Photo-onycholysis is a rare phototoxic reaction, which occurs due to the separation of the nail plate from the nail bed after a drug ingestion and exposure to ultraviolet (UV) light. We have reported the case of a male patient who developed distal onycholysis after receiving 100 mg diclofenac and exposure to UV light. The patient developed tenderness of all fingernails within 12 hours of drug ingestion, which was shortly followed by onycholysis. He improved rapidly on symptomatic treatment. The onycholysis resolved spontaneously within three months without sequelae. Our case is clinically typical to other instances reported in the literature.
Case Report
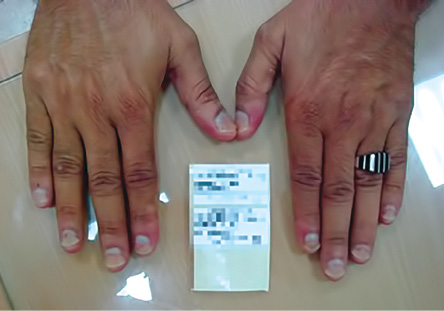
Figure 1: The patient presented with distal, half-moon-shaped onycholysis.

Figure 2: On follow-up, the onycholysis was observed to be resolving spontaneously.
A 46-year-old Omani male, not known to have any dermatological diseases, allergies or photosensitivity was presented to the skin clinic in Salalah with onycholysis of his entire fingernails with sparing of his toenails. The onycholysis occurred during the summer while he was in Muscat.
The patient gave a history of oral intake of 100 mg diclofenac three weeks earlier for the treatment of lower back pain. He took the tablet in the morning and, in the evening, he started to experience painful swellings on all of his fingernails. He consulted a general practitioner who instructed him to stop taking the diclofenac and gave him symptomatic treatment. The swellings had resolved totally within two days and then the patient started to notice the separation of all fingernail plates from nail beds.
Examination of the hands revealed distal half-moon-shaped onycholysis of all fingernails surrounded by a brownish zone [Figure 1]. Skin, hair, and mucous membranes were normal. The routine blood investigation and immune status (complete blood count, liver function test, renal function test, random blood sugar, and HIV test) were normal. Scrapings for fungus from the nail bed and plate in 10% potassium hydroxide preparations were negative. Fungal culture was also sterile. The final diagnosis was drug-induced (diclofenac) photo-onycholysis. The patient was treated symptomatically.
On follow-up, the onycholysis regressed spontaneously [Figure 2]. The patient recovered totally after three months.
Discussion
Our patient presented with onycholysis of all fingernails after taking diclofenac tablets and exposure to ultraviolet A (UVA) radiation. Photo-onycholysis can occur due to loss of nail bed-plate adhesion because of damage to the nail bed epithelium with epidermolysis and/or with formation of hemorrhagic bulla.1
Photo-onycholysis is usually drug-induced, but it might occur in some photosensitivity disorders such as porphyria.2 Porphyria photo-onycholysis occurs due to photosensitization by porphyrin, an endogenous photoactive cutaneous substance in the presence of high-intensity UVA exposure.
The condition often affects fingernails with sparing of the thumb, which is normally less exposed. Toenail involvement is well known among travelers to sunny tropical areas, as their feet are usually uncovered.3 The separation of the nail plate from nail bed usually does not affect the lateral edges of nails.
The most frequently cited drugs that cause photo-onycholysis are tetracyclines, psoralens, and fluoroquinolones.2–7 Medications such as chlorpromazine, chloramphenicol, and oral contraceptive pills may also cause photo-onycholysis but rarely.4
Four patterns of nail detachment from its bed can be seen clinically2:
- Type I: The most commonly found and affects several digits. It appears as a distal half-moon shaped detachment surrounded by a well-demarcated pigmented border, as reported in our patient.
- Type II: Involves only one digit and presents as a proximal circular notch.
- Type III: Affects several digits and changes are located in the central part of the nail bed.
- Type IV: Bullae under the nails. This has been reported following tetracycline hydrochloride as well as in five types of cutaneous porphyria (porphyria cutanea tarda, erythropoietic porphyria, erythropoietic protoporphyria, and variegate porphyria as well as in pseudoporphyria).
Between 3–20% of UV radiation can penetrate normal fingernails. The involvement of the nails while sparing of the skin might be explained by the nails structure as the nail plate may serve as a lens to focus UV energy onto the nail bed.
The natural photoprotection of the nail bed is limited by the absence of melanocytes, stratum granulosum, and sebaceous glands.3 The action spectrum of photo-onycholysis is mostly in the UVA wavelength.8 However, some authors say it is in the UVB range.5 UVB most likely plays a synergistic role in this reaction.9
Exposure to UV light cannot simply reproduce photo-onycholysis.2,7 The pathogenesis is still unknown and to get photo-onycholysis we might need a long period of intense sunlight exposure.10
The drugs most commonly responsible contain ringed structures and include the tetracyclines (particularly doxycycline and demeclocycline), the non-steroidal anti-inflammatory drugs (NSAIDs) (especially propionic acid derivatives), and fluoroquinolones. Additional drugs that can produce phototoxic reactions include amiodarone, psoralens and phenothiazines, anticancer drugs, retinoids, zidovudine, and quinine. In the case of pseudoporphyria, the most likely culprit is naproxen. The photosensitivity of tetracyclines has been reported, and it is due to a phototoxic reaction.11 This photosensitivity is dose dependent, and it differs according to the cyclin molecule. The rate of photo-onycholysis for tetracyclines is as follows: demecycline >doxycycline >tetracycline >minocycline. The phototoxicity of doxycycline is linked to lumidoxycycline, one of its photoproducts.12 When photo-onycholysis is drug induced, it is often associated with a rash, but it can also occur as an isolated phenomenon.11,13
Potentially, all patients can develop phototoxic reactions if enough of a therapeutic dose of an inducing drug and sufficient light irradiation. While there is no need to avoid these drugs completely, precautions should be taken. For drugs with a short half-life, administration of the drug in the evening may be enough to decrease the risk below the clinical threshold for phototoxicity.14 In photo-allergic reactions, only susceptible, sensitized people can develop this reaction after taking a small amount of the drug and exposed to the sun. In these cases, we must avoid these medications.
Photo-onycholysis is usually asymptomatic. However, photo-onycholysis-associated onycholysis has been described in the literature. Photo-onycholysis may accompany but often follows a cutaneous photosensitivity reaction, and usually appears after two or more weeks of drug exposure.
A good history of drug intake is necessary to confirm the diagnosis of drug-induced nail changes. The diagnosis of photo-onycholysis is almost clinical and can be made by exclusion of onycholysis which can be seen in other dermatologic diseases such as fungal infection, lichen planus, psoriasis, histiocytosis, atopic dermatitis, contact dermatitis, ectodermal dysplasia, collagenosis, dysthyroidism, bronchiectasis, yellow nail syndrome, iron deficiency anemia, multiple myeloma, and neoplasia. Local causes of onycholysis include cosmetics, physical agents (e.g. thermal injury), chemicals (prolonged immersion in hot water with alkaline detergents, paint solvents, and gasoline), and trauma.
Treatment of photo-onycholysis is unnecessary, as it disappears spontaneously after discontinuation of the suspected drug and the nails regenerate within three to six months. However, in few severe cases, scarring of the nail bed with consequent nail dystrophy can develop. Patients should clip the affected portion of the nail and keep the nail short. They should also avoid trauma, contact with irritant products and prolonged exposure to water.
Re-ingestion of the offending drug does not necessarily cause a recurrence, as drug intake should be combined with intense sun exposure to induce photo-onycholysis.15
Clinicians must be aware of diclofenac and other drugs known to cause photo-onycholysis and should pay careful attention to any patients prescribed these drugs. Photo-onycholysis is an unwanted side effect; however, it can be self-limiting after stopping the offending drug.16
Conclusion
Drug-induced photo-onycholysis is the result of direct cellular injury following UV radiation-induced activation of a phototoxic agent. All exposed individuals are susceptible to this disorder in the presence of adequate doses of both the agent and radiation. Precaution should be taken when tetracyclines, psoralen, fluoroquinolones, and NSAIDs are prescribed to patients who live in sunny areas or work in the desert, or when doxycycline is prescribed for malaria prophylaxis for travelers to tropical endemic areas.
The patient should be informed about the possible phototoxic reaction that may occur and must be aware of the necessity of protective measures against sun exposure for skin and nails such as the application of sun block and wearing gloves or applying colored varnish on the nails.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Piraccini BM, Tosti A. Drug-induced nail disorders: incidence, management and prognosis. Drug Saf 1999 Sep;21(3):187–201.
- 2. Baran R, Juhlin L. Photoonycholysis. Photodermatol Photoimmunol Photomed 2002 Aug;18(4):202–207.
- 3. Baran R, Juhlin L. Drug-induced photo-onycholysis. Three subtypes identified in a study of 15 cases. J Am Acad Dermatol 1987 Dec;17(6):1012–1016.
- 4. Torras H, Manuel Mascaró J Jr, Mascaró JM. Photo-onycholysis caused by clorazepate dipotassium. J Am Acad Dermatol 1989 Dec;21(6):1304–1305.
- 5. Jeanmougin M, Morel P, Civatte J. Photo-onycholysis induced by doxycycline. Ann Dermatol Venereol 1982;109(2):165–166.
- 6. Carroll LA, Laumann AE. Doxycycline-induced photo-onycholysis. J Drugs Dermatol 2003 Dec;2(6):662–663.
- 7. Baran R, Barthélémy H. [Photo-onycholysis caused by 5-MOP (Psoraderm) and the application of the imputation method of drug effects]. Ann Dermatol Venereol 1990;117(5):367–369.
- 8. Logan RA, Hawk JL. Spontaneous photo-onycholysis. Br J Dermatol 1985 Nov;113(5):605–610.
- 9. Bjellerup M. Medium-wave ultraviolet radiation (UVB) is important in doxycycline phototoxicity. Acta Derm Venereol 1986;66(6):510–514.
- 10. Cavens TR. Onycholysis of the thumbs probably due to a phototoxic reaction from doxycycline. Cutis 1981;27(1):53–54.
- 11. Ibsen HH, Lasthein Andersen B. Photo-onycholysis due to tetracycline-hydrochloride. Acta Derm Venereol 1983;63(6):555–557.
- 12. Shea CR, Olack GA, Morrison H, Chen N, Hasan T. Phototoxicity of lumidoxycycline. J Invest Dermatol 1993 Sep;101(3):329–333.
- 13. Kanwar AJ, Singh OP. Onycholysis secondary to tetracycline hydrochloride. Cutis 1979 May;23(5):657–658.
- 14. Lowe NJ, Fakouhi TD, Stern RS, Bourget T, Roniker B, Swabb EA. Photoreactions with a fluoroquinolone antimicrobial: evening versus morning dosing. Clin Pharmacol Ther 1994 Nov;56(5):587–591.
- 15. Frank SB, Cohen HJ, Minkin W. Photo-onycholysis due to tetracycline hydrochloride and doxycycline. Arch Dermatol 1971 May;103(5):520–521.
- 16. Badri T, Ben Tekaya N, Cherif F, Ben Osman Dhahri A. Photo-onycholysis: two cases induced by doxycycline. Acta Dermatovenerol Alp Pannonica Adriat 2004 Dec;13(4):135–136.