Since the 1960’s when Dr. Bowen introduced composite resin (CR) restorative material, CR has become the most used restorative material in dental clinics.1,2 One of the significant shortcomings of CR is polymerization shrinkage caused by its methacrylate-based monomer’s free-radical polymerization. Further polymerization shrinkage generates internal stresses within the restorations, and the restoration-tooth inter-face that might exceed the bond strength between the resin and the tooth interface can lead to undesirable sequelae.3–5 Thermal changes and masticatory forces during function may adversely affect adhesive bonding and marginal adaptation.6,7 Due to differences in thermal expansion and contraction coefficients between CR and tooth structure, internal stresses could develop at the adhesive interface. Combined with masticatory forces, these stresses can lead to debonding, gap formation, and cuspal deformation.8–12 Marginal gaps allow micro-leakage that can result in discoloration, as post-operative sensitivity, cuspal deformation, and recurrent caries.
Modified CR composition and application techniques have been utilized to overcome some drawbacks, chiefly polymerization shrinkage and gap formation. For example, in the sandwich technique, a glass ionomer base is applied first to reduce the CR volume and reduce shrinkage. Another technique variation, layering, involves the incremental application of CR (each layer being no more than 2 mm thick) to minimize contraction. This process is time-consuming, and the prolonged application time increases sensitivity.13–15
In the last decade, CR’s material composition has been altered, introducing the bulk-fill CRs, aiming to reduce contraction stress and the number of restorative steps required. Bulk-filling entails CR placement in one layer up to 4–5 mm thick with optimum polymerization. There is no precise classification for a bulk-fill CR, but it is available in two consistencies: low-viscosity (similar to flowable CRs) and high-viscosity (similar to conventional CRs).16–18
Studies have shown that flowable CR can improve marginal adaptation and adhesion by acting as a flexible cushion to absorb stress.19,20 Manufacturers introduced a low-viscosity bulk-fill CR to promote marginal adaptation, but it had low mechanical properties and required veneering with a conventional CR. This led to creating a high-viscosity bulk-fill CR that manufacturers claim does not need to be layered with conventional CR and can be used as the final restorative material. Despite the rapid release and modification of bulk-fill CRs, there is scientific evidence to support the use of bulk-fill CR as it showed similar performance clinically compared to conventional CR and superior performance in vitro.21–24,25
Several in vitro testing methods have been used to measure marginal adaptation and interface gap formation and are direct (clinical, visual, and tactile examination) or indirect (radiographs). These customarily-employed methods have shortcomings. Conventional radiographs are two-dimensional, limiting the ability to study the whole interface, and some direct techniques are destructive. A new and innovative technology, microcomputed tomography (μ-CT), has been introduced to measure marginal integrity and internal adaptation of restorations. It allows for nondestructive evaluation of the tooth-restoration interface in two- and three-dimensions.26–28
Some reports suggest that bulk-fill composite reduces cuspal deflection but increases marginal leakage; others assert that bulk-fill CR improves marginal adaptation but increases cuspal deflection.29–31 This study sought to evaluate the adaptation ability of different bulk-fill composites by evaluating the volumetric changes in the marginal gap size and, by extension, restoration success. Specifically, to identify any differences in marginal gap size after polymerization and aging process concerning the type of resin-based composite (RBC) used. The null hypothesis tested was that there is no difference in gap volume after aging between the tested RBC and tooth structure enamel or dentin.
Methods
Twenty-eight human molars (mandibular molar) free of caries and cracks were extracted for periodontal reasons. Written informed consent was obtained from each patient before treatment. Calculus deposits were removed by hand-scaling before random distribution into four groups (n = 7 per group).32,33 Three bulk-fill CRs—Smart Dentin Replacement SDR Flow+ (SDR) (Dentsply Sirona, York, PA, USA), 3M™ Filtek™ One Bulk Fill (FBF) (3M ESPE, Maplewood, MN, USA), and Tetric® N-Ceram Bulk Fill (TBF) (Ivoclar Vivadent, Schaan, Liechtenstein)—and one conventional composite (CC)—Filtek™ Z350 (3M ESPE, Maplewood, MN, USA)—were used to restore the teeth.
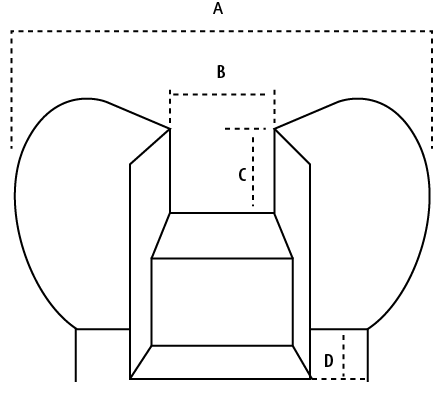
Figure 1: Cavity preparation configuration. (a) Bucco-lingual cusps width (BLW). (b) Inter-proximal cavity width (1/3 BLW). (c) Enamel margin (above the enamel-cementum junction). (d) Dentin margins (1 mm beyond enamel-cementum junction).
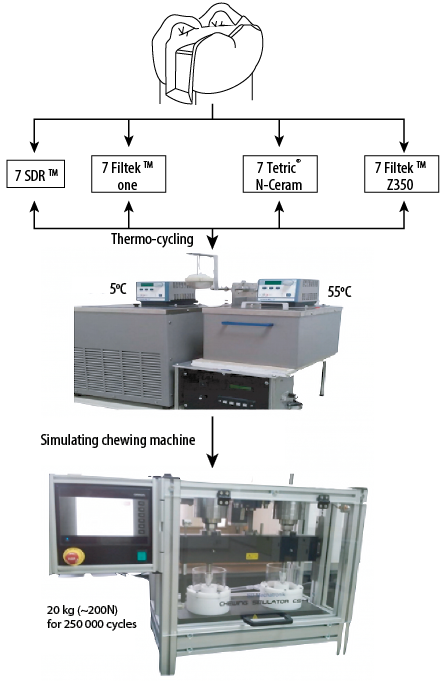
Figure 2: Scheme of the experiment methodology and steps of testing.
Table 1: Statistical results for enamel margin before and after aging.
|
SDR |
-0.004 |
0.003 |
|
FBF |
-0.010 |
0.008 |
|
TBF |
-0.009 |
0.012 |
SDR: Smart Dentin Replacement Flow+; FBF: Filtek™ One Bulk Fill; TBF: Tetric® N-Ceram Bulk Fill; CC: conventional composite resin.
Table 2: Statistical results for dentin margin before and after aging.
|
SDR |
-0.011 |
0.012 |
|
FBF |
-0.012 |
0.023 |
|
TBF |
-0.008 |
0.010 |
SDR: Smart Dentin Replacement Flow+; FBF: Filtek™ One Bulk Fill; TBF: Tetric® N-Ceram Bulk Fill; CC: conventional composite resin.
.png)
Figure 3: The volumetric width of the interfacial gap at the enamel-restoration interface before and after aging and enamel margins-gap descriptive statistics.
Each molar was prepared using diamond burs with copious water irrigation to receive a standard mesio-occlusal-distal (MOD) cavity in which the width of the isthmus of the preparation was half the bucco-palatal width/buccolingual width (BPW/BLW), and the interproximal box width was one-third the BPW/BLW. Occlusal depth was standardized using 330 burs marked (at 2 mm depth). The cavity was prepared as an extension of the central cavity on the mesial aspect, leaving the enamel margins (4 mm height). A box preparation was extended 1 mm beyond the cementoenamel junction on the distal aspect, leaving the margins on the dentin/cementum16,34 [Figure 1].
Teeth were etched using a selective etching technique. The enamel was totally-etched using 37% phosphoric acid for 15 seconds, followed by self-etching the dentin using Xeno® IV One Component dental adhesive (Dentsply Sirona, York, PA, USA). The adhesive was applied to both enamel and dentin in a generous layer, scrubbed on dentin for 15 seconds, then air-dried gently for 5 seconds to remove all solvents, and then light-cured for 20 seconds. Each group was restored following the manufacturer’s instructions for each corresponding CR; bulk-fill in the bulk of 4 mm each layer and the CC using a layering technique of 2 mm each. Bulk-fill restorations were cured at the occlusal (two overlapping exposures, one mesially-oriented, and one distally-oriented, to ensure full exposure of the occlusal surface), mesial, and distal surfaces for 40 seconds each using a light-emitting diode (LED) light (Bluephase N®, Ivoclar Vivadent, 1140 mW/cm2). While CC was cured for 30 seconds each layer, each composite restoration was finished and polished by 3M™ Sof-Lex™ XT discs (3M ESPE, St. Paul, MN, USA), starting with medium-coarse, then fine, then extra-fine discs.
The aging procedure was conducted through thermocycling and cyclic loading. A total of 5000 thermal cycles (based on the recommendation by the International Organization for Standardization)35 were performed between 5 °C and 55 °C in deionized water with a 30-second dwell time.35–37 Cyclic loading was conducted using a chewing simulator (SD Mechatronic, Feldkirchen-Westerham, Germany); the load was produced by weights mounted on vertical bars on a traverse with an individual weight configuration. Utilizing a computer-controlled servo motor,38 the load used was 20 kg (~200 N) for 250 000 cycles [Figure 2].
Teeth were mounted in clear-acrylic blocks; blocks were marked on one side to ensure exact positioning in the scanner. Teeth were scanned using µ-CT (SkyScan 1176, Bruker-microCT, Kontich, Belgium) to measure the volumetric size of the gap at the tooth-restoration interface. Each tooth was scanned in 360° rotation, and the x-ray tube was operated at 50 kV and 800 µA using a 0.5 mm thick aluminum-copper filter with a resolution of 13.7 µm pixels. Series of cross-sectional images with a voxel size of 11.94 × 11.94 × 11.94 μm were selected using the SkyScan software (CTan version 1.11.10.0 for 2-D visualization). Images were then utilized to assemble 3D visualization of each sample using reconstruction software (NRecon V1.4.0; SkyScan b.v.b.a.). The scan was conducted before restoration, immediately after restoration placement, and after the aging procedure. A qualitative evaluation of the gap was calculated by superimposing each sample’s before and after 3D visualization then measuring the gap volume change.
The quantitative data were entered into a computer and analyzed using SPSS (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). Descriptive analyses (mean±standard deviation (SD)) were undertaken to present an overview of the findings. The Wilcoxon signed-rank test and two-way analysis of variance (ANOVA) were used in testing statistical significance. The level of statistical significance was set at α = 0.05.
Results
The mean gap volume before aging is shown in Figure 3 for enamel and Figure 4 for dentin. The mean gap volume was highest in FBF with enamel margins (0.379), followed by TBF with enamel (0.326), FBF with dentin (0.390), CC with dentin (0.179), TBF with dentin (0.335), CC with enamel (0.175), SDR with enamel (0.069), followed by SDR with dentin (0.074).
The mean gap volume increased for all groups after aging; the Wilcoxon signed-rank test showed statistically significant differences between marginal gap sizes before and after aging for all groups (p < 0.050) except FBF with dentin (p > 0.050) [Table 1]. The greatest mean difference in gap volume for the tested RBC was seen in FBF with enamel (0.010), followed by CC with dentin (0.013), FBF with dentin (0.012), SDR with dentin (0.011), TBF with enamel (0.009), then TBF with dentin (0.008). The smallest mean difference in gap volume was seen in SDR with enamel (0.004) [Table 1; Figure 3 and Table 2; Figure 4].
Table 3: Two-way interaction between surface, aging, and material.
|
Corrected model |
1.404a |
15 |
0.094 |
3.369 |
< 0.001 |
|
Intercept |
5.541 |
1 |
5.541 |
199.449 |
< 0.001 |
|
S |
0.040 |
1 |
0.040 |
1.451 |
0.231 |
|
M |
1.191 |
3 |
0.397 |
14.297 |
< 0.001 |
aadjusted R squared. S: surface (enamel and dentin); M: material.
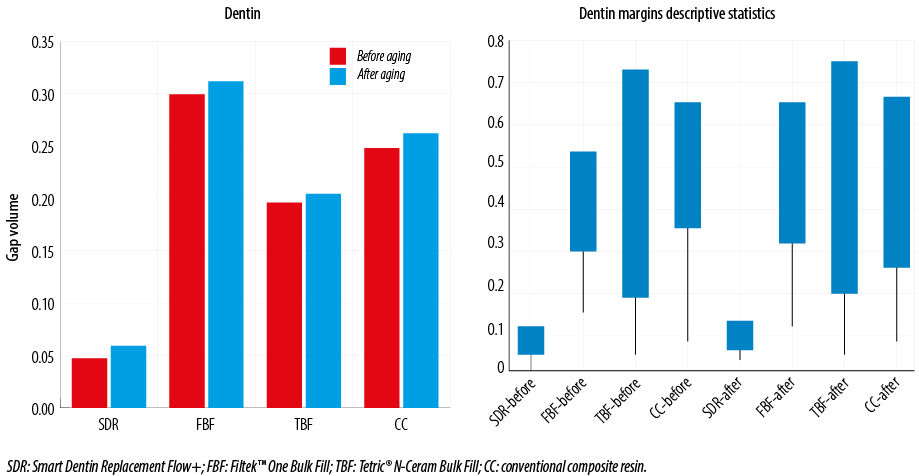
Figure 4: The volumetric width of the interfacial gap at the dentin-restoration interface before and after aging and dentin margins-gap descriptive statistics.
Two-way ANOVA revealed a statistically significant difference in the mean gap volume of the four materials before and after aging (p < 0.001) but no statistically significant interaction between study factors; surface, aging, and material (p > 0.050) [Table 3].
Discussion
The null hypothesis was rejected. The tested RBCs behaved differently upon aging regarding the gap at the tooth-restoration interface.
The use of µ-CT imaging proved useful in measuring restorative adaptation. Unlike other analytical methods that require sample sectioning at multiple time points, µ-CT imaging permits nondestructive evaluation of marginal gaps at different treatment periods; for example, immediately after polymerization and after aging, as in this study [Figure 5].
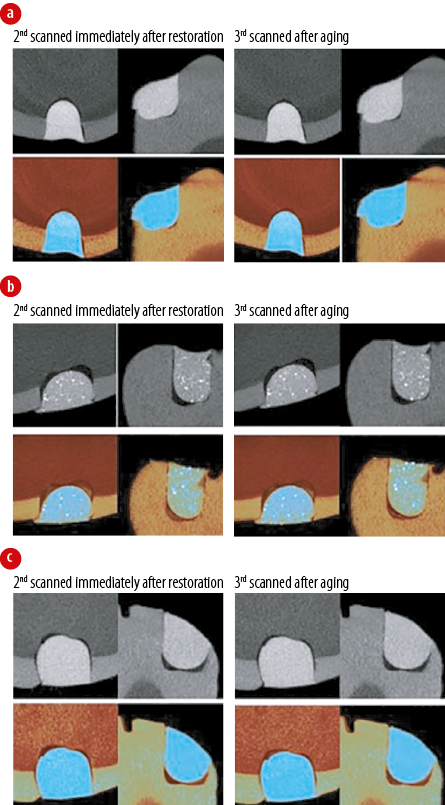
Figure 5: µ-CT imaging of samples immediately after restoration and then after aging, (a) Smart Dentin Replacement Flow+, (b) Filtek™ One Bulk Fill, and (c) conventional composite resin.
A marginal gap, or failure to attain intimate adaptation, adversely affects restoration longevity and clinical performance; it can be responsible for post-operative pain and sensitivity, marginal discoloration, recurrent caries, and failure or loss of the restoration.39,40 Marginal gaps result from an interaction between multiple factors, including the resin composite, cavity design, and restorative procedures. Marginal gap volume is proportional to the polymerization shrinkage value and the resin composite’s modulus of elasticity. Polymerization shrinkage generates stress at the tooth-restoration interface due to the modulus of elasticity and strain; greater polymerization shrinkage results in a larger gap.41,42 A material with a low modulus can compensate for the shrinkage by partially releasing the polymerization stress.32,43,44
In this study, factors affecting polymerization shrinkage and gap formation other than the composite were kept constant. Care was taken during cavity preparation to standardize cavity design and dimensions to keep the c-factor the same. A standard adhesive technique with a universal single-bond system was used for all restorations. All samples were light-cured for 40 seconds at all relevant tooth aspects (occlusal, mesial, and distal); increasing the light-curing duration to ≥ 30 seconds, which is longer than manufacturer recommendations, may improve composite polymerization and is recommended by some reports.16,45
There was no significant interaction between tooth surface, material, or aging. SDR showed the lowest mean gap volume of all tested materials in both enamel and dentin before aging and in enamel after aging. FBF showed the highest gap in enamel and dentin before aging and the highest gap in enamel after aging. CC showed a high gap volume in dentin before and after aging. The smallest gap in enamel was presented by TBF. TBF, while showing a high gap volume in enamel, had the second-lowest volume in dentin before aging and the second-lowest in dentin after aging. These outcomes agree with those established by previously published studies.17,46
According to each manufacturer, the filler particle content by volume is 42.5% for FBF, 45% for SDR, 59.5% for CC, and 55% for TBF. Higher filler content typically reduces the amount of monomer, leading to less shrinkage and polymerization stress. FBF and CC showed shrinkage correlates to the filler content but not the SDR. SDR contains a polymerization modulator in the resin’s backbone that reduces polymerization stress. This may explain the smaller gap volumes of SDR restorations detected in this investigation and in previous studies that reported greater marginal integrity using SDR compared to conventionally-layered composites.47–49
TBF exhibited better results in dentin than enamel, producing the lowest dentinal gap volume after aging. TBF contains a patented light activator called Ivocerin® with a higher absorption spectrum (range: 350–470 nm), and thus greater photocuring activity than camphorquinone (CQ). This improved the ability to polymerize deep sites during light-curing, may contribute to the positive TBF marginal results in dentin.50
It has been reported that when used as a base material, a flowable composite can absorb the impact of mechanical loading due to its lower flexural moduli, resulting in better marginal adaptation upon function.16,51–53 Similarly, this study determined that SDR and TBF, both flowable bulk-fill RCs, produced the smallest marginal gaps in dentin.
The marginal gaps were more severe in enamel than dentin before and after aging in all groups except for CC. Given that all other factors were kept constant, enamel-dentin discrepancies may be attributed to the modulus of elasticity of each RC used (ranging from 4-5 to 10-11 GPa) closer to dentin than enamel. The comparable moduli of dentin elasticity and resin improve marginal adaptation and adhesive bonding during function (aging), whereas a greater mismatch, seen at the enamel and composite interface, leads to partial debonding and wider gaps.31,46,47,54 Some published literature agrees with this finding. However, one study showed a contradictory outcome—wider gaps at the dentin margins—that may be due to its inclusion of variable class II cavity designs and involved surfaces (mesio-occlusal, disto-occlusal, and MOD) as well as differences in the duration of thermo-mechanical loading.49
A randomized clinical trial is an ultimate method for evaluating the real-life performance of restorations; it is a highly demanding study to conduct, requiring significant funding, participant availability, and compliance. The massive number of new composite materials released into the market complicates matters. In vitro models allow for wide-range screening of materials, highlighting ones with the most practical potential that can be further tested in a controlled clinical trial.
In the current in vitro study, restorations were subjected to thermocycling and cyclic loading to reproduce the stresses that these restorations undergo in the oral cavity during the function. These stresses are generated by polymerization, masticatory load, and mismatched coefficients of thermal expansion and contraction. The findings agree with those published previously; high-viscosity bulk-fill composites demonstrate better dentin margin integrity than conventionally-layered ones. The marginal adaptation difference was more apparent post-aging.
Conclusion
This study revealed that the marginal gap was more significant in enamel than dentin for all tested bulk-fill CR. Compared to CC, bulk-fill composites exhibited better bonding to dentin after aging. Based on in vitro results, the use of bulk-fill instead of conventionally-layered composites in deep class II cavities involving dentin may produce better marginal adaptation upon function. Further clinical study is required to determine the practical, long-term impact of bulk-filled composites, and evaluate the marginal adaptation and clinical performance of high-viscosity bulk-fill composites.
Disclosure
The author declared no conflicts of interest. No funding was received for this study.
references
- 1. Bowen RL, Chandler HH. Metal-filled resin composites. J Dent Res 1973 May-Jun;52(3):522-532.
- 2. Bowen RL, Chandler HH, Wyckoff HO Jr, Misra DN. Metal-filled resin composites. II. J Dent Res 1978 Feb;57(2):213-220.
- 3. Davidson CL, de Gee AJ, Feilzer A. The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res 1984 Dec;63(12):1396-1399.
- 4. Özcan M, Pekkan G. Effect of different adhesion strategies on bond strength of resin composite to composite-dentin complex. Oper Dent 2013 Jan-Feb;38(1):63-72.
- 5. Pinna R, Usai P, Filigheddu E, Garcia-Godoy F, Milia E. The role of adhesive materials and oral biofilm in the failure of adhesive resin restorations. Am J Dent 2017 Oct;30(5):285-292.
- 6. Szczesio-Wlodarczyk A, Sokolowski J, Kleczewska J, Bociong K. Ageing of dental composites based on methacrylate resins-a critical review of the causes and method of assessment. Polymers (Basel) 2020 Apr;12(4):E882.
- 7. Soares CJ, Faria-E-Silva AL, Rodrigues MP, Vilela AB, Pfeifer CS, Tantbirojn D, et al. Polymerization shrinkage stress of CRs and resin cements - What do we need to know? Braz Oral Res 2017 Aug;31(suppl 1):e62.
- 8. Campodonico CE, Tantbirojn D, Olin PS, Versluis A. Cuspal deflection and depth of cure in resin-based composite restorations filled by using bulk, incremental and transtooth-illumination techniques. Journal of the American Dental Association 2011;142(10):1176-1182.
- 9. Oglakci B, Kazak M, Donmez N, Dalkilic EE, Koymen SS. The use of a liner under different bulk-fill resin composites: 3D GAP formation analysis by x-ray microcomputed tomography. J Appl Oral Sci 2019 Nov;28:e20190042.
- 10. Pereira R, Bicalho AA, Franco SD, Tantbirojn D, Versluis A, Soares CJ. Effect of restorative protocol on cuspal strain and residual stress in endodontically treated molars. Oper Dent 2016 Jan-Feb;41(1):23-33.
- 11. Oliveira LR, Braga SS, Bicalho AA, Ribeiro MT, Price RB, Soares CJ. Molar cusp deformation evaluated by micro-CT and enamel crack formation to compare incremental and bulk-filling techniques. J Dent 2018 Jul;74:71-78.
- 12. Rosatto CM, Bicalho AA, Veríssimo C, Bragança GF, Rodrigues MP, Tantbirojn D, et al. Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. J Dent 2015 Dec;43(12):1519-1528.
- 13. Azevedo LM, Casas-Apayco LC, Villavicencio Espinoza CA, Wang L, Navarro MF, Atta MT. Effect of resin-modified glass-ionomer cement lining and composite layering technique on the adhesive interface of lateral wall. Journal of applied oral science 2015;23(3):315-320.
- 14. Mount GJ. Clinical requirements for a successful ‘sandwich’–dentine to glass ionomer cement to CR. Aust Dent J 1989 Jun;34(3):259-265.
- 15. Spencer P, Ye Q, Park J, Topp EM, Misra A, Marangos O, et al. Adhesive/Dentin interface: the weak link in the composite restoration. Ann Biomed Eng 2010 Jun;38(6):1989-2003.
- 16. Jung JH, Park SH. Comparison of polymerization shrinkage, physical properties, and marginal adaptation of flowable and restorative bulk fill RBC. Oper Dent 2017 Jul/Aug;42(4):375-386.
- 17. Kim RJ, Kim YJ, Choi NS, Lee IB. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J Dent 2015 Apr;43(4):430-439.
- 18. Kim YJ, Kim R, Ferracane JL, Lee IB. Influence of the compliance and layering method on the wall deflection of simulated cavities in bulk-fill composite restoration. Oper Dent 2016 Nov/Dec;41(6):e183-e194.
- 19. Aggarwal V, Singla M, Yadav S, Yadav H. Effect of flowable composite liner and glass ionomer liner on class II gingival marginal adaptation of direct composite restorations with different bonding strategies. J Dent 2014 May;42(5):619-625.
- 20. Oliveira LC, Duarte S Jr, Araujo CA, Abrahão A. Effect of low-elastic modulus liner and base as stress-absorbing layer in CR restorations. Dent Mater 2010 Mar;26(3):e159-e169.
- 21. Behery H, El-Mowafy O, El-Badrawy W, Saleh B, Nabih S. Cuspal deflection of premolars restored with bulk-fill CRs. Journal of Esthetic and Restorative Dentistry 2016;28(2):122-130.
- 22. Ilie N. Comparative effect of self- or dual-curing on polymerization kinetics and mechanical properties in a novel, dental-resin-based composite with alkaline filler. Materials 2018;11(1):108.
- 23. Cidreira Boaro LC, Pereira Lopes D, de Souza AS, Lie Nakano E, Ayala Perez MD, Pfeifer CS, et al. Clinical performance and chemical-physical properties of bulk fill composites resin -a systematic review and meta-analysis. Dent Mater 2019 Oct;35(10):e249-e264.
- 24. Orłowski M, Tarczydło B, Chałas R. Evaluation of marginal integrity of four bulk-fill dental composite materials: in vitro study. ScientificWorldJournal 2015;2015:701262.
- 25. Xue J. [Factors influencing clinical application of bulk-fill CR]. Hua Xi Kou Qiang Yi Xue Za Zhi 2020 Jun;38(3):233-239.
- 26. Gerdolle DA, Mortier E, Droz D. Microleakage and polymerization shrinkage of various polymer restorative materials. J Dent Child (Chic) 2008 May-Aug;75(2):125-133.
- 27. Nahedh HA, Sibai NS. Evaluation of interfacial gap volume of two low-shrinkage composites using micro-computed tomography. Oper Dent 2017 Nov/Dec;42(6):658-668.
- 28. Rizzante FA, Sedky RA, Furuse AY, Teich S, Ishikiriama SK, Mendonça G. Validation of a method of quantifying 3D leakage in dental restorations. J Prosthet Dent 2020;123(6):839-844.
- 29. Ausiello P, Ciaramella S, Garcia-Godoy F, Martorelli M, Sorrentino R, Gloria A. Stress distribution of bulk-fill resin composite in class II restorations. Am J Dent 2017 Aug;30(4):227-232.
- 30. Ausiello P, Ciaramella S, Fabianelli A, Gloria A, Martorelli M, Lanzotti A, et al. Mechanical behavior of bulk direct composite versus block composite and lithium disilicate indirect Class II restorations by CAD-FEM modeling. Dental Materials 2017;33(6):690-701.
- 31. Ilie N, Bucuta S, Draenert M. Bulk-fill RBC: an in vitro assessment of their mechanical performance. Oper Dent 2013 Nov-Dec;38(6):618-625.
- 32. Rizzante FA, Mondelli RF, Furuse AY, Borges AF, Mendonça G, Ishikiriama SK. Shrinkage stress and elastic modulus assessment of bulk-fill composites. J Appl Oral Sci 2019 Jan;27:e20180132.
- 33. Elshazly TM, Bourauel C, Aboushelib MN, Sherief DI, El-Korashy DI. The polymerization efficiency of a bulk-fill composite based on matrix-modification technology. Restor Dent Endod 2020 May;45(3):e32.
- 34. McHugh LEJ, Politi I, Al-Fodeh RS, Fleming GJP. Implications of resin-based composite (RBC) restoration on cuspal deflection and microleakage score in molar teeth: placement protocol and restorative material. Dental materials 2017;33(9):e329-e335.
- 35. International Organization for Standardization. ISO. Dental materials-testing of adhesion to tooth structure. Geneva, Switzerland: ISO; 2003.
- 36. Rinastiti M, Özcan M, Siswomihardjo W, Busscher HJ. Effects of surface conditioning on repair bond strengths of non-aged and aged microhybrid, nanohybrid, and nanofilled CRs. Clin Oral Investig 2011 Oct;15(5):625-633.
- 37. Kiomarsi N, Saburian P, Chiniforush N, Karazifard MJ, Hashemikamangar SS. Effect of thermocycling and surface treatment on repair bond strength of composite. J Clin Exp Dent 2017 Aug;9(8):e945-e951.
- 38. Kern M, Strub JR, Lü XY. Wear of CR veneering materials in a dual-axis chewing simulator. J Oral Rehabil 1999 May;26(5):372-378.
- 39. Savadi Oskoee S, Bahari M, Jafari Navimipour E, Ajami AA, Ghiasvand N, Savadi Oskoee A. Factors affecting marginal integrity of class II bulk-fill CR restorations. J Dent Res Dent Clin Dent Prospects 2017;11(2):101-109.
- 40. Schwendicke F, Kniess J, Paris S, Blunck U. Margin integrity and secondary caries of lined or non-lined composite and glass hybrid restorations after selective excavation in vitro. Oper Dent 2017 Mar/Apr;42(2):155-164.
- 41. Ferracane JL. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent Mater 2005 Jan;21(1):36-42.
- 42. Peutzfeldt A, Asmussen E. Determinants of in vitro gap formation of resin composites. J Dent 2004 Feb;32(2):109-115.
- 43. Suiter EA, Tantbirojn D, Watson LE, Yazdi H, Versluis A. Elastic modulus maturation effect on shrinkage stress in a primary molar restored with tooth-colored materials. Pediatr Dent 2018 Sep;40(5):370-374.
- 44. Vidal ML, Rego GF, Viana GM, Cabral LM, Souza JP, Silikas N, et al. Physical and chemical properties of model composites containing quaternary ammonium methacrylates. Dent Mater 2018 Jan;34(1):143-151.
- 45. Zorzin J, Maier E, Harre S, Fey T, Belli R, Lohbauer U, et al. Bulk-fill resin composites: polymerization properties and extended light curing. Dent Mater 2015 Mar;31(3):293-301.
- 46. Peutzfeldt A, Mühlebach S, Lussi A, Flury S. Marginal gap formation in approximal “bulk fill” resin composite restorations after artificial ageing. Oper Dent 2018 Mar/Apr;43(2):180-189.
- 47. Benetti AR, Peutzfeldt A, Lussi A, Flury S. Resin composites: modulus of elasticity and marginal quality. J Dent 2014 Sep;42(9):1185-1192.
- 48. Burgess J, Cakir D. Comparative properties of low-shrinkage CRs. Compend Contin Educ Dent 2010 May;31(Spec No 2):10-15.
- 49. Roggendorf MJ, Krämer N, Appelt A, Naumann M, Frankenberger R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J Dent 2011 Oct;39(10):643-647.
- 50. Moszner N, Fischer UK, Ganster B, Liska R, Rheinberger V. Benzoyl germanium derivatives as novel visible light photoinitiators for dental materials. Dent Mater 2008 Jul;24(7):901-907.
- 51. Kemp-Scholte CM, Davidson CL. Complete marginal seal of class V resin composite restorations effected by increased flexibility. J Dent Res 1990 Jun;69(6):1240-1243.
- 52. Kemp-Scholte CM, Davidson CL. Marginal integrity related to bond strength and strain capacity of CR restorative systems. J Prosthet Dent 1990 Dec;64(6):658-664.
- 53. Senawongse P, Pongprueksa P, Tagami J. The effect of the elastic modulus of low-viscosity resins on the microleakage of class V resin composite restorations under occlusal loading. Dent Mater J 2010 May;29(3):324-329.
- 54. Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G. Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent 2014 Aug;42(8):993-1000.