A four-year-old boy presented with his parent to the emergency department complaining of face deviation and mouth lesions for three days. He had no similar attack before and no medical history. The parent claimed that the patient complained of fever, cough, rhinorrhea, and ear pain one week before. The patient followed-up with a general practitioner who prescribed him antipyretics, antihistamine, and cough syrup. While the patient’s condition improved initially, he later started to complain of tongue pain. His parents noticed a facial deviation when smiling, a large white lesion on his tongue, and decreased lacrimation of the left eye when crying. Additionally, the patient complained of abnormal taste sensations and was brought to the emergency department. He looked comfortable, with no acute distress. His vital signs showed a pulse rate of 110 beats/min, a respiratory rate of 26 breaths/min, and a temperature of 37.7 oC.
Oral examination showed multiple whitish lesions on the anterior two-thirds of the tongue’s left side [Figure 1a]. The patient was unable to close his left eye and the left nasolabial fold was absent. Furthermore, the patient’s mouth deviated to the right when asked to smile or show his teeth [Figure 1b]. He had multiple erythematous vesicular rashes on his left ear [Figure 1c]. The neck examination revealed enlarged cervical lymph nodes. He had a clear chest with no added heart sounds. Proper neurological examination was normal apart from the left-side facial palsy. The consultant otolaryngologist instructed to discharge the patient on acyclovir and prednisone along with a follow-up appointment with the otolaryngology clinic within five days.
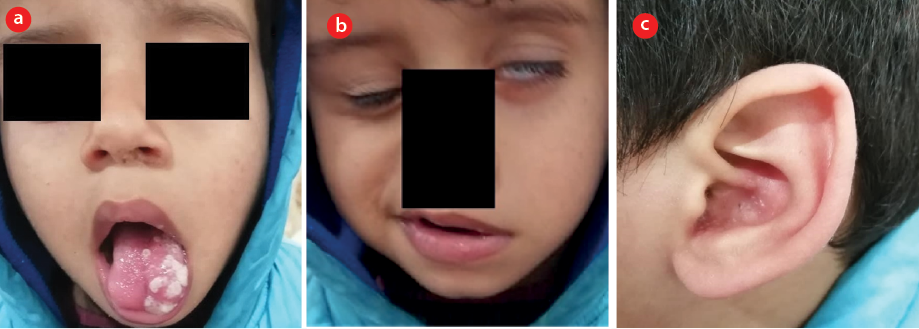 Figure 1 : (a) Oral examination showed multiple vesicular lesions with a whitish cover on the anterior two-thirds of the tongue’s left side. (b) Left lower motor neuron facial palsy where the patient cannot close his left eye, loss of left nasolabial fold, and the mouth deviated to the right side. (c) Erythematic vesicular rashes on the left ear.
Figure 1 : (a) Oral examination showed multiple vesicular lesions with a whitish cover on the anterior two-thirds of the tongue’s left side. (b) Left lower motor neuron facial palsy where the patient cannot close his left eye, loss of left nasolabial fold, and the mouth deviated to the right side. (c) Erythematic vesicular rashes on the left ear.
Question
What is the most likely diagnosis?
a. Acoustic neuroma.
b. Bell’s palsy.
c. Postherpetic neuralgia.
d. Ramsay Hunt syndrome.
e. Temporomandibular disorders.
Answer
d. Ramsay Hunt syndrome.
Discussion
Ramsay Hunt syndrome is a disease characterized by peripheral facial palsy with a vesicular rash involving the ear, oropharyngeal mucous membrane, or both. It is caused by varicella-zoster virus infection of the head and the neck. It typically affects the seventh cranial nerve, although other cranial nerves, including the eighth, ninth, tenth, and eleventh could be affected. This infection leads to the development of vesicular rashes affecting the external ear and ipsilateral anterior two-thirds of the tongue along with ipsilateral facial palsy, geniculate ganglionopathy, or radiculoneuropathy. Furthermore, 16% and 18% of unilateral facial palsy in children and adults, respectively, are attributed to Ramsay Hunt syndrome. This syndrome is rare in children under six years. Typically, patients with Ramsay Hunt syndrome present with ipsilateral lower motor neuron facial paresis/palsy, headache, otalgia, and a vesicular rash on the ear or mouth. Additionally, vertigo, ipsilateral hearing loss, cervical adenopathy, and fever can be observed. The diagnosis is mainly based on history and physical examinations that shows the characteristic symptoms. Varicella-zoster virus can be isolated from the vesicular fluid. Ramsay Hunt syndrome management aims to relieve the symptoms and minimize the complications. The prognosis improves with early medicine administration. The treatment typically involves a combination of oral acyclovir and oral corticosteroids. The patient should follow-up with the otolaryngology clinic regularly to observe the recovery and detect any possible complications.1,2
Disclosure
Informed consent was obtained from the patient's parents.
references
- 1. Jeon Y, Lee H. Ramsay Hunt syndrome. J Dent Anesth Pain Med 2018 Dec;18(6):333-337.
- 2. Muengtaweepongsa S, Sukphulloprat P. Ramsay hunt syndrome. 2018 [cited 2020 August 30]. Available from: https://emedicine.medscape.com/article/1166804-overview.