A 16-year-old girl presented with progressive left neck swelling of six weeks duration associated with low-grade fever and rash [Figure 1]. Four weeks before visiting our institute, she was started on antibiotics combined with non-steroidal anti-inflammatory drugs (NSAIDs) prescribed by a doctor from a local health center. As a result, her pain resolved while the size of the swelling had an interval regression followed by rebound enlargement. Clinical examination revealed unilateral multiple non-tender enlarged left cervical lymphadenopathy involving level II to V with normal overlaying skin. The rest of her examination was unremarkable including upper aero-digestive endoscopy. These findings were demonstrated with further details with a computed tomography (CT) scan [Figure 2]. She had mild microcytic hypochromic anemia with normal iron profile, folate, and B12. Further laboratory findings showed a white blood cell count of 4.0 × 109/L, C-reactive protein (CRP) < 1 mg/L, erythrocyte sedimentation rate (ESR) 31 mm/hour, and lactate dehydrogenase (LDH) 288 U/L. An excisional biopsy of the swelling was taken for histopathological examination, which revealed areas of necrosis with histiocytic proliferation without granulomas [Figure 3]. The histiocytes were positive for CD68 and myeloperoxidase (MPO).

Figure 1: Rash on the arms of a 16-year-old female.

Figure 2: CT scan revealed enlarged left cervical lymph nodes.
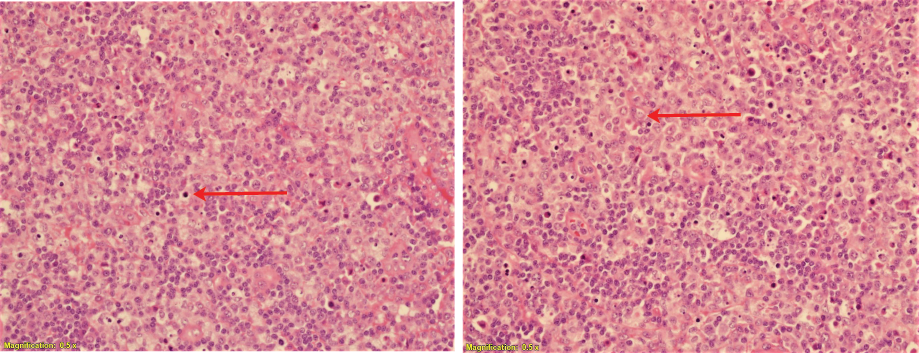
Figure 3: Excisional biopsy revealed predominant histiocytic cells, apoptotic cells, and lymphocytic cells. Hematoxylin and eosin stain, magnification = 0.5 ×.
Questions
- What is the most likely diagnosis?
a. Suppurative bacterial lymphadenitis.
b. Tuberculous lymphadenitis.
c. Histiocytic necrotizing lymphadenitis.
(Kikuchi-Fujimoto disease).
d. Autoimmune related lymphadenitis.
e. Lymphoma.
f. Secondary metastatic lymphadenopathy.
- Which of the following is a treatment option?
a. Supportive care.
b. NSAIDs.
c. Steroids.
d. Intravenous immunoglobulin.
e. All of the above.
f. None of the above.
Answers
1. c. Histiocytic necrotizing lymphadenitis.
2. e. All of the above.
Discussion
Histiocytic necrotizing lymphadenitis, commonly known as Kikuchi-Fujimoto disease, is a rare condition with a typically benign course. Infective triggers and autoimmune association have been described in the literature; however, its etiology is yet to be identified. In 1972, Kikuchi and Fujimoto laid the bases of this diagnostic entity. This disease tends to affect young female adults of Asian origin. Fever and neck swelling are the most common presenting complaints, while unilateral cervical lymphadenopathy is the most common detectable sign. However, it can affect almost all systems. Rash and constitutional symptoms are also common.1–3
On basic metabolic panel, it is not uncommon to find patients have mild granulocytopenia with elevated ESR. LDH and CRP may also be elevated.Primarily, it is necessary to exclude all infective and non-infective lymphadenitis with other detailed investigation as per clinical input guidance. In CT scan imaging, the lymphadenopathy in Kikuchi-Fujimoto disease has peripheral enhancement with central hypoattenuation suggestive of central necrosis with absence of calcification. Lymph node biopsy is necessary to exclude primary hematopoietic malignancy or secondary metastatic malignancy.3,4
The distinctive features of histopathological examination include, scattered apoptotic cells (areas of necrosis) with predominant histiocytic and lymphocytic infiltrate, and absent neutrophilic cells. T-lymphocyte (CD3/CD8), histiocyte (CD68/PGM-1), and MPO are the immunohistochemical markers of this condition.1,3 The usual course of the disease is to resolve spontaneously or with help of medications, which takes two weeks to four months. However, there have been cases reported with serious complications that patient may experience, namely hemophagocytic lymphohistiocytosis. There is no standardized treatment yet, nevertheless, it can range from supportive care with NSAIDs to steroids and immunomodulators such as hydroxychloroquine.3,5
references
- 1. Lo KB, Papazoglou A, Chua L, Candelario N. Case report: kikuchi: the great mimicker. F1000Res 2018 Apr;7:520.
- 2. Chang C, Lin SH, Medeiros LJ, Chang KC. Kikuchi disease: an unusual case with features suggesting an infectious aetiology. Pathology 2018 Oct;50(6):694-697.
- 3. Fidai SS, Cipriani NA, Ginat DT. Histiocytic necrotizing lymphadenitis involving the neck: radiology-pathology correlation. Head Neck Pathol 2018. Dec:13(4):648-651.
- 4. Rakesh P, Alex RG, Varghese GM, Mathew P, David T, Manipadam MT, et al. Kikuchi-fujimoto disease: clinical and laboratory characteristics and outcome. J Glob Infect Dis 2014 Oct;6(4):147-150.
- 5. Lelii M, Senatore L, Amodeo I, Pinzani R, Torretta S, Fiori S, et al. Kikuchi-Fujimoto disease in children: two case reports and a review of the literature. Ital J Pediatr 2018 Jul;44(1):83.