|
Abstract
Objectives: Despite the fact that cesarean delivery does not offer significant health benefits for either mother or newborn, there has been a noticeable upward trend in elective cesarean births in Iran, over the last two decades. This study aims to examine whether knowledge, perception of health threats, efficacy, and personal beliefs act as psychological predictors towards the intention of women to have a normal vaginal delivery.
Methods: The mixed-method approach was used as quantitative and qualitative design. Simultaneously, 290 pregnant women who visited prenatal clinics participated in the study. Quantitative and qualitative data were collected using a structured questionnaire based on Witte’s Extended Parallel Process Model, and four focus groups, respectively.
Results: Women perceived lower personal risk but higher levels of efficacy. Perceived self-efficacy, severity, and response efficacy emerged as significant predictors of intention to experience vaginal birth. The participants’ insufficient knowledge and misconceptions about birth methods were prevalent. Major themes were identified and divided into negative and positive beliefs about vaginal birth.
Conclusion: This educational model is useful for understanding women’s intention to undergo a vaginal birth, especially when it is combined with a qualitative approach. Maternal care providers should acknowledge their clients’ beliefs and intended childbirth methods prior to offering medical intervention.
Keywords: Normal vaginal delivery; Extended Parallel Process Model; mixed methods.
Introduction
Cesarean section (CS) has become an increasingly common surgical procedure and a health concern in many developing countries.1 According to a World Health Organization statement, there is no justification to have a CS rate higher than 10-15%.2 However, this has been the case in most industrialized and developing regions. Research findings show that elective cesarean birth does not decrease maternal mortality rates or offer a significantly better prognosis for newborns.3,4 Conversely, scheduled cesareans increase the probability of late preterm births and neonatal morbidity as the cesarean rate increases from 10% to 20%.3 Increased harm to the mother also should not be discounted.
In Iran, the rising cesarean rate is notable and a large percentage of all cesarean births occur predominantly in first-time pregnant women. Of all deliveries in the country, the CS rate was approximately 38.4% in 2005 and 46% in 2009.5 Despite the success of breast-feeding and family-planning programs over the last two decades, the approach of midwife-assisted childbirth has changed to a medical approach. Although more than 95% of all deliveries take place in hospitals assisted by educated midwives, the childbirth process and midwifery practice happen under the supervision of obstetricians in hospitals, so that medical interventions such as episiotomy, perinea shaving, restricting oral intake, and intravenous lines have become common practices in routine childbirth care. The assistance of a doula is not common, and the presence of a spouse is forbidden in all teaching and most private hospitals. Midwives are the only source of support for women in labor, yet they often engage in many other duties and assist other women in labor. In addition, maternal education is only briefly presented during short prenatal visits in clinics or hospitals.6 Thus it is not surprising that the lack of information and misconceptions of childbirth in an unprepared woman can induce excessive fear and anxiety before labor.
Even though pregnancy and childbirth are auspicious and memorable event in every woman’s life, women tend to argue with professionals, peers, and their family.7 Most Iranian studies have examined the socio-demographic factors or organizational elements related to the rising cesarean trend.8-10 Assessing pregnant women’s beliefs and their understanding of the different modes of childbirth or how different elements may affect their intention to plan childbirth has been limited to a few small quantitative studies in Iran,11-13 but the role of Iranian women in the rising CS rate has not been closely studied.
Like several developed cities in Iran, Shahroud, a populous and developed Northeastern city has confronted rising cesarean birth rates over recent years. Planned cesareans among first-time pregnant women has developed into a major health concern (57.5% in 2010).14 Considering the magnitude of the problem and the fact that beliefs and knowledge of pregnant women about the mode of childbirth and the role of influential factors on their intention to plan the mode of childbirth have never been studied in Shahroud, the present study was conducted to explore the facts by answering the following questions using a quantitative approach: a) What do pregnant women know about the methods of childbirth? b) How do they view the potential risks of a cesarean section delivery for mother and baby? c) Do they perceive themselves as self-confident enough to cope with a normal vaginal delivery (NVD)? d) How do these factors influence their plans for an NVD?
At first, a model for evaluating the individuals’ perceptions toward a specific issue called the Extended Parallel Processing Model (EPPM) was chosen, first proposed by Witte in the early 1990s.15 Since a number of theories ignore the failures as well as successes of participants’ intentions or changes in behavior, an inventory based on a solid theory was needed to evaluate the participants’ intentions to plan NVD; EPPM was useful for this purpose.
In addition, our qualitative objectives were to explore the knowledge and beliefs of expectant mothers about methods of childbirth as the main behavioral change target group that has not been closely studied before. The rational of the mixed-method approach was to develop a more complete understanding of expectant women’s questions and provide detailed information about Iranian women’s beliefs through their quotes and based on their cultural context. The mixed purpose of the present research aimed to determine whether the intention of pregnant women towards NVD can be predicted by EPPM inventory and to identify their salient beliefs towards NVD during pregnancy.
The authors believe that the findings from this study may provide insights into women’s perceptions and understanding of childbirth, what they expect from maternal care during labor and delivery, and how meeting the mother’s needs improves their inclination towards normal childbirth.
Methods
This study incorporated the quantitative and qualitative mixed-methods approach, simultaneously. According to Creswell and Plano Clark (2011), when the intent is to merge concurrent quantitative and qualitative data to address study aims, the investigator combines both quantitative and qualitative research.16 Thus this study was designed as a convergent or parallel design since combining individual and group response formats is one of the best methods for collecting data from a target population about sensitive health issues.17
As mentioned above, the participants’ perceptions of threats and efficacy as the psychological elements were assessed using EPPM to predict their intention towards normal childbirth. Although this model has been used in various health domains,18-22 it is the first time it has been applied to predict pregnant women’s intention to plan the mode of birth.
Briefly, the EPPM helps to predict the outcome in conditions involving fear appeals and whether these fear appeals succeed or fail to motivate people to react as to either accepting or refusing a message of health concern. The EPPM explains both successes and failures of fear appeals, and fear is reincorporated as a central variable in the model. According to the EPPM, the evaluation of a fear appeal initiates two appraisals of the message (a threat appraisal and an efficacy appraisal), rejection (individuals assessment of the threat as an issue of insignificance), fear control (audience is scared but act in such a way as to reduce the fear) and acceptance of the message (when the threat is believed to be serious, but motivates the individual to control the danger of the threat).23 In short, recommendations pertaining to a health risk message are accepted when danger control dominates and it is rejected when fear control dominates. (Fig. 1)
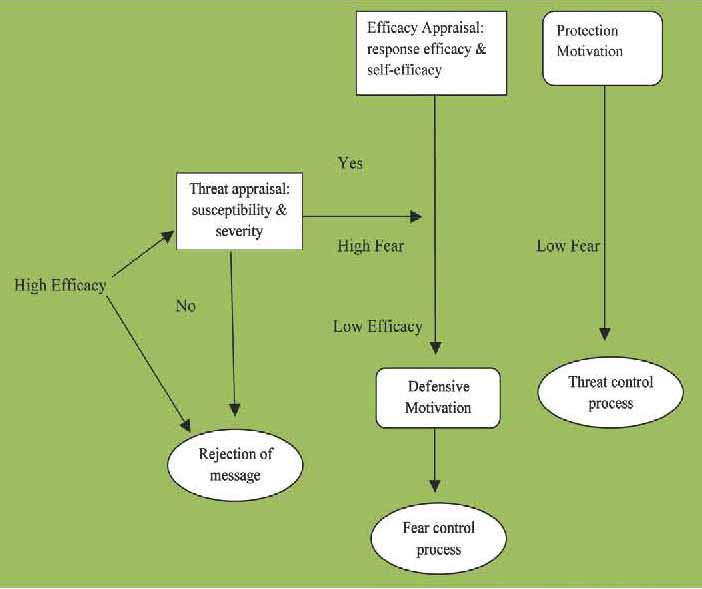
Figure 1: Simple Description of Witte’s Extended Parallel Process Model for fear appeals (according to Wite, 2001).
The participants were a sample of pregnant Iranian women living in Shahroud who attended prenatal care clinics affiliated with Shahroud University of Medical Sciences. Six clinics were selected from different points of the city. First, using the clinics’ maternal health lists, women who met the inclusion criteria of the study were recruited. The goals of the study were described to the women, and willing participants entered into the study and completed the structured questionnaires after giving written informed consent. The questionnaires were self-completed in a private room in the clinic. The inclusion criteria consisted of patients with low-risk pregnancy, aged between 18 and 40 years, with a gestational age of at least 18 weeks or more, who were able to read and write in Persian, with singleton pregnancy and negative history of previous cesarean section or any diagnosed prohibition of vaginal delivery.
As vaginal birth after cesarean surgery (VBAC) is not performed in Shahroud and many other cities of Iran, women with previous CS were not included in the study. Participants had the right to refuse or withdraw at any time and were assured of the confidentiality of the collected data. Data were gathered from December 2010 to March 2011.
In most EPPM studies by Witte, effect sizes ranged from medium to very large and to meet conventional standards of 0.80 power with alpha = 0.05, 29 participants per group were needed for attitudes, 38 participants were needed per group for intentions, and 26 participants were needed per group for behaviors. To test the relationship between EPPM constructs, at least 150 participants were needed to test the relationship between them.23 Since only the participants’ perception of threat and efficacy, knowledge and intentions (but not behaviors) were assessed, and considering the attrition rate of 10%, the initial sample size was determined to be 350 persons. However, 290 women completed the questionnaires without missing data giving a response rate of 83%. To develop a comprehensive understanding of the mothers’ knowledge and beliefs towards childbirth, a purposeful sub-sample of women were recruited from among the 290 women into the qualitative section of study. It was estimated that a sample of 15 to 20 participants would be needed to reach saturation. Maximum variation sampling was used to recruit a group of pregnant women whose age ranged from 18 to 32 years, first time pregnant (10), house wife (9) and the rest were second time pregnant (7), employed (5) and students (3). In total, 17 pregnant women took part in four separate focus group discussions (FGD). The study design of both the qualitative and quantitative approaches is illustrated in Fig. 2.
Discussions were undertaken in a large, quiet room at the clinics and at a time most convenient for the participants. Two researchers conducted the focus groups. One researcher, as the facilitator, led the focus group discussion and one observer took notes and audio taped the session. Participants were ensured anonymity and were provided snacks during the discussion. In all of the focus groups, mothers stated common viewpoints and there appeared to be no peer pressure.
At the beginning of each FGD, the facilitator introduced the objectives of the study and began the discussion with a semi –structured question such as: How much do you know about methods of childbirth (normal childbirth and cesarean birth) and their benefits or risks? Then, focusing on each of the expressed response, the facilitator proceeded with the questioning to explore the women’s beliefs toward vaginal delivery. Examples of interview questions included: What are your beliefs about normal childbirth? Why do some women request a cesarean without a medical necessity? What are effective strategies to make a normal birth more preferable?
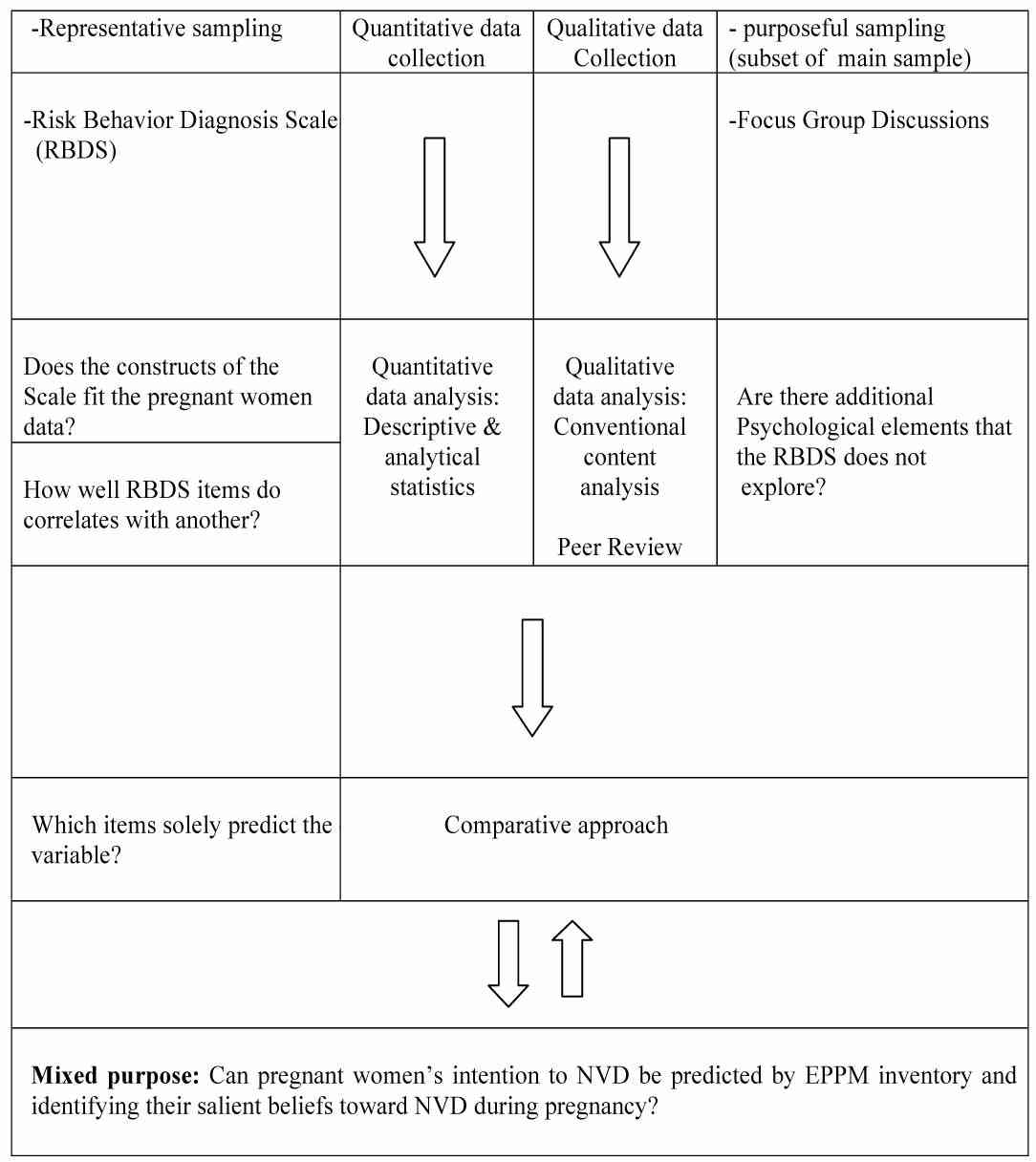
Figure 2: Study design and data analysis of the EPPM prediction for intention to NVD.
Depending on the responses, probing questions such as, "What do you mean?" "Why?" "Please explain more", were asked to find out the depth of the women’s perceptions and beliefs. Sampling was continued until data saturation was achieved and no new information or codes obtained in the data occurred at the 4th FGD. The discussions lasted 45-60 minutes.
Qualitative discussions were audio-taped and all tapes transcribed verbatim. Conventional content analysis was used to analyze all FGDs and field notes. The advantage of a conventional approach is the ability to gather data directly from study participants without imposing pre-conceived categories and previous theoretical perspectives.24 Key terms in the text were highlighted and then key phrases were reinstated. Labels were attached to key phrases and after coding, phrases reduced to clusters. The analysis was performed by separating and coding words relevant to the research question. The codes were classified into main categories and subcategories on the basis of differences and similarities. The whole text was thoroughly reviewed several times by the authors, and after obtaining consensus among them, three categories were identified. To increase the credibility of data, the text of the discussions was given to two external researchers who were not involved in the present study, who were requested to read them and check the accuracy of the coding process.
At the time of the study, no exact scale to measure perceptions of pregnant women towards the mode of delivery based on EPPM was available. Therefore, a structured inventory was designed to identify whether our participants were in fear control or in danger control process. The Risk Behavior Diagnosis Scale (RBD Scale) is a 12-item survey theoretically grounded in the EPPM. The original scale asks three basic questions/phrases each about perceptions of susceptibility, severity, response efficacy, and self-efficacy on a seven point scale ranging from" 1-strongly disagree" to "7-strongly agree." By means of quantitative analysis of the answer scores, what the participants’ perceptions of threat and efficacy will be determined. This has been used in different health topics and populations and has yielded reliable and valid responses.19,23
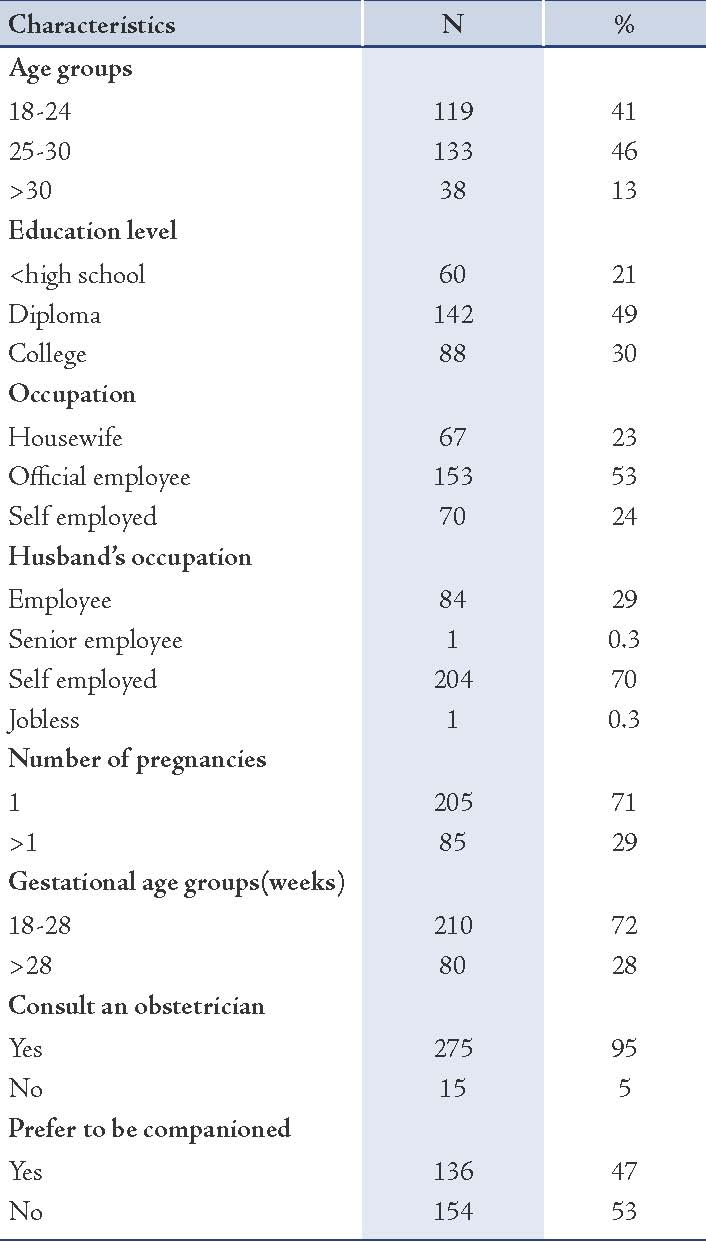
The study inventory consisted of two separate parts used to measure the data: Demographic (Table 1), and RBD items. The RBD scale was used to assess each participant’s perceptions of threat (susceptibility to and severity of common complications of unnecessary cesarean) and efficacy (their responses to the effectiveness of the recommended messages and self-efficacy).
Table 1: Patient characteristics.
The variables "susceptibility" and "severity" were assessed using five phrases for each domain with seven-point Likert-type scales (e.g., "I am more likely to experience major infections after cesarean delivery"). Higher scores indicated greater perception of vulnerability to cesarean side effects. The responses "efficacy" and "self efficacy" variables were measured by six and seven statements, respectively, in the same above-mentioned manner.
The participants’ knowledge related to childbirth was assessed using nine questions, with "true," "false," and "don’t know" answers. A correct answer was rated as 1 and incorrect or "don’t know "answers rated as 0. This was expressly designed for the study based on the literature and research objectives. At the end of the questionnaire, five items were considered to assess the intention towards vaginal birth using seven-point Likert-type scales (e.g., "I intend to learn pain control skills to use them in my vaginal birth"). To avoid affirmation bias, a combination of positively and negatively worded questions/statements was presented in the scales.
To examine the content validity in this step, professional subjective judgment was required to determine the extent to which the scale was designed to measure the considered variables.25 For this purpose, inclusion of at least five to 10 experts was useful to review and judge the appropriateness of items to the domain of content represented in the questionnaire using content validity index (CVI).26 The group members consisted of nine experienced staff specializing in the related subject of study. The less conservative approach was used to test the total agreement degree (e.g., 80% of experts should rate 3 or 4 for each item). Hence, seven out of nine experts’ ratings were required to be 3 or 4, for a minimum item CVI score of 0.78 for each item. Items that did not have at least CVI 0.78 were discarded and the rest were amended. In the next step, to improve clarity, the remaining questions were given to 25 pregnant women from two clinics using convenience sampling. However, few revisions were conducted. Finally, the internal consistency of the EPPM inventory was tested using Cronbach’s alpha and correlation. Reliability coefficient of 0.75 seemed to be sufficient for a new scale.27 For this purpose, the inventory was given to 50 pregnant women with different socioeconomic characteristics. Cronbach’s α coefficients were 0.71, 0.76, 0.78, 0.70, 0.69 and 0.81 for susceptibility, severity, response efficacy, self-efficacy, knowledge and intention subscales, respectively. Ethical approval was obtained from the Ethics Committee at Shahroud University of Medical Sciences on February 15, 2011.
After receiving ethical approval from the Ethics Committee, the researcher identified eight midwives in target settings and trained them for recruitment of the eligible test subjects and data collection. The recruitment standards included the following: 1) All participants were assured that their responses would be maintained in strict confidence; 2) All participants were informed and confirmed that their participation was voluntary and that they could withdraw at any time; and 3) Any participant who required emergency care would be referred to emergency obstetrics services immediately.
Primary data analysis was conducted to determine whether participants were engaged in danger control or fear control. The threat score (sum of perceived severity and susceptibility scores) was subtracted from the efficacy score (sum of perceived response efficacy and self-efficacy scores) to calculate the discriminating value. Also, descriptive statistics were developed for numerical data. Various analytical tests were used to assessed the correlations of the questionnaire’s components to one another and with obstetrics - socioeconomic variables using correlation coefficients, independent samples t-test, Man-Whitney-U test, one-way ANOVA, and x2. Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) version 15.0. Furthermore, linear regression analysis was used to determine the intention to deliver vaginally.
Results
Quantitative data revealed that the sample consisted of 290 first-time pregnant women, which represented 83% of those who consented to participate in the study. Most were 25 years old and younger (52%). The average gestational age of the study population was 25 ± 5 weeks. Nearly half of the women had high school education and almost all were housewives (93%). Also, most participants had monthly appointments with an obstetrician during pregnancy, along with the routine prenatal care at health centers (95%). Table 1 outlines the sample characteristics.
Approximately half of the participants had moderate knowledge of the risks and benefits of each mode of childbirth. A two-sample independent t-test revealed a significant statistical difference between the number of pregnancies and self-efficacy (CI 95%: 3.19-4.81; p<0.001) and knowledge (CI 95%: 0.91-2.01; p<0.008). Using one-way ANOVA, statistically significant increase was found for knowledge, perceived susceptibility, and perceived severity based on the level of education (p<0.001). Also, women with previous pregnancies had a significantly lower probability of having an attendant (e.g., family member, doula, etc.) during labor than first-time mothers (p<0.001). On the other hand, first-time mothers and women who preferred to be accompanied by an attendant during labor exhibited lower self-efficacy compared with women who had given birth at least once (CI 95%: 2.31-3.1).
Moreover, older participants had a higher level of knowledge (p<0.07), response efficacy, and self-efficacy (p<0.001). Around 79% of women indicated a strong intention to have a vaginal birth. Table 2 shows the mean and dispersion of the EPPM variable scores. There was no statistically significant difference between the EPPM variables and any of the following using x2: occupation, gestational age, spouse’s education, or spouse’s occupation.
Table 2: Range, mean and standard deviation of the EPPM scale.
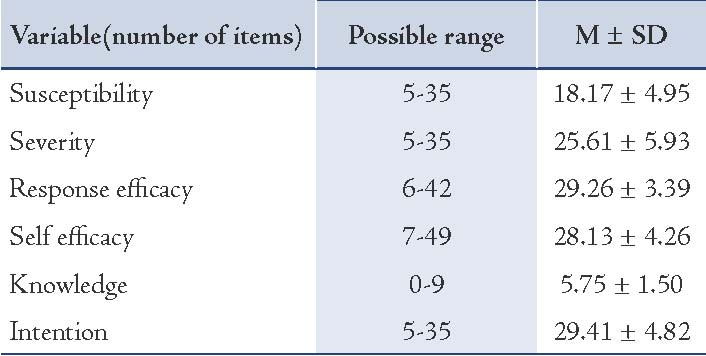
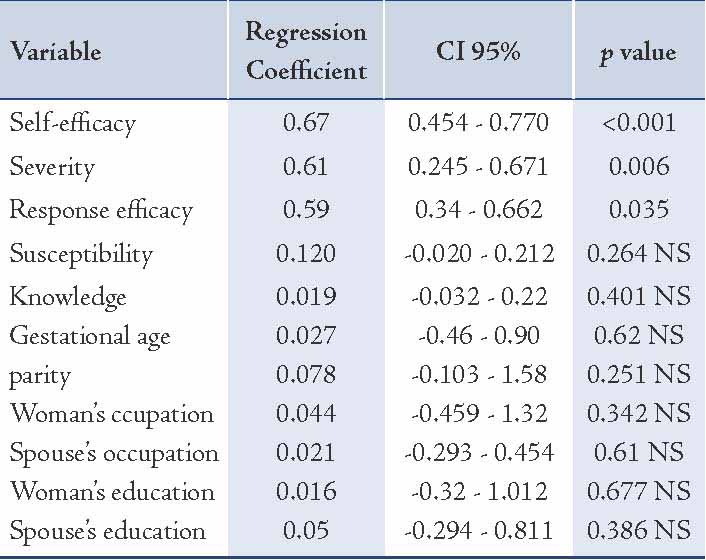
Lastly, the main items of the questionnaire were entered into a linear regression analysis in a stepwise method - as independent variables - to be tested as predictors of intention to deliver vaginally. Variance of inflation factors were calculated for each item and showed that collinearity was not an issue within the model. The variables "perceived self-efficacy", "perceived severity", and "perceived response efficacy" were identified as the main predictors of intention towards having normal birth, whereas, perceived susceptibility and the level of knowledge on mother’s intention to deliver vaginally were not statistically significant after adjusting for probable confounders such as gestational age, number of pregnancies, occupation and the level of education of the women and their spouses. In other words, women with perceived higher self-efficacy, perceived response-efficacy, and perceived severity were more likely to plan a vaginal birth (Table 3). This model predicted 44% of the variance in vaginal delivery intention.
Data saturation and repetition of qualitative data was achieved through four focus group discussions with the participation of 17 pregnant women. At first, the participants’ knowledge was assessed to gain insight into their attitudes and beliefs. Women who had one or more previous pregnancies were more likely to be aware of common maternal indications of CS and risks or benefits of the methods of childbirth compared with first-time pregnant mothers. However, nearly all participants knew that CS (specifically with general anesthesia) may delay the initiation of the newborn’s attachment to the mother, delay breast feeding, and restrict the mother’s activities in the first few days following surgery. Nevertheless, most women thought it was unlikely that they would face undesirable outcomes following cesarean surgery.
Table 3: Results of linear regression analysis in determining the intention to vaginal delivery.
A total of 28 codes and three subcategories were extracted and classified into two main categories: "positive beliefs toward childbirth" and "negative beliefs toward childbirth." These categories are presented separately for ease of discussion. (Fig. 3)
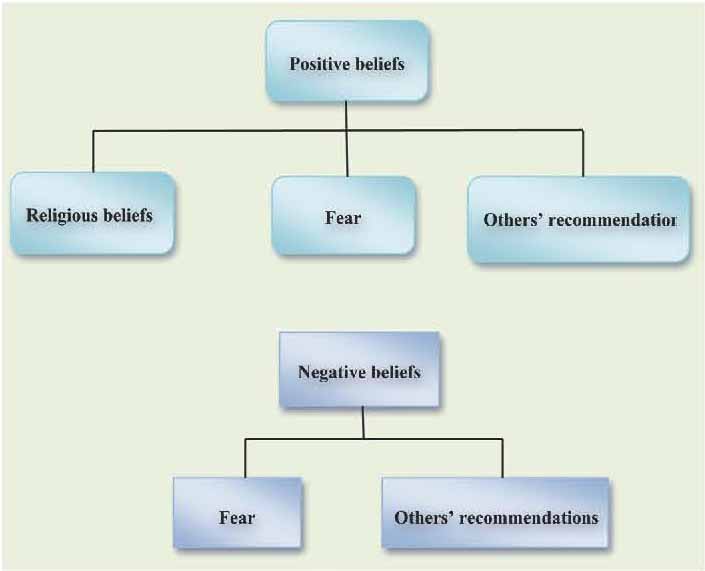
Figure 3: Beliefs toward normal vaginal birth according to focus groups discussion.
Positive beliefs
Beliefs toward NVD appeared more positive than negative. Positive beliefs toward NVD were categorized into "religious beliefs," "fear," and "others’ recommendation." One main subcategory derived from data analysis of the beliefs in the women centered on religious beliefs, which were frequently expressed by the participants. The data showed that faith in the Lord and religious tenets played an important role in the women’s behavior and decision-making. The following are some of the religious sentiments expressed by participants: a participant aged 33 years old (second pregnancy) commented that, "Childbirth is a natural process of creation that the Lord fore ordains"; while a participant aged 22 years old (first pregnancy) declared that, "Childbirth pain sanctifies a woman from the guilt"; and 27-year-old woman (second pregnancy) affirmed that "Praying and seeking help from God and the saints give me power and enable me to endure labor pain."
Fear of CS was a common concern among participants and was considered an important cause of women’s inclination towards NVD. Some statements from the participants included: One participant (first pregnancy, 25 years) stated that "It (CS) is a surgery per se and has its own risks"; while a 21-year-old participant (first pregnancy) expressed that, "Whenever I think about the cesarean birth, I remember the operating room, unconsciousness, pain and bleeding. I have thought several times about the consequences of this surgery, specially the abdominal wound after cesarean delivery." Hence, several participants indicated that they were fearful because the painful operation would prevent them from doing their work and looking after the child.
Most mothers shared the view that "others’ recommendations" in planning a normal childbirth was the most powerful factor in their plans for a vaginal childbirth. "Others" referred to friends, physician, spouse, and family (mainly the pregnant woman’s mother). A few women declared that the mode of birth was primarily recommended by their obstetrician as a safe method either for the mother or the baby. One woman said, "I believe in my doctor’s decision. She advised me to give birth normally. Whenever she reassures me that everything is OK, I rely on her" (first pregnancy, 32 years).
In particular, the recommendation of the woman’s mother or mother-in-law had a significant impact on the participant’s beliefs towards childbirth. A participant aged 23 years old (first pregnancy) stated that "My mother had two births, one difficult normal birth and one cesarean. Yet she always advises me to give birth as naturally as possible because of her awful experience after surgery." For many women (particularly very young mothers), a spouse’s recommendation was also a factor in planning a vaginal delivery.
Negative beliefs
Although negative statements towards vaginal birth were discussed, there were only a few negative views that appeared to be important. Negative beliefs were classified into two subcategories: "fear" and "others’ recommendation."
Vaginal childbirth-related fear described by the mothers had multiple dimensions that are captured in four sub themes: fear of labor pain, fear of being alone during labor, fear of jeopardizing the baby’s health, and fear of genital tract damage. Fear of labor pain was a sub-theme that formed a major segment of the women’s concerns and was frequently expressed, especially by first-time mothers. A feeling of incapability, lack of accessibility to pain relief, and fear of death from excessive pain were expressed by the test subjects. However, pregnant mothers who had previously given birth described their results from previous birth experience and felt their fears were justifiable because of labor ward environment. For instance, one participant (second pregnancy, 28 years) stated that "I did not get any pain relief or sedative (during previous childbirth), my pain intensified after labor progressed and my water broke. I felt feverish and asked for water or juice but I was not allowed to drink and I was only fed by serum (IV hydration)."
Fear of being alone during birth encompassed feelings of loneliness, being ignored by care providers, and feelings of helplessness, which were common fears expressed by the test subjects. One participant aged 34 years old (first pregnancy) stated that "It is a very dreadful situation when you are left alone and you endure labor without your family or your own doctor," while another participant aged 30 years old (second time pregnancy) related that, "Every time the midwives came to me and checked my (vital) signs or my baby’s heart and explained to me about delivery progress, I felt safe. But when they left me, I panicked again".
Fear of endangering the baby’s health was another sub-theme frequently encountered. Most mothers shared the view that a long-lasting vaginal birth process could endanger the baby’s health. However, this misconception mostly returned to a lack of knowledge about pregnancy and the childbirth process. One test subject (first pregnancy, 27 years) commented that "I think continuous pressure on the baby’s head during labor may damage her/his brain."
In addition, fear of urinary and genital tract damage was also evident among the studied subjects. A few women disclosed their concerns about bodily damage following NVD and potential sexual and urinary tract dysfunction that may lead to less sexual satisfaction and affect the sexual relationship. Repeatedly, heard were mothers' concerns about urinary incontinence, a lack of sexual attraction, abandonment by their spouse, and the need for surgical repair. One woman (first pregnancy, 30 years) commented that "I think dilatation of the vagina during childbirth can affect my sexual relationship and may cause urinary incontinence."
The recommendations of others also played a role around the negative beliefs expressed by the study participants. A small number of mothers disliked the idea of giving birth vaginally because it can be a time-consuming procedure. Interestingly, they described NVD as an old-fashioned or outdated method of childbirth. One study participant aged 38 years old (second pregnancy) related that "I think natural birth is not very common among the new generation. They prefer cesarean to be considered prestigious." While another participant (first pregnancy, 21 years) declared that "My mother-in-law advises me not to undergo the suffering and troublesome method for childbirth. If we had an option to choose (for childbirth), I would have chosen cesarean birth absolutely."
Finally, determining effective strategies to make vaginal birth more acceptable and preferable for participants were tried. All women agreed that prenatal education should emphasize pain-relief methods. They believed women should be more aware of which birth method is safer, how to combat fears of labor, and how to learn more about pregnancy and the methods of childbirth. In addition, participants believed that if some women knew how alternative pain reduction methods worked, they would be less likely to choose unnecessary CS. Also, women proposed that midwives and physicians should have a more important role in this domain and spend more time counseling mothers to minimize misconceptions pertaining to vaginal birth.
Discussion
This study revealed that several psychological factors are involved in the prediction of the mothers’ intention towards planning a vaginal childbirth. Results of both the qualitative and quantitative studies showed that the more knowledge the participants have about the mode of childbirth, they tend to perceive a high degree of severity of surgical childbirth and their perceptions of self-efficacy increased; moreover, there was a greater likelihood of intending to deliver vaginally regardless of parity, gestational age or social class.
Using the EPPM in this study, it was observed how Iranian pregnant women’s degrees of perceived threat and perceived efficacy influence their intention to give birth vaginally. The study subjects were selected from six different regions to minimize any potential selection bias. Findings from the quantitative data appear consistent with the qualitative results that suggest that the participants exhibited concern regarding the potential for harm from cesarian surgery. However, susceptibility perceptions were found to be lower than other model components. It seems that a few women were not fully aware of (or in denial regarding) their vulnerability to the potential harms of CS. Despite the infrequency of severe maternal/fetal problems, a cesarean presents certain risks for the mother and child and should not be undertaken lightly.28 Apparently, incorrect beliefs of cesarean delivery as a safe option lead to its overuse.
Previously, it was believed that being older at first pregnancy, having a higher level of education, living in an urban environment, and having a smaller family size were all correlated with a greater probability of CS preference.8 However, no such finding was observed in this study. In addition, women with previous childbirth experience showed higher levels of self-efficacy and knowledge and a lower preference to be accompanied during labor, compared to first-time pregnant mothers. This finding is consistent with another Iranian study that described a greater competency among non-first-time mothers in adopting coping behaviors.29 It is stated that women evaluate their abilities to cope with different realities and make decisions accordingly. If they feel the birth is difficult, they act in a manner that reinforces their perception and vice versa.30
Although both quantitative and quantitative findings revealed that most pregnant women in Shahroud had a greater tendency to deliver vaginally (as opposed to CS), the current investigation of women’s perceptions showed that they often lacked knowledge and held negative beliefs towards vaginal childbirth based on their previous experiences or others’ recommendations. These could steer women away from plans for vaginal childbirth. These findings are impressive and consistent with other relevant studies that showed the most important reason for women changing their preference from vaginal birth to elective cesarean section was fear of labor pain, previous undesirable experience,31 and pelvic damage.32 Thus, the related fear of childbirth appeared to be the most common multi dimensional factor contributing to the tendency of preference for faster and less painful childbirth, particularly among younger mothers. However, the modality of this sentiment differed substantially. It implied that fear plays a central role in motivating people to plan health behaviors as previously mentioned.
The tendency to prefer a specific childbirth method is multi-factorial in causes. The main reasons leading to a high preference for surgical births over the past decade include several social, cultural and economic factors. Presumably, there could also be financial factors if health insurance payers withdraw reimbursements for elective cesarean surgery based on the mother’s request rather than a clinical necessity. Thus, it is not surprising that some medical indications such as large baby (fetal macrosomia), cephalopelvic disproportion (CPD), or maternal obesity are exaggerated in the hospital records.14
In this study, it was observed that participant’ religious beliefs were a positive factor on their perceptions of vaginal birth. As most of Iranian people have rigid, pious beliefs, they believe that childbirth is a sign of the Lord’s majesty and the nature of pregnancy and birth reinforces this philosophy, thus allowing women to trust their ability to proceed through the childbirth process with minimal fear and pain.6 Furthermore, caregivers, friends, and family appeared to influence the mothers’ beliefs and reinforce their positive perceptions. It is important to remember that these external influences have a significant impact on people’s behaviors and may shape their subjective norms.7,11 Moreover, the participants wished to be accompanied by a family member, especially by a spouse. They also desired to learn and apply pain reduction skills before or during pregnancy.
The study was limited to women living in a relatively developed area of Iran, thus generalizations should be taken with caution. However, mixing a quantitative and qualitative approach gives more thorough understanding of women’s birthing preferences and intentions.
Conclusion
The present study uses a theoretical model based on fear appeals and explores women’s beliefs about the extent of concerns and confidence that can influence health-related behaviors. The paper discussed how, in a representative sample of pregnant Iranian women, the perception of threat and efficacy, knowledge, and beliefs influence women’s intention to deliver vaginally. Women should learn more about the methods of childbirth and how to cope with fear and anxiety by promoting self-efficacy as an important prerequisite to acquiring coping skills and behaviors for childbirth. Likewise, educating women who had undesirable childbirth experiences and investigating fear factors during vaginal birth may help reduce women’s preference for elective cesarean birth. As pregnant women receive continuous labor support, they are more likely to deliver vaginally and use fewer pain medications. Supportive care during labor (via a competent midwife or trusted family member) facilitates emotional support and advocacy.
Acknowledgements
We extend special thanks to the midwives and participants for their kind assistance in facilitating data collection. The authors have no competing financial interests to disclose.
References
1. Kazmi T, Saiseema SV V, Khan S. Analysis of Cesarean Section Rate - According to Robson’s 10-group Classification. Oman Med J 2012 Sep;27(5):415-417.
2. Scarella AC, Chamy V, Sepúlveda M, Belizán JM. Medical audit using the Ten Group Classification System and its impact on the cesarean section rate. Eur J Obstet Gynecol Reprod Biol 2011 Feb;154(2):136-140.
3. Villar J, Carroli G, Zavaleta N, Donner A, Wojdyla D, Faundes A, et al; World Health Organization 2005 Global Survey on Maternal and Perinatal Health Research Group. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ 2007 Nov;335(7628):1025.
4. Harper LM, Odibo AO. Mode of delivery and obstetric outcomes in Asia. Womens Health (Lond Engl) 2010 May;6(3):365-366.
5. The Ministry of Health, Maternal Health Office, Iran. National program for maternal health in The Forth Program of socio-economic and cultural Development 2010. http://www.fhp.hbi.ir [In Persian]. Accessed Feb 21, 2011.
6. Torkzahrani S. Commentary: childbirth education in iran. J Perinat Educ 2008;17(3):51-54.
7. Leone T, Padmadas SS, Matthews Z. Community factors affecting rising caesarean section rates in developing countries: an analysis of six countries. Soc Sci Med 2008 Oct;67(8):1236-1246.
8. Ahmad-Nia S, Delavar B, Eini-Zinab H, Kazemipour S, Mehryar AH, Naghavi M. Caesarean section in the Islamic Republic of Iran: prevalence and some sociodemographic correlates. East Mediterr Health J 2009 Nov-Dec;15(6):1389-1398.
9. Badakhsh MH, Seifoddin M, Khodakarami N, Gholami R, Moghimi S. Rise in cesarean section rate over a 30-year period in a public hospital in Tehran, Iran. Arch Iran Med 2012 Jan;15(1):4-7.
10. Maharlouei N, Moalaee M, Ajdari S, Zarei M, Lankarani KB. Caesarean Delivery in South-Western Iran: Trends and Determinants in a Community-Based Survey. Med Princ Pract 2012. Epub ahead of print.
11. Mohammaditabar Sh, Kiani A, Heidari M. The survey on tendencies of primiparous women for selecting the mode of delivery. J Babol Univ Med Sci 2009;11(3):54-59. In Persian.
12. Sharifi rad Gh, Fathian Z, Tirani M, Mehaki B. Investigation of pregnant women’s attitudes toward normal childbirth and cesarean birth based on Behavioral Intention Model. Ilam Journal of Medical Sciences 2007;15(1):19-23. in Persian.
13. Faraji R, Zahiri Z, Farjad F. Investigation of knowledge and attitudes of pregnant women toward modes of childbirth. Gilan Journal of Medical Sciences 2003;12(46):69-75.
14. Shahroud University of Medical Sciences, Deputy for Research and Education, Iran. Statistical report of registered births of hospitals in Shahroud.Unpublished data. 2011.
15. Witte K. Fear as Motivator, Inhibitor: Using Parallel Process Explain Fear Appeal Fear as the Extended Model to Successes and Failures, in Handbook of Communication and Emotion: Research, Theory, Applications, and Contexts. Academic Press: East Lansing, Michigan.1995.
16. Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Thousand Oaks, CA: Sage Publications, Inc.2011.
17. Chow MY, Quine S, Li M. The benefits of using a mixed methods approach–quantitative with qualitative–to identify client satisfaction and unmet needs in an HIV healthcare centre. AIDS Care 2010 Apr;22(4):491-498.
18. Anderson C, Harris MS, Kovarik R, Skelton J. Discovering expectant mothers’ beliefs about oral health: an application of the Centering Pregnancy Smiles program. Int Q Community Health Educ 2009-2010-2010;30(2):115-140.
19. Witte K, Cameron KA, McKeon JK, Berkowitz JM. Predicting risk behaviors: development and validation of a diagnostic scale. J Health Commun 1996 Oct-Dec;1(4):317-341.
20. Campo S, Askelson NM, Spies EL, Losch M. Ambivalence, communication and past use: understanding what influences women’s intentions to use contraceptives. Psychol Health Med 2012;17(3):356-365.
21. Balicer RD, Barnett DJ, Thompson CB, Hsu EB, Catlett CL, Watson CM, et al. Characterizing hospital workers’ willingness to report to duty in an influenza pandemic through threat- and efficacy-based assessment. BMC Public Health 2010;10:436.
22. Goei R, Boyson AR, Lyon-Callo SK, Schott C, Wasilevich E, Cannarile S. An examination of EPPM predictions when threat is perceived externally: an asthma intervention with school workers. Health Commun 2010 Jun;25(4):333-344.
23. Witte K, Meyer G, Martell D. Effective Health Risk Messages: A Step-By-Step Guide. SAGE Publications, Inc.2001.
24. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005 Nov;15(9):1277-1288.
25. Yaghmaie F. Content validity and its estimation. J Med Educ 2003;3(1).
26. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health 2007 Aug;30(4):459-467.
27. Burns N, Grove SK. The Practice of Nursing Research, Philadelphia: WB. Saunders, 1997.
28. Declercq E, Barger M, Cabral HJ, Evans SR, Kotelchuck M, Simon C, et al. Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstet Gynecol 2007 Mar;109(3):669-677.
29. Toghyani R, Ramezani MA, Izadi M, Shahidi Sh, Aghdak P, Motie Z, et al. The Effect of Prenatal Care Group Education on Pregnant Mothers' Knowledge, Attitude and Practice. Iranian journal of education in medicine 2007; 7(2):317-324.
30. Lowe NK. The nature of labor pain. Am J Obstet Gynecol 2002 May;186(5)(Suppl Nature):S16-S24.
31. Pang MW, Leung TN, Lau TK, Hang Chung TK. Impact of first childbirth on changes in women’s preference for mode of delivery: follow-up of a longitudinal observational study. Birth 2008 Jun;35(2):121-128.
32. Hantoushzadeh S, Shariat M, Rahimi Foroushan A, Ramezanzadeh F, Masoumi M. Sexual satisfaction after child birth: vaginal versus elective cesarean delivery. Tehran Univ Med J 2009;66(12):931-935.
|