Condylar hyperplasia (CH) is a non-neoplastic pathology of unknown etiology resulting from excessive growth of the condyle head and/or neck. It presents clinically as a classical progressive unilateral facial asymmetry.1–4 Epidemiological data have shown a female predominance with theories suggestive of a possible role of estrogen hormone.2,5 Due to the continued excessive growth of the condyle, this pathological process can adversely affect the mandibular morphology, dental occlusion, temporomandibular joint function, and indirectly the maxillary growth.3,6 Clinical evaluation and imaging are essential tools for establishing an accurate diagnosis of CH.7–10
We present two cases of unilateral CH in female patients diagnosed and managed at our center with different surgical options, both with satisfactory outcome.
Case report
Case one
A 17-year-old female presented to the Oral and Maxillofacial Surgery Department at Al Nahdha Hospital, Oman, in February 2012 complaining of progressive facial asymmetry over the past two years. Clinical examination showed marked facial asymmetry with chin deviation to the right side and mild mandibular prognathism [Figure 1a]. Intraorally, she had a midline shift of 11 mm to the right and a reverse overjet, which was more marked on the right side. In addition, there was an anterior open bite in relation to the left upper lateral incisor [Figure 1b]. Radiographic examinations showed a discrepancy between the left and right sides of the mandible with a 6 mm elongation of the left condylar neck. The ramus was elongated downwards and forwards with no effects on the coronoid process [Figure 1c]. Bone scan using technetium-99m showed a significant increase in the condylar uptake on the left side [Figure 1d], confirming the diagnosis of active left CH (type 1B as per Wolford’s classification of CH).
Due to the disturbed psychosocial status of the patient, there was an urgent need for treatment; therefore, the patient underwent left proportional condylectomy with removal of 6 mm of the condylar head. Postoperatively, clinical reviews showed significant improvement of the facial profile with good facial symmetry and dental alignment. The patient was referred for orthodontic treatment to further facilitate the correction of the minor dental discrepancy, but the patient opted to reject the orthodontic treatment as she was happy with the outcome. Five years follow-up showed stable skeletal and dental results [Figure 1e–g].
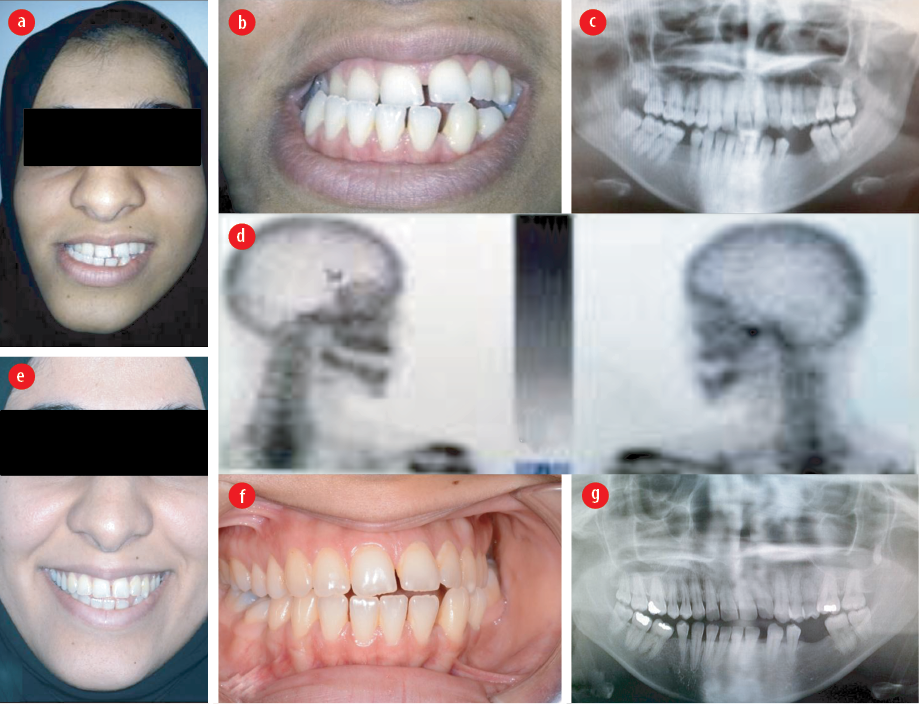
Figure 1: Case 1 (a) preoperative frontal photograph showing asymmetrical face with chin deviation to the right side, (b) anterior dental view showing occlusal discrepancy, (c) technetium-99m scintigraphy showing the continued growth of the left condyle, and (d) preoperative orthopantomogram (OPG) showing elongation of the left condylar neck. (e) Four years postoperative frontal view showing symmetrical face with improved appearance, and (f) dental view showing marked improvement in dental occlusion and a residual minor anterior dental discrepancy. (g) Postoperative OPG showing bilateral symmetrical condyles and rami segments.
Case two
A 29-year-old female presented to the Oral Surgery Department at Oman Dental College in October 2017 complaining of facial asymmetry that was noticed by the patient over many years [Figure 2a]. The patient had a history of minor trauma to the left side of the face without fractures. Clinical examination revealed marked facial asymmetry and chin deviation to the left side.
Clinically, there was an 8 mm left midline shift and a left posterior crossbite [Figure 2b]. Radiographic assessments showed marked elongation of the right condyle, and the technetium-99m bone scan showed inactivity of the condylar growth [Figure 2c and d]. Based on the clinical and medical imaging, inactive right CH was confirmed, and the patient was planned for combined orthodontic-orthognathic surgery treatment.

Figure 2: Case 2 (a) clinical photograph showing asymmetrical face with chin deviation to the left side, (b) anterior dental view showing occlusal discrepancy with midline shift to the left side, (c) technetium-99m scintigraphy showing cessation of condylar growth, and (d) an orthopantomogram showing elongation of the right condylar neck.
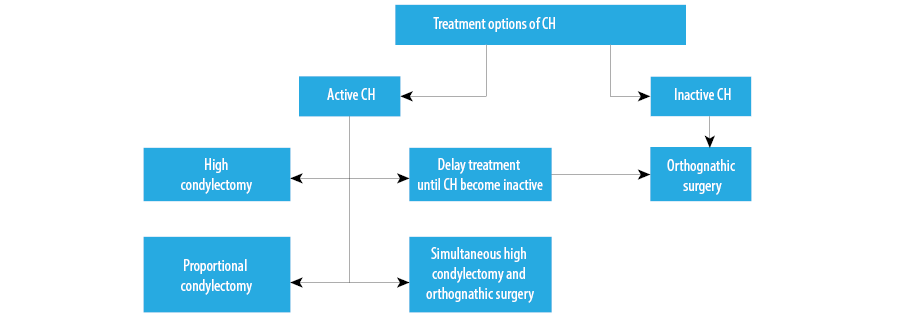
Figure 3: Diagram summarizing treatment options of condylar hyperplasia (CH).
Discussion
The mandibular condyle is a known center of growth in the facial skeleton.4 Studies showed that 99% of the facial growth is completed at the age of 15 and 18 years in females and males, respectively. CH occurs at an equal rate in males and females as well as unilateral and bilateral.11–13 CH represents a disorder where the growth of the condyle continues beyond the normal growth period.14 Previous literature has shown that CH often presents in the second or third decades of life and more commonly affects women than men.2,5 Raijmakers et al,12 conducted a meta-analysis in 2012, which revealed that women develop CH significantly more frequently (64%). However, there was no evidence to suggest that the side affected by CH was linked to sex.12 Our cases are consistent with previous case reports in terms of age at presentation and gender.
There is a lot of ambiguity surrounding the etiology of CH. Extrinsic and intrinsic factors have been suggested in association with the development of CH. The suggested intrinsic factors include alteration of the condylar vascularization, hormonal disorders, and cartilaginous hypertrophy. The extrinsic factors include micro-trauma and infections.8,9 The suggested factors may act as initiating factor for the disease process, but the exact pathogenesis remain unclear.
Obwegesr and Makek published a classification system of CH in 1986, which was based on asymmetry and growth vector.5 More recently, Wolford et al,15 proposed a simpler classification system based on the suggestion of CH being a pathological condition causing an over development of the condylar head and/or neck of the mandible. The proposed classification is made of four subtypes. Our presented cases are classified as type 1B, which comprises a unilateral asymmetric abnormal condylar overgrowth, leaving an obvious asymmetrical condyle, chin deviation towards the contralateral side, and facial asymmetry.
Accurate diagnosis of CH is essential for proper treatment. Many diagnostic methods are available, including clinical examination, orthopantomogram (OPG), and nuclear imaging. Clinical examination and OPG assessment are often referred to as the gold standard in making the correct diagnosis. However, they do not provide any valuable information regarding the burnout or staging of condylar hyperactivity.7,9,11,16 Nuclear imaging, which includes scintigraphy (technetium-99m), single-photon emission computed tomography, and positron emission tomography, provides detailed information on the condylar activity and cessation of growth, thus assisting the formulation of an appropriate
treatment plan.8–10,16,17
Different treatment protocols have been suggested in the literature for the management of CH [Figure3].18–20 Before determining the type of treatment, careful assessment and consideration should be given to the patient’s age, the activity status of the condyle, level of facial asymmetry and occlusal discrepancy, and the patient’s psychological status.6,18,21,22 Published studies have confirmed that condylectomy is recommended in patients with continued active growth of CH.18,19 On the other hand, orthognathic surgery is the more appropriate surgical management in cases of inactive CH.21
There is no consensus regarding the optimal timing for the surgical treatment of CH. Some studies suggested deferring the treatment until the activity of the CH has arrested then performing the corrective orthognathic surgery. However, this may cause the patient to suffer from a functional problem, worsening the esthetic and the psychosocial stigmata associated with a facial deformity.18,19 Nowadays, there is good support from published studies for early surgical interventions, which mainly entails high condylectomy or, more recently, proportional condylectomy.6,21,22 Wolford et al,18,19 advocated that early high condylectomy, at the age of 15 years in females and 17–18 years in males, is regarded as a minor intervention where 3–5 mm is removed from the upper part of the condylar head. This intervention often leads to excellent esthetic and good functional outcome. Another treatment modality suggested in the literature is the simultaneous combination of high condylectomy and orthognathic surgery, which is thought to reduce further needs for surgical intervention. However, recent studies showed a risk of relapse associated with this treatment modality that was seen more in the maxilla than the mandible, thus requiring secondary surgical intervention.18,19 More recently, Fariña et al,20 showed that proportional condylectomy is superior to high condylectomy due to the low need for further corrective orthognathic surgery (16% for proportional condylectomy compared to 91% for high condylectomy). Proportional condylectomy entails the removal of the difference observed between the hyperplastic and the opposing healthy condyle. The amount removed is usually estimated based on preoperative OPG.
In our first reported case, the CH lesion was active, and due to the overwhelming psychosocial issues with the patient, a proportional condylectomy was performed, which resulted in a successful outcome and satisfactory result at four-years follow-up, obviating the need for further surgical intervention. However, in the second case, as the CH was inactive, the patient is currently undergoing orthodontic-
orthognathic treatment.
Conclusion
CH is a relatively rare idiopathic condition affecting the mandibular condyle. Careful assessment and investigations are essential before formulating an appropriate treatment plan that should consider the patient’s needs and the condyle growth status.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Kim JY, Ha TW, Park JH, Jung HD, Jung YS. Condylectomy as the treatment for active unilateral condylar hyperplasia of the mandible and severe facial asymmetry: retrospective review over 18 years. Int J Oral Maxillofac Surg 2019 Dec;48(12):1542-1551.
- 2. Obwegeser HL. Mandibular growth anomalies terminology- aetiology diagnosis- treatment. Berlin, Heidelberg: Spriner Berlin Heidelberg; 2001.
- 3. Wolford LM. Mandibular asymmetry: temporomandibular joint degeneration. In: Bagheri SC, Bell RB, Khan HA, editors. Current therapy in oral and maxillofacial surgery. St Louis (MO); 2012. p. 696-725.
- 4. Nitzan DW, Katsnelson A, Bermanis I, Brin I, Casap N. The clinical characteristics of condylar hyperplasia: experience with 61 patients. J Oral Maxillofac Surg 2008 Feb;66(2):312-318.
- 5. Obwegeser HL, Makek MS. Hemimandibular hyperplasia–hemimandibular elongation. J Maxillofac Surg 1986 Aug;14(4):183-208.
- 6. Marchetti C, Cocchi R, Gentile L, Bianchi A. Hemimandibular hyperplasia: treatment strategies. J Craniofac Surg 2000 Jan;11(1):46-53.
- 7. Saridin CP, Raijmakers PG, Tuinzing DB, Becking AG. Bone scintigraphy as a diagnostic method in unilateral hyperactivity of the mandibular condyles: a review and meta-analysis of the literature. Int J Oral Maxillofac Surg 2011 Jan;40(1):11-17.
- 8. Abboud WA, Krichmar M, Blinder D, Dobriyan A, Yahalom G, Yahalom R. Three-dimensional orofacial changes occurring after propotional condylectomy in patients with condylar hyperplasia type 1B unilateral himimandibular elongation. J Oral Maxillofac Surg 2019 Apr;77(4):803-817.
- 9. Chan WL, Carolan MG, Fernandes VB, Abbati DP. Planar versus SPET imaging in the assessment of condylar growth. Nucl Med Commun 2000 Mar;21(3):285-290.
- 10. Fariña RA, Becar M, Plaza C, Espinoza I, Franco ME. Correlation between single photon emission computed tomography, AgNOR count, and histomorphologic features in patients with active mandibular condylar hyperplasia. J Oral Maxillofac Surg 2011 Feb;69(2):356-361.
- 11. Rodrigues DB, Castro V. Condylar hyperplasia of the temporomandibular joint: types, treatment, and surgical implications. Oral Maxillofac Surg Clin North Am 2015 Feb;27(1):155-167.
- 12. Raijmakers PG, Karssemakers LH, Tuinzing DB. Female predominance and effect of gender on unilateral condylar hyperplasia: a review and meta-analysis. J Oral Maxillofac Surg 2012 Jan;70(1):e72-e76.
- 13. Bharathi SC,Senthilnathan S, Kumar LD, Mohan AC, Taranath M.Unilateral condylar hyperplasia: A case report and review of literature. JISPCD 2014 Jan 4(1):67-70.
- 14. Arora KS, Bansal R, Mohapatra S, Pareek S. Review and Classification Update: Unilateral condylar hyperplasia. BMJ Case Rep 2019 Feb;12(2):bcr-2018.
- 15. Wolford LM, Movahed R, Perez DE. A classification system for conditions causing condylar hyperplasia. J Oral Maxillofac Surg 2014 Mar;72(3):567-595.
- 16. Pripatnanont P, Vittayakittipong P, Markmanee U, Thongmak S, Yipintsoi T. The use of SPECT to evaluate growth cessation of the mandible in unilateral condylar hyperplasia. Int J Oral Maxillofac Surg 2005 Jun;34(4):364-368.
- 17. Laverick S, Bounds G, Wong WL. [18F]-fluoride positron emission tomography for imaging condylar hyperplasia. Br J Oral Maxillofac Surg 2009 Apr;47(3):196-199.
- 18. Wolford LM, Mehra P, Reiche-Fischel O, Morales-Ryan CA, García-Morales P. Efficacy of high condylectomy for management of condylar hyperplasia. Am J Orthod Dentofacial Orthop 2002 Feb;121(2):136-150.
- 19. Wolford LM, Morales-Ryan CA, García-Morales P, Perez D. Surgical management of mandibular condylar hyperplasia type 1. Proc (Bayl Univ Med Cent) 2009 Oct;22(4):321-329.
- 20. Fariña R, Pintor F, Pérez J, Pantoja R, Berner D. Low condylectomy as the sole treatment for active condylar hyperplasia: facial, occlusal and skeletal changes. An observational study. Int J Oral Maxillofac Surg 2015 Feb;44(2):217-225.
- 21. Wolford LM, Movahed R, Dhameja A, Allen WR. Low condylectomy and orthognathic surgery to treat mandibular condylar osteochondroma: a retrospective review of 37 cases. J Oral Maxillofac Surg 2014 Sep;72(9):1704-1728.
- 22. Jones RH, Tier GA. Correction of facial asymmetry as a result of unilateral condylar hyperplasia. J Oral Maxillofac Surg 2012 Jun;70(6):1413-1425.