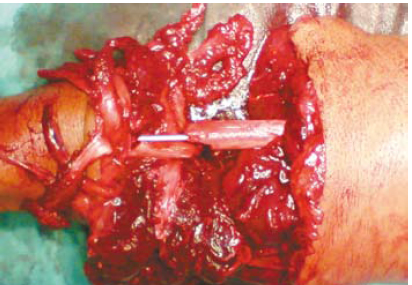
Figure 3: Close-up of Figure 2 showing crush avulsion of the muscles
Thorough debridement of the crushed forearm muscles on the volar and dorsal aspect was done. The incision was extended proximally and distally to identify the neurovascular structures. The radial artery was found discontinuous and the healthy proximal end was found just below the brachial artery bifurcation and distally just above the wrist. A 12-cm vein graft was harvested from the great saphenous vein in the region of the ankle and foot, was reversed and interposed between the radial artery (Figure 4).

Figure 4: Vein graft in situ
A vein in the distal aspect of the forearm was identified, mobilized and anastomosed to the cephalic vein. No other suitable veins could be identified in the distal part. All anastomoses were done with 8-0 nylon under the operating microscope (Zeiss OpMi Vario). The tourniquet was deflated and the return of pink colour, turgor and venous filling confirmed adequate blood flow. The warm ischemia time was estimated to be around six hours. The ulnar artery was continuous, but found contused and thrombosed in its entire length. The ulnar nerve was identified and confirmed to be continuous in its entire length. An attempt was made to identify the median nerve proximally and distally. However, in view of the distortion due to the crush injury, it was postponed for a subsequent stage. A mass closure was done for the muscle bellies on the volar and dorsal aspect of the forearm. The skin was closed and a skin graft applied on the volar aspect.
The patient received low-molecular-weight heparin for five days and antibiotics for seven days postoperatively. His vitals, urine output and hand vascularity were monitored closely. A supplementary skin grafting was done for the residual raw areas under LA after two weeks. The sensations in the ulnar nerve distribution improved gradually. All wounds healed and the patient was discharged after one month. (Figure 5)

Figure 5: Patient at the time of discharge
At six weeks followup, the x-rays showed faint callus formation, grossly normal sensations in the ulnar nerve territory and around 20-degree flexion at the MP joints suggestive of recovering intrinsic muscle function. (Figures 6a and Figure 6b)

Figure 6a: Hand at rest

Figure 6b: Demonstrating active flexion of fingers
He is presently undergoing active and passive physiotherapy to improve range of motion in all small joints of the hand. He has been advised the need for a graft for the median nerve at 3 months and a regular followup to assess for bony union. Further procedures that may be required for the nerve, selective arthrodeses and possible tendon transfers during the next few years have been explained to the patient.
The goal of revascularization after a near-total traumatic amputation is successful salvage of the limb in both form and function. The results of revascularization have improved in the last four decades. This has happened with better understanding of the pathophysiology of the injury, early referral to a trained multispecialty team and better preservation to reduce warm ischemia times, advanced technology available for the surgeon, close monitoring in the postoperative period and a rigorous followup with appropriate secondary procedures.
Various recommendations have crystallized from the
experience in large series. When transferring the patient, ice
placed in plastic bags should be placed in the vicinity of the distal part to reduce warm ischemia time. When the distal part is connected with a small bit of tissue, it may be better to cut it off and the severed part should then be transported carefully. The severed part is to be covered with gauze moistened with saline, kept in a plastic bag and then placed in ice. Direct contact with ice is to be avoided as it may cause frostbite injury.8 Bleeding vessels in the stump should not be clamped and should be managed by compressive dressings and limb elevation.
The upper limits of ischemia times for major injuries from the level of shoulder to the wrist are six hours of warm and 12 hours of cold ischemia, although occasionally success has been reported after longer ischemia times.9-13 Reduction in ischemia time may be achieved by placing a shunt between the proximal and distal vessels while the patient is being prepared for surgery. Complete vascular washout with University of Wisconsin solution at 4oC into the artery has been shown to improve results.14
Preoperative preparation includes fluid resuscitation and warming to prevent vasoconstriction. Incisions are made to identify neurovascular structures which are carefully tagged and protected during the bony manipulations. Bone shortening is recommended to reduce the tension across the neurovascular repairs and for ease of soft tissue closure. Bone should be shortened on the amputated part and not the stump so as to retain the length, should the operation fail. K-wires are placed commonly to fix the fracture.
The arterial flow is assessed after deflating the tourniquet. If the proximal vessel spurt is inadequate, additional vessel shortening may be required. The order of repair of various structures depends on the surgeon’s preference and the specific clinical situation. Most surgeons prefer repairing the dorsal structures followed by the volar structures.2 The arteries may be repaired earlier if the warm ischemia time is unusually long. A vein graft may be harvested from the contralateral arm or leg and should be reversed for arterial interposition. The aim should be to repair at least one artery and two veins.
If a vessel repair lies in hypovascular muscles, it will thrombose within a few days. If a vein graft lies between devascularized muscles, it may even rupture at the anastomosis. Hence, after revascularization, it is essential to observe the vascularity of the muscles and carry out further debridement of muscles, if necessary.15 Muscle in the region of the crush injury may be devitalized and may require further assessment and debridement after 72 hours.
Postoperative care includes adequate fluids and warming the patient’s room to prevent hypotension and vasospasm. There are reports recommending the use of Aspirin, Dextran or Heparin; however, none is backed by a randomized control trial.1,2,16,17 The patient’s hand is monitored closely for signs of arterial insufficiency or venous congestion. Both situations often merit an urgent re-exploration and revision of the affected anastomosis.
During the postoperative period, systemic reperfusion problems may present as myoglobulinuria, tachypnea, and signs of acute respiratory distress syndrome. Amputation in such an eventuality may be life-saving and should be performed as early as possible if the patient shows progressive symptoms of reperfusion syndrome.15
The outcome of surgery has to be assessed not only by the rate of limb survival but also by the functional result and patient acceptability. Most large series are a combination of patients who underwent replantation or revascularization.
In reviewing the large volume retrospective reports, the limb survival rates range from 54% in China’s Sixth People’s Hospital to 82% in North Carolina and 100% in Ogori Daiichi Hospital, Japan.18,19,20 Overall, success rates are significantly higher for replantation of guillotine amputations versus crush amputations.1,2
Long-term outcomes are commonly evaluated using various scoring systems which are based on early professional readaptation, the extent of joint restriction, sensory recovery and muscle power. Lutz reported a series of 64 patients who underwent successful
hand and digit replantation/revascularization for salvage after crush injuries. The average follow-up is around 12 years and secondary procedures are necessary in 45% of the study population.21 Russell et al have published the largest review regarding major limb replantations, and have found that 11 of 24 patients achieved greater than 50% total active motion and 19 of 24 achieved protective sensation. They state that 22 of 24 patients were satisfied with the function and appearance of their replanted part.5
CONCLUSION
The field of revascularization/replantation has become sophisticated over the last four decades. Awareness of the possibility of salvage should be spread among health care personnel as well as the need for immediate attention by a multispecialty team. This will help in reducing ischemia time and thus improve the survival rates and the long-term functional outcomes.
1. O’Brien BM, Miller GD. Digital reattachment and revascularization.J Bone Joint Surg Am 1973; 55:714-724.
2. O’Brien BM. Replantation surgery.Clin Plast Surg 1974; 1:405-426.
3. Brown PW. The rational selection of treatment for upper extremity amputations. Orthop Clin North Am 1981; 12:843-848.
4. May JW Jr, Toth BA, Gardner M. Digital replantation distal to the proximal interphalangeal joint.J Hand Surg (Am) 1982; 7:161-166.
5. Russell RC, O‘Brien BM, Morrison WA, Pamamull G, MacLeod A.The late functional results of upper limb revascularization and replantation.J Hand Surg [Am]1984; 9:623-633.
6. Meyer VE.Hand amputations proximal but close to the wrist joint: prime candidates for reattachment (long-term functional results).J Hand Surg [Am]1985; 10:989-991.
7. Vanstraelen P, Papini RPG, Sykes PJ, Milling MAP.The functional results of hand replantation. The Chepstow experience.J Hand Surg [Br]1993; 18:556-564.
8. Hayhurst JW, O‘Brien BM, Ishida H, Baxter TJ.Experimental digital replantation after prolonged cooling.Hand1974; 6:134-141.
9. May JW.Digit replantation with full survival after 28 hours of cold ischemia.Plast Reconstr Surg1981; 67:566.
10.Chiu HY, Chen MT.Revascularization of digits after thirty-three hours of warm ischemia time: a case report.J Hand Surg [Am]1984; 9:63-67.
11.May JW Jr, Hergrueter CA, Hansen RH.Seven-digit replantation: digit survival after 39 hours of cold ischemia.Plast Reconstr Surg 1986; 78:522-525.
12.Wei FC, Chang YL, Chen HC, Chuang CC. Three successful digital replantations in a patient after 84, 86, and 94 hours of cold ischemia time.Plast Reconstr Surg1988 ; 82:346-350.
13.VanderWilde RS, Wood MB, Su ZG.Hand replantation after 54 hours of cold ischemia: a case report.J Hand Surg [Am] 1992; 17A:217-20.
14.Kour AK, Phone MH, Chia J, Pho RW. A preliminary report of tissue preservation with University of Wisconsin cold storage solution in major limb replantation. Ann Acad Med Singapore. 1995; 24:37-41.
15.Sabapathy SR, Venkatramani H, Bharathi RR, Dheenadhayalan J, Bhat VR, Rajasekaran S. Technical Considerations and Functional Outcome of 22 Major Replantations. Journal of Hand Surgery [Europ] 2007, 32:488-501.
16.Tamai S.Twenty years’ experience of limb replantation: review of 293 upper extremity replants.J Hand Surg [Am] 1982; 7:549-556.
17.Goldner RD, Urbaniak JR.Replantation.In: Green DP, Hotchkiss RN, Pederson WC, Lampert R, eds.Green’s Operative Hand SurgeryVol 1. 4th ed. New York, NY:Churchill Livingstone;1999:1139-1155.18. Replantation of severed fingers. Clinical experiences in 217 cases involving 373 severed fingers.Chin Med J [Engl] 1975; 1:184-196.
19.Tamai S.Digit replantation. Analysis of 163 replantations in an 11 year period.Clin Plast Surg1978; 5:195-209.
20.Hattori Y, Doi K,To S, Oi R. Results of Major Replantation of Upper Extremity. Journal of Japanese Society for Surgery of the Hand [Jap] 2002 18; 6:863-866.
21.Lutz BS, Klauke T, Dietrich FE. Late results after microvascular reconstruction of severe crush and avulsion injuries of the upper extremity. J Reconstr Microsurg 1997; 13:423-429.