Wildlife in Oman is as varied as the country’s topography which consist of vast deserts, mountains, rocky hills, valleys, and even tropical rain forests. Among more than 20 species of snakes in Oman, nine are venomous.1 Most of the latter belong to the Viperidae family, whose venom is primarily hemotoxic. Of these, 90% cases of human envenomation are caused by the saw-scaled viper (Echis carinatus), found throughout the country, with a preference to rocky areas. Around 9% are caused by Burton’s carpet viper (Echis coloratus) found in hilly regions, or the horned viper (Cerastes gasperetti) which inhabits the deserts.2
Worldwide, an estimated 421 000 envenomation cases and 20 000 deaths occur due to snakebites each year.3 The incidence in Oman is not clear due to under-reporting from rural areas where most bites occur. Clinical presentations range from mild and localized, to severe systemic manifestations. Antivenom is indicated when there are significant local signs of bite, systemic signs, circulatory collapse, or systemic bleeding.4 Early management is essential to avoid complications, such as venom-induced consumption coagulopathy, renal toxicity, cardiac toxicity, and even death. A study in tertiary care hospitals in central India concluded that certain predictors, such as bleeding, respiratory failure, and hematotoxicty, can be predictors for mortality among snakebite patients.5 Risk factors for renal toxicity after snakebite have been described in many studies.6–10 Despite such indicators, it is difficult to predict which individual patient might be at significant risk of developing complications.
To the best of our knowledge, no study has investigated the risk factors for developing snakebite-related complications in Oman. This study aims to narrow the research gap by assessing the risk factors of snakebite-associated complications by evaluating cases presenting to emergency departments of two hospitals in Oman.
Methods
This was a multicenter retrospective observational study, using data from two different emergency departments, namely Sultan Qaboos University Hospital (SQUH), a tertiary hospital in Muscat city, and Rustaq Hospital, a secondary hospital located in a semi-rural town in South Al Batinah governorate.
The study was approved by the institutional ethical committees of both hospitals. Patient's data was obtained from the hospital electronic records. Patient demographics, the geographical location (terrain) where the snake was encountered, site of the bite, initial symptoms and vital signs at presentation, laboratory investigations, time elapsed from the bite to hospital presentation, time taken from the bite to administration of anti-snake venom (ASV), the dose of ASV used initially and total amount administered during hospitalization, the use of antibiotics and tetanus toxoid, and details of complications that arose, were obtained and evaluated.
Inclusion criteria comprised: (a) a definitive patient report of snakebite; (b) a clinical picture consistent with snakebite, such as the presence of fang marks, cellulitis, coagulopathy, or neuroparalysis; and (c) where laboratory results confirmed snake envenomation. Excluded from the study were: (a) cases of unknown bite source; (b) where the clinical picture was not consistent with snakebite; (c) patients with preexisting renal diseases (e.g. serum creatinine >1.5 mg/dl before snake bite), with preexisting deranged coagulation profiles, or known to be on anticoagulants; and (d) where laboratory data was unavailable.
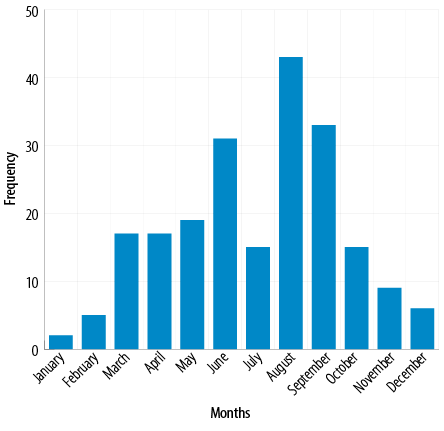
Figure 1: Frequency of snake bites by month.
Acute kidney injury (AKI) was defined as an abrupt (< 48 hours) absolute increase in the serum creatinine concentration of ≥ 0.3 mg/dL from baseline measured after admission or elsewhere after the snake bite, an increase in the serum creatinine concentration of ≥ 50% above baseline, oliguria of < 0.5 mL/kg per hour for more than 6 hours, serum creatinine of > 1.5 mg/dL, or oliguria (urine output < 400 mL/day).6 Venom-induced consumption coagulopathy was defined a prolonged prothrombin time (PT) of > 1.5 times normal. Partial thromboplastin time (PTT) of > 10 seconds above control value was classified severe coagulopathy.11,12 Compartment syndrome was defined based on clinical findings in the affected limb, including presence of pallor, lack of pulse, pain, change of color, and increased swelling. Swelling at the bite site was classified as mild, moderate, and severe based on the physician’s assessment using Oman’s national management guideline of poisoning.4
The t-test was used to assess continuous normally distributed variables. For categorical data, the Chi-square test was used, with the Fisher's exact test for small numbers. For variables that were not normally distributed, the Mann-Whitney U test was used. A p-value of < 0.05 was considered statistically significant. The statistical analysis was performed using the Statistical Package for the Social Sciences, version 11.0 (SPSS Inc. (1999). SPSS Base 10.0 for Windows User's Guide. SPSS Inc., Chicago IL).
Table 1: Sociodemographic characteristics of the participants (N = 212).
|
Age (median, IQR) |
30 (23–41) |
|
Sex |
|
|
Male |
178 (84.0) |
|
Female |
34 (16.0) |
|
Nationality |
|
|
Omani |
130 (61.3) |
|
Non-Omani |
82 (38.7) |
|
Hospital |
|
|
SQUH |
11 (5.2) |
|
Rustaq Hospital |
201 (94.8) |
|
Area where snake encountered |
|
|
Farm |
132 (62.3) |
|
Valley |
35 (16.5) |
IQR: interquartile range; SQUH: Sultan Qaboos University Hospital.
Results
Among a total of 236 snakebite cases identified from the hospital databases, 24 patients did not meet the inclusion criteria. Therefore, 212 cases were included in this study. Of these, 11 patients presented at SQUH and 201 patients at Rustaq Hospital. Table 1 illustrates the baseline characteristics of the included patients. The median age was 30 years and 84.0% were male. The youngest patient was one year old, and the oldest was 85 years old. Most snakebites occurred on farms (62.3%), 16.5% in valleys, while 20.8% patients were bitten at home. The monthly incidence in cases followed a rising trend during the summer months, peaking in August [Figure 1].
Table 2 illustrates the clinical features of the patients, with the vast majority complaining of pain (97.2%) and swelling (85.8%). Bleeding from the site of the bite was present in 8.5% cases and nausea or vomiting in 9.9%. The majority of the patients (124, 58.5%) were bitten on a lower limb and 85 (40.1%) on an upper limb. Three patients were bitten on the torso.
Of the 212 patients included in this study, 102 (48.1%) developed complication from the snake bite, the major ones being coagulopathy (38.7%), AKI (6.6%), and external bleeding (2.4%). One pediatric patient developed compartment syndrome and had to be transferred to a tertiary hospital. No deaths were recorded during the study period.
Among the variables included for bivariate analysis [Table 3], there was an independent association of AKI with bleeding as an initial symptom and the geographical location (rocky valley) where the snake was encountered. For those who developed coagulopathy, the bivariate analysis [Table 4] showed an independent association between coagulopathy and bleeding, nausea and vomiting as initial symptoms, swelling at the site of the bite, and delay between the time of snake bite till the time of presentation and ASV administration.
Table 2: Clinical variables of the participants
(N = 212).
|
Initial symptoms |
|
|
Pain |
206 (97.2) |
|
Swelling |
182 (85.5) |
|
Bleeding from site of bite |
18 (8.5) |
|
Nausea/vomiting |
21 (9.9) |
|
Shortness of breath |
– |
|
Site of bite |
|
|
Lower limb |
124 (58.5) |
|
Upper limb |
85 (40.1) |
|
Torse |
3 (1.4) |
|
Classification of swelling |
|
|
None |
33 (15.6) |
|
Mild |
125 (59) |
|
Moderate |
51 (24.1) |
Table 3: Association of the variables with acute kidney injury.
|
Age (median, IQR) |
40 (22–56) |
30 (23–40) |
0.085 |
|
Sex |
|
|
|
|
Male |
12 (85.7) |
166 (83.8) |
> 0.050 |
|
Female |
2 (14.3) |
32 (16.2) |
|
|
Nationality |
|
|
|
|
Omani |
13 (92.9) |
117 (59.1) |
0.011 |
|
Non-Omani |
1 (7.1) |
81 (40.9) |
|
|
Area where snake encountered |
|
Desert |
- |
1 (0.5) |
< 0.001 |
|
Farm |
2 (14.3) |
130 (65.7) |
|
|
Valley |
12 (85.7) |
23 (11.6) |
|
|
Home |
- |
44 (22.2) |
|
|
Site of bite |
|
|
|
|
Lower limb |
10 (71.4) |
114 (57.6) |
0.506 |
|
Upper limb |
4 (28.6) |
81 (40.9) |
|
|
Torso |
- |
3 (1.5) |
|
|
Symptoms |
|
|
|
|
Nausea/vomiting |
5 (35.7) |
16 (8.1) |
0.007 |
|
Bleeding |
6 (42.9) |
12 (6.1) |
< 0.001 |
|
Swelling |
14 (100) |
168 (84.8) |
0.227 |
|
Pain |
14 (100) |
192 (97.0) |
> 0.050 |
|
Laboratory results |
|
|
|
|
Hemoglobin |
|
|
0.464 |
|
Anemia |
2 (14.3) |
10 (5.1) |
|
|
Normal |
8 (57.1) |
123 (62.1) |
|
|
Polycythemia |
4 (28.6) |
64 (32.3) |
|
|
INR |
|
|
0.033 |
|
Normal |
9 (64.3) |
169 (85.4) |
|
|
Mild-moderate |
2 (14.3) |
2 (1.0) |
|
|
Severe |
3 (21.4) |
27 (13.6) |
|
|
WBC |
|
|
0.36 |
|
Normal |
12 (85.7) |
137 (69.2) |
|
|
Abnormal |
2 (14.3) |
59 (29.8) |
|
|
Platelets |
|
|
0.398 |
|
Low |
0 |
9 (4.5) |
|
|
Normal |
14 (100) |
184 (92.9) |
|
|
High |
0 |
2 (1.0) |
|
|
Prothrombin time |
|
|
0.178 |
|
Normal |
1 (7.1) |
50 (25.3) |
|
|
Mild-moderate |
9 (64.3) |
119 (60.1) |
|
|
Severe |
4 (28.6) |
29 (14.6) |
|
|
Time from bite to hospital in minutes (median, IQR) |
145 (98–323) |
120 (65–180) |
0.157 |
|
Presentation to receiving ASV in minutes (median, IQR) |
133 (88–203) |
100 (22–120) |
0.016 |
AKI: acute kidney injury; ASV: anti-snake venom; INR: international normalized ratio; IQR: interquartile range; SD: standard deviation;
WBC: white blood cell count.
Table 4: Association of the variables with coagulopathy.
|
Age (median, IQR) |
28 (18–41) |
31 (24–41) |
> 0.050 |
|
Gender |
|
|
> 0.050 |
|
Male |
71 (86.6) |
107 (82.3) |
|
|
Female |
11 (13.4) |
23 (17.7) |
|
|
Nationality |
|
|
0.313 |
|
Omani |
54 (65.9) |
76 (58.5) |
|
|
Non-Omani |
28 (34.1) |
54 (41.5) |
|
|
Area of snake encounter |
|
|
< 0.001 |
|
Desert |
- |
1 (0.8) |
|
|
Farm |
39 (47.6) |
93 (71.5) |
|
|
Valley |
25 (30.5) |
10 (7.7) |
|
|
Home |
18 (22.0) |
26 (20.0) |
|
|
Site of bite |
|
|
0.002 |
|
Lower limb |
59 (72.0) |
65 (50.0) |
|
|
Upper limb |
23 (28.0) |
62 (47.7) |
|
|
Torso |
- |
3 (2.3) |
|
|
Symptoms |
|
|
|
|
Nausea/vomiting |
16 (19.5) |
2 (1.5) |
< 0.001 |
|
Bleeding |
16 (19.5) |
12 (9.2) |
< 0.001 |
|
Swelling |
81 (98.8) |
101 (77.7) |
< 0.001 |
|
Pain |
82 (100) |
125 (96.2) |
0.301 |
|
Laboratory results |
|
|
|
|
Hemoglobin |
|
|
0.903 |
|
Anemia |
5 (6.1) |
7 (5.4) |
|
|
Normal |
52 (63.4) |
79 (60.8) |
|
|
Polycythemia |
25(30.5) |
43 (33.1) |
|
|
Creatinine |
|
|
0.435 |
|
Normal |
78 (95.1) |
126 (96.9) |
|
|
Abnormal |
4 (4.9) |
3 (2.3) |
|
|
WBC |
|
|
0.121 |
|
Normal |
53 (64.6) |
96 (73.8) |
|
|
Abnormal |
29 (35.4) |
32 (24.6) |
|
|
Platelets |
|
|
0.199 |
|
Low |
6 (7.3) |
3 (2.3) |
|
|
Normal |
74 (90.2) |
124 (95.4) |
|
|
High |
2 (2.4) |
2 (1.5) |
|
|
Time from bite to hospital in minutes (median, IQR) |
120 (120–187) |
120 (120–180) |
0.052 |
|
Presentation to receiving ASV in minutes (median, IQR) |
120 (120–171) |
75 (75–120) |
< 0.001 |
ASV: anti-snake venom; IQR: interquartile range; SD: standard deviation; WBC: white blood cell count.
Discussion
The snakebite victims in this study were mostly male adults, with most incidents occurring in farms, a common habitat for snakes in Oman. Most incidents occurred during the summer months (March to September), peaking in August; snakes are known to be more active during summers than in winters.13 The most common site of the bite was a lower limb, followed by an upper limb while bites to the torso were rare, with just three cases. Lower limbs appear to be vulnerable while walking in farms or traversing valleys without appropriate footwear. Similar trend has been described in other studies.14,15
Notably, those presenting with snakebites received in the valleys and had bleeding from the site of bite were at higher risk of developing AKI than those who were bitten on a farm. This may be because in the rocky valleys of Oman there is high possibility of being bitten by saw-scaled viper (Echis carinatus)2 whose venom is reported to trigger direct nephrotoxicity.16–18 The venom of this snake also causes intravascular hemolysis leading to bleeding from the site of the bite.8,17 Other causes mentioned in literature as leading to AKI after snake bite envenomation, namely, hypotension and significant bleeding,17 were not observed in AKI patients in
this study.
Patients in this study who were bitten on a farm tended to develop coagulopathy, probably due to being bitten by another member of the Viperidae family, the Burton’s carpet viper (Echis coloratus), often found in hilly regions and farms.2 Its bite is known to cause venom-induced consumption coagulopathy, which occurs secondary to the activation of a coagulation cascade by procoagulant toxins in the snake venom, in turn leading to a severe coagulation factor deficiency that ultimately causes hemorrhage.19–21 Echis coloratus victims also tend to present with nausea, vomiting, swelling, and bleeding at the site of bite, were observed in
this study.
The results from this study showed that delayed presentation to the emergency department and delayed administration of ASV were the main risk factors for developing coagulopathy. The delay of administration of ASV was observed in Rustaq Hospital, as they had a protocol to only administer the antivenom in the admission ward to those in high dependency beds rather than in the emergency department. The administration of ASV requires observation for any anaphylactic reactions, a possible side effect, which can be conducted in an adequately equipped emergency department. As it is well known that the early presentation to the emergency room and early administration of ASV are closely linked to an increased efficacy of the ASV and good outcomes,22 and also supported by the current study’s findings, we recommend revision of the protocol in secondary hospitals in Oman so that ASV can administered and the patients monitored in the emergency department itself. As the vast majority of cases occur in rural areas and the need for urgent treatment, we also recommend that rural primary health centers situated far from secondary hospitals to be fully equipped to facilitate the administration of ASV.
The most notable limitation of this study is its retrospective nature. Certain laboratory variables could not be studied as they had not been acquired from the patients. Another limitation was that the identification of the snakes was not carried out or reported in the patient records, though this is usually not feasible. In addition, the sample size being small, multivariate analysis could not be run for some variables as predictors of complications. Finally, this study represents only the northern part of
Oman. For a more representative picture, future studies need to include other parts of the country, especially the southern Dhofar governorate, which has a monsoon climate and the home to other snake species such as the Arabian cobra whose venom is predominantly neurotoxic.
Conclusion
To the best of our knowledge, this is the first study of its kind in Oman. This study noted that the type of the location where the snake was encountered, whether a valley or a farm, was correlated with the risk for developing either AKI or coagulopathy. Time taken from the bite till ASV administration was associated with the risk of developing of coagulopathy. Therefore, rapid administration of ASV to avoid unnecessary complications is crucial. As most snakebites occur in rural areas and the need for immediate treatment, there is a strong case for equipping rural and semi-rural secondary hospitals, and even primary health centers in Oman with sufficient facilities and expertise to manage
these emergencies.
Disclosure
The abstract of this paper was published in the European Journal of Emergency Medicine. The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Scrimgeour EM, Gallagher M, Gardner A, Al Kaabi JM. Venomous snake-bite and use of polyvalent snake antivenom in Oman. Oman Med J 2001 Jan;18(1):20-26.
- 2. Al-Lawati A, Al-Abri SS, Lalloo DG. Epidemiology and outcome of snake bite cases evaluated at a tertiary care hospital in Oman. J Infect Public Health 2009;2(4):167-170.
- 3. Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, et al. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med 2008 Nov;5(11):e218.
- 4. Ministry of Health of Oman. National management guidelines of poisoning. 2018 [cited 2020 May 2]. Available from: https://www.moh.gov.om/en/-/---906 /.
- 5. Chaudhari TS, Patil TB, Paithankar MM, Gulhane RV, Patil MB. Predictors of mortality in patients of poisonous snake bite: Experience from a tertiary care hospital in Central India. Int J Crit Illn Inj Sci 2014 Apr;4(2):101-107.
- 6. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al; Acute Kidney Injury Network. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007;11(2):R31.
- 7. Dharod MV, Patil TB, Deshpande AS, Gulhane RV, Patil MB, Bansod YV. Clinical predictors of acute kidney injury following snake bite envenomation. N Am J Med Sci 2013 Oct;5(10):594-599.
- 8. Chugh KS. Snake-bite-induced acute renal failure in India. [cited 2022 Jan 4]. Available from: Kidney Int 1989 Mar;35(3):891-907.
- 9. Li W, Chen F, Wu S. The related risk factors analysis of snake-bite induced acute kidney injury. Med Sci Monit 2016 Jul;22:2335-2339.
- 10. Singh RR, Uraiya D, Kumar A, Tripathi N. Early demographic and clinical predictors of developing acute kidney injury in snake bite patients: a retrospective controlled study from an Indian tertiary care hospital in North Eastern Uttar Pradesh India. Indian J Crit Care Med 2016 Jul;20(7):404-408.
- 11. Arruda V, High KA, Loscalzo J, Kasper D, Hauser S, Fauci A, et al. Harrison’s principles of internal medicine. [cited 2019 May 3]. Available from: https://scholar.google.com/scholar_lookup?title=Harrison%27s+Principles+of+Internal+Medicine&author=V+Arruda&author=KA+High&publication_year=2008&.
- 12. Firkin F, Chesterman C, Rush B, Pennigton D. De Gruchy’s clinical haematology in medical practice. John Wiley & Sons; 2008 [cited 2019 May 3]. Available from: https://scholar.google.com/scholar_lookup?title=de+Gruchy%27s+Clinical+haematology+in+Medical+Practice&publication_year=1997&.
- 13. Al-Sadoon MK. Snake bite envenomation in Riyadh province of Saudi Arabia over the period (2005-2010). Saudi J Biol Sci 2015 Mar;22(2):198-203.
- 14. Ruha A-M, Kleinschmidt KC, Greene S, Spyres MB, Brent J, Wax P, et al; ToxIC Snakebite Study Group. Snakebite study group. The epidemiology, clinical course, and management of snakebites in the North American Snakebite Registry. J Med Toxicol 2017 Dec;13(4):309-320.
- 15. Feitosa ES, Sampaio V, Sachett J, Castro DB, Noronha Md, Lozano JL, et al. Snakebites as a largely neglected problem in the Brazilian Amazon: highlights of the epidemiological trends in the State of Amazonas. Rev Soc Bras Med Trop 2015;48(Suppl 1):34-41.
- 16. Ali G, Kak M, Kumar M, Bali SK, Tak S, Hassan G, et al. Acute renal failure following Echis carinatus (saw – scaled viper) envenomation. Indian J Nephrol 2004;14:177-181.
- 17. Kohli HS, Sakhuja V. Snake bites and acute renal failure. Saudi J Kidney Dis Transpl 2003 Apr-Jun;14(2):165-176.
- 18. Abdel-Nabi IM, Rahmy TR. Influence of the venom of snake Echis carinatus on the structure and function of the hepatic tissues of white rat. J. Egypt. Ger. Soc. Zool. 1992:171-87 [cited 2020 June 18]. Available from: https://scholar.google.com/scholar_lookup?journal=J.+Egypt.+Ger.+Soc.+Zool.+(C)&title=Influence+of+the+venom+of+snake+Echis+carinatus+on+the+structure+and+function+of+the+hepatic+tissues+of+white+rat&author=I.M.+Abdel-Nabi&author=T.R.+Rahmy&publication_year=1992&pages=171-187&.
- 19. Maduwage K, Isbister GK. Current treatment for venom-induced consumption coagulopathy resulting from snakebite. PLoS Negl Trop Dis 2014 Oct;8(10):e3220.
- 20. Obeidat MB, Al-Swailmeen AM, Al-Sarayreh MM, Rahahleh KM. Thrombotic microangiopathy following Arabian saw-scaled viper (Echis coloratus) bite: case report. Am J Case Rep 2020 Apr;21:e922000-1-e922000-5.
- 21. Dart RC. Medical toxicology. Lippincott Williams & Wilkins; 2004. p. 1967.
- 22. Warrell DA. WHO/SEARO Guidelines for the clinical management of snake bites in the Southeast Asian region. Southeast Asian J Trop Med Public Health 1999;30(Suppl 1):1-85.