Dental caries is a prevalent disease, which is mainly associated with consuming foods containing high levels of free sugars. Caries affect the majority of the adult population around the world.1,2 For instance, in the US, 92% of adults have had tooth decay,3 indicating a need to develop interventions that can help to reduce the prevalence of dental caries among the adult population. Approaches to the prevention of caries include the application of appropriate plaque control methods and reducing the overall intake and frequency of eating free sugars.4,5 Evidence shows that control of free sugars intake contributes to a reduction in the prevalence of dental caries.1,2,4,6–11 The relative importance of free sugars intake frequency versus the total amount of sugary food eaten is debatable. Some suggest that the overall intake of sugary food plays a major role in caries progression,4,8 whereas others emphasize frequency rather than total intake.4,12 The Scientific Advisory Committee on Nutrition (SACN) in the UK concluded from a systematic literature review that there are limited studies that assess the frequency of free sugars intake and the relationship between frequency of free sugars intake and dental caries, and as a result were unable to determine the relationship between the two variables.13 In addition, the committee found moderate evidence in the relationship between overall free sugars intake and dental caries. Therefore, they made a strong recommendation to reduce the total intake of free sugars. This recommendation will reduce not only dental caries but also other systemic diseases as a common risk factor.14 Based on the results of the SACN review,13 this literature review focuses on tackling total free sugars intake rather than the frequency of intake.
The reduction of free sugars intake requires behavior change by individuals.15 Theories of behavior change are essential in the design of effective behavior change strategies.16–19 Interventions based on such models are better at predicting behavior change than non-theory-based interventions.20 Of these, four appear to be the most commonly used by the literature: Transtheoretical Model of change (TTM), Theory of Planned Behavior (TPB), Social Cognitive Theory (SCT), and the Information-Motivation-Behavioral Skills (IMB) model. In addition, a recent discussion of the weaknesses of the existing literature21 argued that the two models that most comprehensively capture the full range of factors that might influence behavior are PRIME Theory and The Behavior Change Wheel (BCW). This literature review discusses the application of each of the six common behavior change theories in predicting behaviors and developing interventions related to general and oral health and hypothesized their use in reducing free sugar intake related to dental caries among adults.
To achieve this, we have outlined the key features of each of the six behavior change theories and reviewed their usefulness in general and oral health-related behavior and possible future application in reducing sugars intake. Generally, the use of psychological models, including social cognition models, in behavior change interventions to reduce free sugars intake related to dental caries among adults is still under-research.22 Our review assists in identifying gaps in the literature providing a narrative review of the literature related to dental and general health. Overall, this literature review highlights whether behavior change models can be applied as predictors or behavior change agents to reduce free sugar intake among adults and if they can be used as theories to guide the development of interventions to reduce the intake of free sugar.
A wide range of methods have been used to change behavior, including oral health education, psychological models or theories, and behavior change frameworks.
Oral health education
Oral health education is an educational activity that aims to achieve oral health-related goals through increasing knowledge, which leads to change in attitude and ultimately changes the behavior.23 It is based on the three domains of learning: cognitive, affective, and behavioral.23 Oral health education has been a crucial and integral element of dental services for a century at different community levels.23 There are various means of applying oral health education, including mass media campaigns and school-based health education. Many studies have assessed the effectiveness of oral health education in improving behavior related to dental caries including four systematic reviews, which all demonstrate similar findings concerning the effectiveness of the traditional oral health education approach.24–28 In one systematic review, oral health education had no evidence in reducing dental caries incidence and ambiguous evidence of oral health education to improve diet control.24 Another review reported limited evidence to support oral health education reduces the incidence of dental caries.25
There is strong evidence to suggest that interventions based on behavior change models (such as motivational interviewing) help in improving gingival conditions and oral hygiene.26 In addition, there is strong evidence that educational written materials (e.g., leaflets) help improve patients’ knowledge, but no evidence of their influence on behavior. Finally, there is weak evidence to support the theory that improving knowledge leads to improved behaviors, and if there was any change in behaviors, it would be short term.24,26,27 A systematic review assessing the effectiveness of psychological intervention on improving oral hygiene compared with traditional oral health education among adults and adolescents reported a small statistically significant difference for interventions based on psychological models to decease plaque index compared with the traditional method.28 Also, they found interventions based on psychological models had a better outcome result in relation to oral health behavior and toothbrushing when compared with oral health education.28 The findings confirm that providing education or information about caries or diet alone is not sufficient to change behavior. This is because traditional oral health education programs do not consider other factors, which influence the behavior of individual, including environmental and social factors.25 For free sugars intake, oral health education alone is not sufficient to create a sustainable decrease in free sugar intake among adults. It can be used with other behavior change models such as the BCW, which is discussed below.
Transtheoretical Model (TTM)
The TTM, also known as the stages of change model, is a stage-based model that assumes that behavioral change needs to progress sequentially.29,30 Figure 1 presents the five stages of the TTM.
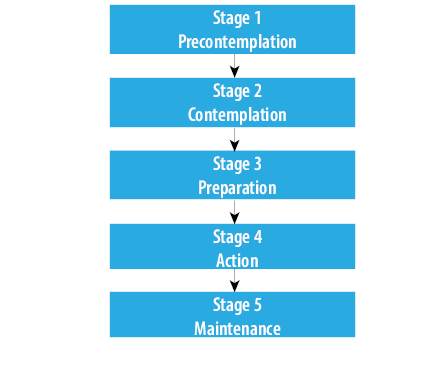
Figure 1: The five stages of the Transtheoretical Model.29
TTM has been applied to changing several health-related behaviors, including eating-related behaviors and smoking cessation. A number of studies assessed the effectiveness of TTM in improving health-related behaviors. A systematic review of 27 studies concluded that TTM was useful for understanding the decision-making processes regarding change for eating-related behaviors.31 Similarly, a systematic review of 15 studies found that TTM is useful in assessing motivation to change for individuals with eating disorders.32 Also, in favor of the model, a systematic review of 87 studies suggested that the TTM has been repeatedly validated and provides useful strategies for dietary behavior change and meaningful outcome measures.33 There is also evidence to support the use of TTM for smoking cessation. A systematic review of 41 randomized controlled trials (RCTs) found supporting evidence for the use of TTM for smoking cessation,34 and a further systematic review of 28 studies found that there was moderate evidence to support the use of TTM for smoking cessation in young people.35 There is strong evidence that the TTM improves smoking cessation in the long term.36
While there is ample support for TTM for eating-related behavior change and smoking cessation, there is little or no evidence that it is effective for other health-related behaviors such as physical activity. A review of three RCTs found no support for the efficacy to produce sustainable changes in weight loss.37 It appears that TTM may be effective only for certain health-related behavior changes, such as eating-related behaviors and smoking cessation, but ineffective for others, such as changes in physical activity. This may indicate that the TTM is applicable to certain health-related behaviors.
The TTM has been applied and assessed for a number of oral health behaviors (e.g., toothbrushing and flossing) and oral hygiene adherence. A systematic review of the effectiveness of interventions based on behavior models for promoting individuals’ oral health reported that the TTM is effective in changing behavior when combined with motivational interviewing.38 However, the authors drew this conclusion on the basis of one observational study, which provided little information on the nature of the intervention. Furthermore, the separate effects of the TTM and motivational interviewing could not be separated in this study.
Two systematic reviews of psychology-based interventions for increasing adherence to oral hygiene instructions in adults with periodontal diseases39,40 revealed that TTM studies were generally of low quality, so no firm conclusions could be made about the effectiveness of TTM in improving periodontal adult patient adherence to oral hygiene instructions.40 However, some support was found for self-efficacy alone in predicting oral health behaviors.39 In addition, the processes posited by the model, which has shown to be effective in promoting change, independent of the stages in the model.41
There is one RCT pilot study that assessed the usefulness of educational intervention based on TTM concerned toothbrushing.42 Based on self-report, 25.4% of participants reported improvements in their oral hygiene behaviors, including toothbrushing. While this shows some promise, it also means that the intervention did not influence three-quarters of the participants. The study had limitations, including the use of convenience sampling.42 Further, the number of participants in the follow-up sessions was low, indicating high rates of attrition.
For interdental cleaning, there is some research to support the use of TTM. A clinical trial that was conducted to identify the impact of an education program based on TTM and the use of interdental cleaning among senior schoolchildren concluded that the findings demonstrated that the model had a significant positive impact on improving the outcome of the educational program and increased the number of students at the maintenance stage compared with the control group.43 The authors also claimed that it decreased the perceived barriers and increased perceived benefits due to an increase in self-efficacy.43 However, the intervention was not based on any of the components of the TTM. The authors only measured two outcome measures based on elements of the model; thus, it may be that the intervention led to change in stage rather than the TTM effecting change. The intervention based on the model had a positive impact on improving understanding of interdental cleaning behavior.44 However, both studies had methodological weaknesses, including a lack of clear methods of randomization, which increases the chances of allocation bias.
For periodontal diseases, two systematic reviews were conducted to find out the effectiveness of interventions based on psychological models, including TTM, to improve the periodontal condition.39,40 There was no strong evidence reported in the reviews to support the effectiveness of interventions based on TTM to improve periodontal diseases.39,40
For free sugars intake, a recent systematic review of psychology-based interventions found no studies assessed the application of TTM at reducing free sugars intake related to dental caries among adults.22 There is a need for more clinical trials to examine the effectiveness of interventions based on TTM in reducing dietary free sugars intake among adults.22
In summary, while there is some evidence that TTM can be effectively applied to changing eating-related health behaviors and smoking cessation, its application to other health-related behaviors is limited. Notwithstanding the findings above, the TTM has been criticized extensively. For example, it has been postulated that the notion that individuals must progress through stages is unwarranted, as it is possible for individuals to progress immediately from wanting to change (stage 2: contemplation) to never engaging in the behavior again (stage 5: maintenance), without passing through intermediate stages.45 Secondly, the model has been critiqued for non-specificity; there is currently no evidence to assure researchers that the positive effects observed in some TTM studies are simply because an intervention is being given, rather than being specifically due to TTM-based interventions. Thirdly, most studies of the TTM are cross-sectional, demonstrating a relationship between behavior and stage, rather than the impact of an intervention.45 Fourthly, there are no systematic rules in TTM to assign individuals to stages.46 Finally, a compelling argument has been made as to why TTM should be ‘put to rest’, detailing a catalog of problems with its theoretical basis, implementation, outcomes, and philosophy, all of which are points within which the results of this review should be interpreted.47,48 Further clinical trials are needed to assess the effect of TTM-based interventions on reducing free sugars intake. Variables such as self-efficacy from the TTM could be useful targets for reducing free sugars intake.
Social Cognitive Theory (SCT)
SCT considers behavior to be the result of social influence and human cognitive processes.49 SCT is based on the principle of ‘triadic reciprocity’, which is illustrated in Figure 2. Triadic reciprocity suggests that three factors influence each other; behaviors, environments, and person. However, the contribution of the three dimensions to behavior change is not equal.
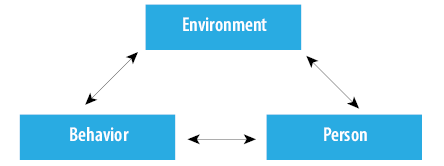
Figure 2: Triadic reciprocity of Social Cognitive Theory.50
SCT has been applied widely in the context of general health behaviors, including medication adherence, sexual behavior, physical activities, weight loss, and drug abuse behaviors.49,51 In a systematic review with meta-analysis, SCT was able to predict 31% of the variance in physical activity behaviors.52 The study also revealed that the ‘goals’ and ‘self-efficacy’ constructs were positively associated with physical activity, unlike other constructs, such as socio-structural factors and outcome expectations, which were negatively related.52 However, many of the included studies were cross-sectional and were unable to determine causal relationships that are important to assess the intervention based on the theory or their constructs.52
A further systematic review and meta-analysis was conducted to determine the effectiveness of physical activity and diet behavior change interventions based on the SCT among cancer survivors.53 The study identified that most of the included interventions were effective for enhancing diet behavior and physical activities, but this effectiveness was not related to specific SCT constructs. However, when taken in isolation, self-efficacy was shown to be positively associated with behavior change for diet and physical activities.53
In the last 10 years, only two RCTs have been conducted to examine the potential effectiveness of SCT for smoking cessation. The pooled results of these two RCTs support the use of SCT.54 However, both were conducted with college students, making the generalizability of these studies problematic, and one of the studies used a combined model of SCT and problem-behavior theory.
SCT has been applied in oral health-related behaviors, including adherence and oral hygiene practice. For tooth brushing, two simultaneous RCTs were conducted to test the effectiveness of oral health intervention based on two constructs; self-efficacy and action planning.55 Patients in the intervention group developed better skills, timing, and duration of toothbrushing, and decreased plaque formation and gingival bleeding compared with patients who received routine care.55 The study also revealed that outcome expectations were related to high self-efficacy and planning among patients.55 This focus on the individual constructs rather than the whole theory means that the full SCT is not assessed, leaving the role of SCT for toothbrushing mostly unexplored.
A trial of an education-based intervention found a positive relationship between dental flossing, self-efficacy, and motivation.56 However, several limitations make these findings less reliable, including having a problematic outcome measure (residual floss), poor generalizability (only university students), and a very short-term follow-up of one week. There was also no control group. Importantly, the intervention did not target constructs within the SCT, and another theory was used along with SCT.
Two systematic reviews have included evaluations of SCT for increasing adherence towards oral hygiene instructions in adults with periodontal diseases. Both reviews identified that self-efficacy, goal setting, and planning were effective interventions for improving oral health behavior in periodontal patients. However, the evidence was derived from a small number of low-quality trials.39,40 This suggests that at least some components of SCT may be effective for predicting oral health adherence.
No studies were found that assessed the effectiveness of applying the SCT to reducing free sugars intake related to dental caries among adults.22
In summary, most systematic reviews identified that the constructs self-efficacy, goal setting, and outcome expectations are promising for promoting individual health behaviors. Self-efficacy was the most often applied in the literature and consistently found positive results. Other constructs remain largely unsupported. This means that SCT may not be the most effective theory for predicting or changing health-related behaviors. However, it is also possible that this finding could be due to many interventions only applying a minimum number of constructs or used in isolation, rather than applying SCT as a whole.57 Further research is needed to address this gap in the literature and to examine the appropriateness of SCT for health-related behavior change.
Similarly, for free sugars intake, there is a need for more clinical trials to assess the effect of SCT-based interventions on free sugars intake, particularly since self-efficacy, goal setting, and outcome expectations constructs appear to be strongly related to free sugars intake among adults.
Theory of Planned Behavior (TPB)
The TPB suggests that behaviors are the result of an evaluation of the positives and negatives of any given action.45
The theory combines constructs to predict behaviors or intentions of individuals,58 including attitudes towards behaviors, subjective norms, and perceived behavioral control. Together, these contribute to the formation of behavioral intentions.45 According to TPB, these intentions are crucial for causing the behavior. The only way these can be bypassed is through perceived behavioral control, which can lead to a behavior without intention.45,58 Figure 3 illustrates this relationship.PB has been applied to many aspects of general health, and many recent systematic reviews have been conducted to assess the efficiency of the theory in predicting or changing behaviors. A systematic review to evaluate the effectiveness of TPB for predicting shared decision-making (SDM) behaviors of different health care professionals found that subjective norms were the most predictive variable of SDM behaviors followed by perceived behavioral control and attitude.59 Also, they found that intention was the most predictive construct of health professional’s performance towards SDM actions. Similar findings were reported in another systematic that concluded that subjective norms, attitude, and self-efficacy predicted the intentions of alcohol consumption.60
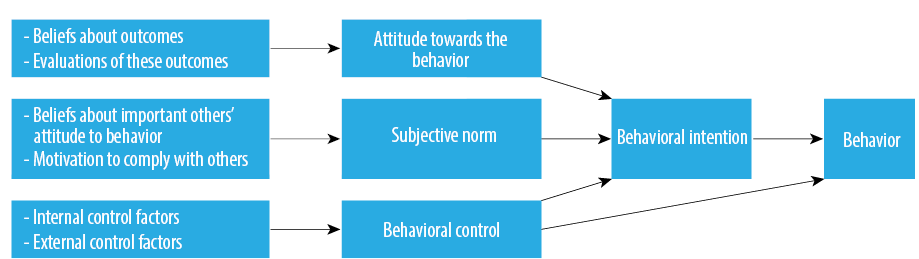
Figure 3: The Theory of Planned Behavior.45
There is strong evidence to support the use of TPB for smoking cessation programs; a meta-analysis study of 35 data sets from primary studies, and found that the construct ‘perceived behavior control’ is the most predictive of smoking cessation because it influences both intentions and behavior.61 The authors suggest that the culture of the country is also important as a mediating factor, with some cultures enhancing the effects of smoking cessation programs, mirroring findings from a separate study.62 This suggests that particularly ‘perceived behavior control’ may be relevant for understanding the effects of TPB for smoking cessation programs, and perhaps culture should be considered as an additional important factor.
In contrast, another systematic review found no strong evidence to support the effectiveness of interventions based on TPB for dietary behavior change in adolescents and young adults; this means that TPB might not be effective in bringing the desired change.63 A systematic review assessing the efficiency of questionnaires based on TPB for behavioral change found that there were errors in the estimation of sample size, namely, demographic data, measures, and the process of development of the questionnaires.64 This means that there were methodological issues in the evaluation of many TPB interventions.
For oral health, TPB has been widely applied to predict behavior related to oral health including toothbrushing, dental flossing, and dental attendance.65–70 When broadly used, the theory could successfully predict a significant portion of the variance in oral health-related behaviors.67,68,70 For example, one study found that they could successfully predict 57% of the variation in oral hygiene habits and 66% of the variance in dental attendance.67 Another study provided more cautious support of TPB, suggesting that cultural differences may exist regarding the most appropriate application of the theory.62 The authors conducted a study to identify predictors of oral hygiene and found that in the Caribbean, the best predictors were attitude and social norms, while in Nepal, perceived behavioral control and expected social outcomes were most predictive.62 The majority of these studies have adopted cross-sectional designs to assess the predictive power of TPB variables on oral health-related behaviors.65–70 These studies support the ability of TPB variables to predict intentions and behavior of oral health, saying that these studies do not assess the effectiveness of an intervention based on TPB in changing behavior.
Only one RCT had incorporated TPB constructs in intervention to improve the periodontal condition of adults.39 However, based on the review, the constructs were used as a basis for predicting behavior change rather than the basis of the intervention. Their findings supported those of a clinical RCT assessing the effectiveness of TPB in changing behavior.71 The authors applied a full-factorial experimental design to determine the effects of three interventions based on the three main TPB constructs to improve physical activity. The choice of physical activity was based on the strong correlation of TPB to predict the behavior. They found that the interventions changed the intention related to the behavior.71 However, the interventions failed to achieve behavior change. This study suggests that TPB has a limited influence on behavior.
For free sugars intake, no studies were found that assessed the effectiveness of applying the TPB to reducing free sugars intake related to dental caries among adults.22
There is some support for the use of TPB for changing some health-related behaviors. But, there is a need for more RCTs to assess the effectiveness of interventions based on TPB that aim to improve oral health-related behaviors.22 It appears that self-efficacy/perceived control is the most important component of the TPB for predicting behavior.39 A major limitation of the theory is that it considers individuals as rational decision-makers;45 however, this is not always the case. For example, patients with dental anxiety may not attend dental clinics on a regular basis.72 In this case, the behavior of not attending regularly is based on emotion (fear) rather than rational decision-making. Finally, the findings of this review need to be considered against recent work in the field suggesting that TPB is not a helpful model in the design of behavior change interventions.71 It has been argued that the TPB is insufficient as a tool for behavior change, but can predict behavior only, which does not serve the purpose of behavioral change science.73 For free sugars intake, the TPB could be useful in predicting free sugars intake, in particular, perceived behavior control seems likely to be a strong predictor.
Information-Motivation-Behavioral Skills Model (IMB)
The IMB model suggests that individuals perform a behavior only if they expect a net benefit from it.74 According to the model, three constructs contribute to behavior change, which are information, motivation, and behavioral skills. Figure 4 illustrates the relationship between the constructs.75
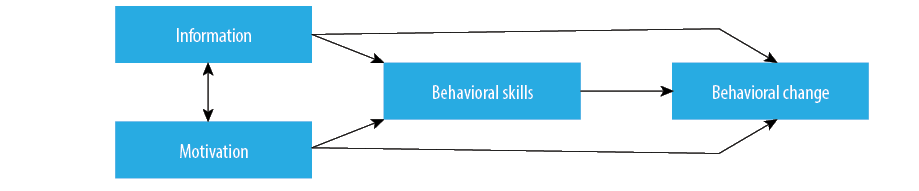
Figure 4: The Information-Motivation-Behavioral Skills Model.75
The IMB model has been applied to a wide variety of health-related behaviors. The IMB model was initially applied to minimize HIV risk behaviors.76–78 For instance, interventions based on the IMB model were used to promote women to use female condoms during intercourse with their partners,78 and the model has shown to be effective in reducing the HIV risk behavior between individuals.76
Within the last five years, three studies from different health domains have tested the effectiveness of the IMB model for changing behavior.79–81 The shared findings indicate that there is no strong evidence to support or reject the effectiveness of interventions based on the IMB model for sustaining new short-term health behavior change. However, their findings are further called into question after a systematic review found that the IMB model achieved healthy behavior change that was sustained for 12 months.82 Because of this, it seems there is some evidence to support the use of the model for health-related behavior change for up to one year, but there is a need for more high-quality studies to assess its effectiveness beyond a one-year follow-up.
The IMB model has been applied in two studies related to oral health; to gather information and change the behavior of oral healthcare providers83 and to examine the practicality of oral health education.84 Despite the promising findings from the studies,83,84 caution should be expressed for several reasons. First, the studies were both based on specific populations – prenatal care providers and HIV patients – and both were non-experimental studies, which means there was no causal assessment of the intervention in improving oral health behavior.73,74 Additionally, in one study, the model constructs were not directly assessed.84 There has been no effective research on the potential usefulness of the model for toothbrushing, interdental cleaning, oral health adherence, and diet control including free sugars intake related to dental caries in adults.22
There are some promising applications of the IMB model to changing general health behavior for up to one year if researchers follow the three phases of the model application when designing interventions. Because of this, there is some possibility that this model could also be useful for oral health-related behavior change in the short term. However, due to a lack of research related to oral health applications, this application remains uncertain. Further, there are some significant limitations to the model. First, the model assumes that individuals are rational decision-makers,85 but this is not always the case as individuals can engage in actions based on emotions.58 A criticism of the IMB model is its lack of specificity regarding the components of the three core constructs. Whereas other models specify the nature of the information and motivation elements, the IMB model is not as specific. Thus, any effects maybe because the constructs identified in the IMB process are similar to those in other models, which means that the change was from the intervention instead of the model. Finally, the model does not take into account the context of behavior change, such as environmental and social factors. Therefore, the usefulness of this model in reducing free sugars intakes among adults may be limited.
PRIME Theory of Motivation
The PRIME Theory of motivation is a very complex framework, which considers the brain as the energizer and director of an individual’s behavior.75 It is based on the principle, “At every moment we act in pursuit of what we most desire (want or need) at that moment”.75 The theory was developed as a patchwork of elements from previous theories, focusing on elements that help explain and predict behavior.86,87 Although not a behavior change theory in itself, given the central role that motivation plays in undertaking behavior change, the PRIME Theory of motivation is reviewed here.86,87 As shown in Figure 5, there are five subsystems within PRIME, including plans, responses, impulses and inhibitors, motives, and evaluations.75
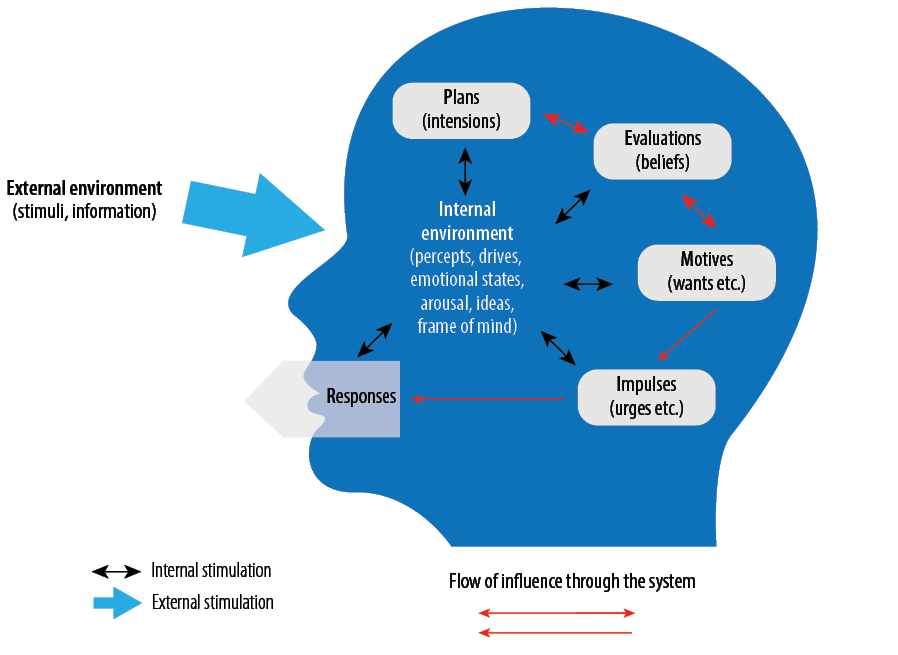
Figure 5: Five levels of subsystems of PRIME Theory of Human Motivation.88
PRIME Theory has been mainly applied to one behavior, namely, tobacco use. It was been applied initially to smoking cessation interventions in conjunction with behavioral change techniques.89,90
A RCT examining the effectiveness of a PRIME-based smoking cessation interactive webpage compared to a passive information providing webpage found that 10% quit smoking for six months in both groups, which is similar to the success rate of one-to-one counseling.91
An observational cohort study investigated the usefulness of a smartphone app based on PRIME Theory and behavior change techniques (BCT) to quit smoking (even though it was not clear exactly how this app was created).92 Approximately 19% of the participants quit smoking for 28 days, so the authors concluded that the app could help certain smokers to stop. Both studies show that PRIME may be effective, but they only have short-term follow-ups and were applied to online or via apps settings, which can miss populations who are not using apps or online smoking cessation programs.
PRIME Theory has not been applied to specific oral health behaviors including reducing free sugars intake related to dental caries among adults,22 although some have suggested that it may be appropriate to apply to do so.73
In summary, the PRIME Theory of motivation has not been applied to specific oral health behaviors and has not been applied to most other health-related behaviors. Because of this lack of evidence-base, more studies are needed before recommendations regarding its application to adult oral health behaviors can be made. Additionally, the theory can be used in conjunction with the capability, opportunity, motivation, and behavior (COM-B) model.75
Behavior Change Wheel (BCW) framework
The BCW framework considers the importance of the contexts in which actions or behaviors take place.75 Also, the framework draws a systematic and coherence plan on how to achieve behavior change, from understanding the context of the behavior to offering many function interventions and categories and techniques to achieve the behavior change.75,93
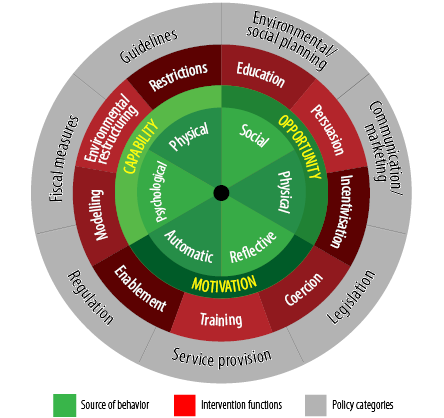
Figure 6: The Behavior Change Wheel.83
The BCW comprises three layers, as demonstrated in Figure 6 and explained below:93
- It starts with the inner layer, which is the hub of the wheel, and it is used to identify the most proximal determinants of behavior at the individual or population levels. The COM-B model is used for this purpose, and the theoretical domain framework (TDF) can be used for further analysis along with the COM-B to model the behavior.
- The second layer is the intervention functions, which contains a range of functions, which are effective in achieving behavior change. The application of these functions depends on COM-B model analysis of the behavior.
- The outer layer (the rim of the wheel) contains policy categories, which support the delivery of the intervention functions and modify the context in which individual behavior occurs.
Four initial tools are applied within the BCW framework when designing effective interventions: COM-B model, TDF, BCT, and mode of delivery ontology (MoDO).89,94 These tools all work together, under the BCW framework, where COM-B model is for understanding behavior, TDF is further analysis of behaviors, BCTs are used to change behaviors, and MoDO is used to deliver the BCT. The relationship between the four tools with BCW is shown in Figure 7. The BCW framework suggests eight steps (grouped into three stages) for designing effective interventions for behavior change.95
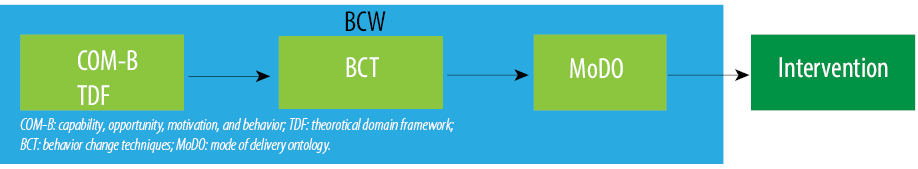
Figure 7: The four tools with Behavior Change Wheel (BCW) and their relation with BCW.
The BCW has been used for different purposes. For example, it provides a system for coding behavioral interventions and has been utilized within systematic reviews to categorize interventions used to change behavior and as a system for designing interventions. To date, the BCW has been used as part of systematic reviews in the following fields: head and neck cancer,96 research design,97 and adherence to medicine related to cardiovascular disease.98 The BCW framework was also used to develop behavior change interventions for weight management-healthy,99,100 rehabilitation,101 capacity building,102 smoking cessation,103 and men’s sexual health.104 In general, most authors found that the BCW was a useful theory for designing interventions.100,102,103
However, one of the challenges in using the BCW framework was difficulty in achieving a consensus among scientists about the importance of a dimension in behavior change after data gathering.104 Also, it has been suggested that the BCW framework is not designed for transforming behavior change plans into software application features, so in one study, the authors had to rely on other sources for selecting appropriate interventions.105 The BCW framework has been described as “less directive and helpful” because the authors believe that and policy categories of the BCW framework are not as well defined as their names suggested in the framework irrespective of the behavior analysis stage.101 For example, the outer layer of the system (policy categories) is not well defined and fit more under the policy level. This led them to fit all of their intervention components under one-category: service provision. However, they felt that the BCT Taxonomy (v1) was useful in the development of behavior change interventions because it provided them with common terminology, which helped in describing the aim of each component of the interventions. Unfortunately, none of these studies was a RCT. Currently, few clinical trial protocols have been published that aim to test the effectiveness of interventions based on the BCW framework in different health-related behaviors, these include physical activity106,107 and men’s sexual health.108
The BCW framework, with its tools and stages, has not been tested in specific oral health behaviors among the adult population, including reducing free sugars intake.22 For example, TDF was used to understand factors that influence the application of fluoride varnish on Scottish children’s teeth.105 Another example is the use of TDF in understanding the factors that influence the management of patient’s with bacterial infections in dental settings.109 The BCW framework and its tools may provide a useful theory for the design of interventions to enhance oral health.73
In summary, the BCW system, along with its associated tools, appears to be the most suitable for capturing the complexity of adult oral health-related behaviors, in particular reducing free sugars intake among adults. The previous applications to general settings have demonstrated that it can be successfully applied to design interventions and to analyze and understand behaviors. Furthermore, it explicitly links behavior analysis with behavior interventions.110 Its usefulness with regard to oral health remains to be explored. The BCW would be a very useful framework for free sugars intake because it offers the opportunity to systematically analyze the context in which the consumption of free sugars takes place.
Conclusion
There is good evidence to suggest that interventions based on theory are more effective than interventions developed without a theory-based approach. Oral health education does not influence diet control behavior in the long term; it mainly increases knowledge with possible behavior change in the short-term. Of the six theories of behavior change and a framework reviewed here, there is limited evidence from intervention studies based on social cognition models, including TTM and TPB. However, these models can predict free sugars intake, in particular individual constructs, including self-efficacy, goal setting, and action planning. The BCW and its tools offer hope for the development of effective behavior change interventions to reduce free sugars intake among adults because of the comprehensiveness they provide. However, their use in oral health is limited at the moment. More studies, including trials, are suggested to apply BCW and its tools when developing interventions for reducing free sugars intake.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Maru AM, Narendran S. Epidemiology of dental caries among adults in a rural area in India. J Contemp Dent Pract 2012 May;13(3):382-388.
- 2. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012 Dec;380(9859):2163-2196.
- 3. NIDCR. Dental caries (tooth decay) in adults (Age 20 to 64). National Institute of Dental and Craniofacial Research. [cited 2015 April 11]. Available from: http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/DentalCaries/DentalCariesAdults20to64.htm.
- 4. Moynihan PJ, Kelly SA. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res 2014 Jan;93(1):8-18.
- 5. Public Health of England. Delivering better oral health: an evidence-based toolkit for prevention. London: The Public Health of England; 2014.
- 6. Bernabé E, Sheiham A. Age, period and cohort trends in caries of permanent teeth in four developed countries. Am J Public Health 2014 Jul;104(7):e115-e121.
- 7. Bernabé E, Sheiham A. Extent of differences in dental caries in permanent teeth between childhood and adulthood in 26 countries. Int Dent J 2014b Oct;64(5):241-245.
- 8. Sheiham A, James WP. A reappraisal of the quantitative relationship between sugar intake and dental caries: the need for new criteria for developing goals for sugar intake. BMC Public Health 2014 Sep;14(14):863.
- 9. Sheiham A, James WP. Diet and dental caries: the pivotal role of free sugars reemphasized. J Dent Res 2015 Oct;94(10):1341-1347.
- 10. Slade GD, Sanders AE, Do L, Roberts-Thomson K, Spencer AJ. Effects of fluoridated drinking water on dental caries in Australian adults. J Dent Res 2013 Apr;92(4):376-382.
- 11. White D, Pitts N, Steele J, Sadler K, Chadwick B. Disease and related disorders – a report from the adult dental health survey 2009. In: O’ Sullivan I, editor. Adult Dental Health Survey 2009. London: The Health and Social Care Information Centre; 2011.
- 12. European Food Safety Authority. Scientific opinion on dietary reference values for carbohydrates and dietary fibre. EFSA Panel on Dietetic Products, Nutrition and Allergies. EFSA J 2010;8:1462.
- 13. SACN. (2015) Carbohydrates and Health. Norwich: TSO (The Stationery Office) Online. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf.
- 14. Moynihan P. Sugars and dental caries: evidence for setting a recommended threshold for intake. Adv Nutr 2016 Jan;7(1):149-156.
- 15. Ramseier CA, Suvan JE. Behaviour change counselling for tobacco use cessation and promotion of healthy lifestyles: a systematic review. J Clin Periodontol 2015 Apr;42(Suppl 16):S47-S58.
- 16. Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev 2015;9(3):323-344.
- 17. Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: how useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health 2007 Jun;7(104):104.
- 18. Ogden J. Health Psychology: a textbook. 3rd edition. Berkshire: Open University Press; 2004.
- 19. Forshaw M. Essential of Health Psychology. London: Hodder Education; 2002.
- 20. Abraham C, Kelly MP, West R, Michie S. The UK National Institute for Health and Clinical Excellence public health guidance on behaviour change: a brief introduction. Psychol Health Med 2009 Jan;14(1):1-8.
- 21. Michie S, West R. Behaviour change theory and evidence: a presentation to government. Health Psychol Rev 2013;7(1):1-22.
- 22. Al Rawahi SH, Asimakopoulou K, Newton JT. Theory based interventions for caries related sugar intake in adults: systematic review. BMC Psychol 2017 Jul;5(1):25.
- 23. Daly B, Batchelor P, Treasure ET, Watt RG. Essential dental public health. 2nd ed. Oxford: Oxford University Press; 2013.
- 24. Kay EJ, Locker D. Is dental health education effective? A systematic review of current evidence. Community Dent Oral Epidemiol 1996 Aug;24(4):231-235.
- 25. Habbu SG, Krishnappa P. Effectiveness of oral health education in children - a systematic review of current evidence (2005-2011). Int Dent J 2015 Apr;65(2):57-64.
- 26. Kay E, Vascott D, Hocking A, Nield H, Dorr C, Barrett H. A review of approaches for dental practice teams for promoting oral health. Community Dent Oral Epidemiol 2016 Aug;44(4):313-330.
- 27. Gupta A, Smithers LG, Harford J, Merlin T, Braunack-Mayer A. Determinants of knowledge and attitudes about sugar and the association of knowledge and attitudes with sugar intake among adults: A systematic review. Appetite 2018 Jul;126(126):185-194.
- 28. Werner H, Hakeberg M, Dahlström L, Eriksson M, Sjögren P, Strandell A, et al. Psychological interventions for poor oral health: a systematic review. J Dent Res 2016 May;95(5):506-514.
- 29. Rutter D, Quine L. Changing Health Behaviour. Buckingham: intervention and research with social cognition models. Open Press University; 2002.
- 30. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol 1992 Sep;47(9):1102-1114.
- 31. Di Noia J, Prochaska JO. Dietary stages of change and decisional balance: a meta-analytic review. Am J Health Behav 2010 Sep-Oct;34(5):618-632.
- 32. Hoetzel K, von Brachel R, Schlossmacher L, Vocks S. Assessing motivation to change in eating disorders: a systematic review. J Eat Disord 2013 Oct;1(1):38.
- 33. Spahn JM, Reeves RS, Keim KS, Laquatra I, Kellogg M, Jortberg B, et al. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J Am Diet Assoc 2010 Jun;110(6):879-891.
- 34. Cahill K, Lancaster T, Green N. Stage-based interventions for smoking cessation. Cochrane Database Syst Rev 2010 Nov;(11):CD004492.
- 35. Stanton A, Grimshaw G. Tobacco cessation interventions for young people. Cochrane Database Syst Rev 2013 Aug;(8):CD003289.
- 36. Bully P, Sánchez Á, Zabaleta-del-Olmo E, Pombo H, Grandes G. Evidence from interventions based on theoretical models for lifestyle modification (physical activity, diet, alcohol and tobacco use) in primary care settings: A systematic review. Prev Med 2015 Jul;76(Suppl):S76-S93.
- 37. Mastellos N, Gunn LH, Felix LM, Car J, Majeed A. Transtheoretical model stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst Rev 2014 Feb;(2):CD008066.
- 38. Yevlahova D, Satur J. Models for individual oral health promotion and their effectiveness: a systematic review. Aust Dent J 2009 Sep;54(3):190-197.
- 39. Newton JT, Asimakopoulou K. Managing oral hygiene as a risk factor for periodontal disease: a systematic review of psychological approaches to behaviour change for improved plaque control in periodontal management. J Clin Periodontol 2015 Apr;42(Suppl 16):S36-S46.
- 40. Renz A, Ide M, Newton T, Robinson PG, Smith D. Psychological interventions to improve adherence to oral hygiene instructions in adults with periodontal diseases. Cochrane Database Syst Rev 2007 Apr;(2):CD005097.
- 41. Renz AN, Newton JT. Changing the behavior of patients with periodontitis. Periodontol 2000 2009;51(1):252-268.
- 42. Wu A, Switzer-Nadasdi R. The role of health behavior in preventing dental caries in resource-poor adults: a pilot intervention. J Tenn Dent Assoc 2014;94(2):17-21, quiz 22-23.
- 43. Hashemian M, Fallahi A, Tavakoli G, Zarezadeh Y, Babaki BN, Rahaei Z. Impact of education on interdental cleaning behaviour based on the transtheoretical model. Oral Health Prev Dent 2012;10(1):37-46.
- 44. Tavakoli G, Falahi A. The effect of educating mothers in inter-dental cleaning behavior on their children’s dental health behavior: testing the transtheoretical model. Health Educ Health Prom 2013;1(2):5-19.
- 45. Ogden J. Health psychology: a textbook 5th Revised edition. England: Open University Press; 2012.
- 46. Sutton S. Interpreting cross-sectional data on stages of change. Psychol Health 2000;15(2):163-171.
- 47. West R. Time for a change: putting the Transtheoretical (Stages of Change) Model to rest. Addiction 2005 Aug;100(8):1036-1039.
- 48. West R. The transtheoretical model of behaviour change and the scientific method. Addiction 2006;101(6):774-77 .
- 49. Sharma M, Romas J. Theoretical foundation of health education and health promotion. London: Jones and Bartlett Learning; 2016.
- 50. Crosby RA, Salazar LF, DiClemente RJ. Social cognitive theory applied to behaviour change. In: DiClemente RJ, Salazar LF, Crosby RA, editors. Health behavior theory for public health: principles, foundations, and applications. Burlington: Jones and Bartlett Learning; 2013. p. 163-186. Available from: https://www.amazon.co.uk/Health-Behavior-Theory-Public-ebook/dp/B07CJWMY8K/ref=sr_1_1?keywords=Health+behavior+theory+for+public+health%3A+principles%2C+foundations%2C+and+applications&qid=1584279886&sr=8-1&swrs=1EBF80E8A4EDAC94D8973C95C4F27CEE.
- 51. Luszczynska A, Schwarzer P. Social cognitive theory. In: Conner M, and Norman P, editors. Predicting health behaviour. Berkshire: Open Press University; 2005. p. 127-169. Available from: https://www.amazon.co.uk/Predicting-Health-Behaviour-Conner-Mark/dp/0335211763/ref=sr_1_1?keywords=Predicting+health+behaviour.&qid=1584280040&sr=8-1.
- 52. Young MD, Plotnikoff RC, Collins CE, Callister R, Morgan PJ. Social cognitive theory and physical activity: a systematic review and meta-analysis. Obes Rev 2014 Dec;15(12):983-995.
- 53. Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv 2015 Jun;9(2):305-338.
- 54. Villanti AC, McKay HS, Abrams DB, Holtgrave DR, Bowie JV. Smoking-cessation interventions for U.S. young adults: a systematic review. Am J Prev Med 2010 Dec;39(6):564-574.
- 55. Clarkson JE, Young L, Ramsay CR, Bonner BC, Bonetti D. How to influence patient oral hygiene behavior effectively. J Dent Res 2009 Oct;88(10):933-937.
- 56. Staunton L, Gellert P, Knittle K, Sniehotta FF. Perceived control and intrinsic vs. extrinsic motivation for oral self-care: a full factorial experimental test of theory-based persuasive messages. Ann Behav Med 2015 Apr;49(2):258-268.
- 57. Abraham C, Conner M, Jones F, O’Connor D. Health psychology topics in applied psychology. London: Hodder Education; 2008.
- 58. Morrison V, Bennett P. An introduction to health psychology. Essex: Pearson Education Limited; 2009.
- 59. Thompson-Leduc P, Clayman ML, Turcotte S, Légaré F. Shared decision-making behaviours in health professionals: a systematic review of studies based on the Theory of Planned Behaviour. Health Expect 2015 Oct;18(5):754-774.
- 60. Cooke R, Dahdah M, Norman P, French DP. How well does the theory of planned behaviour predict alcohol consumption? A systematic review and meta-analysis. Health Psychol Rev 2016 Jun;10(2):148-167.
- 61. Topa G, Moriano JA. Theory of planned behavior and smoking: meta-analysis and SEM model. Subst Abuse Rehabil 2010 Dec;1:23-33.
- 62. Buunk-Werkhoven YA, Dijkstra A, Bink P, van Zanten S, van der Schans CP. Determinants and promotion of oral hygiene behaviour in the Caribbean and Nepal. Int Dent J 2011 Oct;61(5):267-273.
- 63. Hackman CL, Knowlden AP. Theory of reasoned action and theory of planned behavior-based dietary interventions in adolescents and young adults: a systematic review. Adolesc Health Med Ther 2014 Jun;5:101-114.
- 64. Oluka OC, Nie S, Sun Y. Quality assessment of TPB-based questionnaires: a systematic review. PLoS One 2014 Apr;9(4):e94419.
- 65. Lavin D, Groarke A. Dental floss behaviour: a test of the predictive utility of the theory of planned behaviour and the effects of making implementation intentions. Psychol Health Med 2005;10(3):243-252.
- 66. Luzzi L, Spencer AJ. Factors influencing the use of public dental services: an application of the Theory of Planned Behaviour. BMC Health Serv Res 2008 Apr;8(1):93.
- 67. Defranc A, Van den Broucke S, Leroy R, Hoppenbrouwers K, Lesaffre E, Martens L, et al. Measuring oral health behaviour in Flemish health care workers: an application of the theory of planned behaviour. Community Dent Health 2008 Jun;25(2):107-114.
- 68. Van den Branden S, Van den Broucke S, Leroy R, Declerck D, Hoppenbrouwers K. Measuring determinants of oral health behaviour in parents of preschool children. Community Dent Health 2013 Mar;30(1):19-25.
- 69. Anderson CN, Noar SM, Rogers BD. The persuasive power of oral health promotion messages: a theory of planned behavior approach to dental checkups among young adults. Health Commun 2013;28(3):304-313.
- 70. Dumitrescu AL, Dogaru BC, Duta C, Manolescu BN. Testing five social-cognitive models to explain predictors of personal oral health behaviours and intention to improve them. Oral Health Prev Dent 2014;12(4):345-355.
- 71. Sniehotta F. An experimental test of the theory of planned behavior. Appl Psychol Health Well-Being 2009;1(2):257-270.
- 72. Milgrom P, Newton JT, Boyle C, Heaton LJ, Donaldson N. The effects of dental anxiety and irregular attendance on referral for dental treatment under sedation within the National Health Service in London. Community Dent Oral Epidemiol 2010 Oct;38(5):453-459.
- 73. Asimakopoulou K, Newton JT. The contributions of behaviour change science towards dental public health practice: a new paradigm. Community Dent Oral Epidemiol 2015 Feb;43(1):2-8.
- 74. Crosby RA, Salazar LF, DiClemente RJ. Value-expectancy theories. In: DiClemente RJ, Salazar LF, Crosby RA, editors. Health behavior theory for public health: principles, foundations, and applications. Burlington: Jones and Bartlett Learning; 2013. p. 65-82.
- 75. Michie S, West R, Campbell R, Brown J, Gainforth H. ABC of behaviour change theories: an essential resource for researchers, policy makers and practitioners. London: Silverback Publishing; 2014.
- 76. Fisher JD, Fisher WA, Shuper PA. The information-motivation-behavioural skills model of HIV preventive behavior. In: Diclement RJ, Crosby RA, Kegler MC, editors. Emerging Theories in Health Promotion Practice and Research. San Francisco: Jossey-Bass; 2009.
- 77. Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull 1992 May;111(3):455-474.
- 78. Mimiaga MJ, Reisner SL, Reilly L. Individual interventions. In: Mayer KH, Pizer HF, editors. HIV prevention comprehensive approach. London: Elsevier; 2009.
- 79. Ndebele M, Kasese-Hara M, Greyling M. Application of the information, motivation and behavioural skills model for targeting HIV risk behaviour amongst adolescent learners in South Africa. SAHARA J 2012 Dec;9(Suppl 1):S37-S47.
- 80. Kudo Y. Effectiveness of a condom use educational program developed on the basis of the Information-Motivation-Behavioral Skills model. Jpn J Nurs Sci 2013 Jun;10(1):24-40.
- 81. Peltzer K, Naidoo P, Louw J, Matseke G, Zuma K, McHunu G, et al. Screening and brief interventions for hazardous and harmful alcohol use among patients with active tuberculosis attending primary public care clinics in South Africa: results from a cluster randomized controlled trial. BMC Public Health 2013 Jul;13:699.
- 82. Chang SJ, Choi S, Kim SA, Song M. Intervention strategies based on information-motivation-behavioral skills model for health behavior change: a systematic review. Asian Nurs Res 2014 Sep;8(3):172-181.
- 83. Vamos CA, Walsh ML, Thompson E, Daley EM, Detman L, DeBate R. Oral-systemic health during pregnancy: exploring prenatal and oral health providers’ information, motivation and behavioral skills. Matern Child Health J 2015 Jun;19(6):1263-1275.
- 84. Vernon LT, Demko CA, Webel AR, Mizumoto RM. The feasibility, acceptance, and key features of a prevention-focused oral health education program for HIV+ adults. AIDS Care 2014;26(6):763-768.
- 85. Simons-Morton B, McLeroy K, Wendel M. Behavior theory in health promotion practice and research. Jones & Bartlett Publishers; 2011 Sep 16. London: Jones and Bartlett Learning; 2012.
- 86. West R. Theory of addiction. Oxford: Wiley-Blackwell; 2006.
- 87. West R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 2009 Aug;6(4):277-283.
- 88. McEwen A, West R. The PRIME approach to giving up smoking. Pract Nurs 2010;21(3):145-153.
- 89. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011 Apr;6(1):42.
- 90. Michie S, Brown J, Geraghty AW, Miller S, Yardley L, Gardner B, et al. Development of StopAdvisor: A theory-based interactive internet-based smoking cessation intervention. Transl Behav Med 2012 Sep;2(3):263-275.
- 91. Brown J, Michie S, Geraghty AW, Yardley L, Gardner B, Shahab L, et al. Internet-based intervention for smoking cessation (StopAdvisor) in people with low and high socioeconomic status: a randomised controlled trial. Lancet Respir Med 2014 Dec;2(12):997-1006.
- 92. Ubhi HK, Michie S, Kotz D, Wong WC, West R. A mobile app to aid smoking cessation: preliminary evaluation of SmokeFree28. J Med Internet Res 2015 Jan;17(1):e17.
- 93. Michie S, Atkins L, West S. The behaviour change wheel: a guide to designing interventions. London: Silverback Publishing; 2014.
- 94. Carey J, Hastings W, Michie. Mode of delivery ontology (unpublished).
- 95. Atkins L, Michie S. Conference on ‘Changing dietary behaviour: physiology through to practice’ Symposium 4: Changing diet and behaviour – putting theory into practice Designing interventions to change eating behaviours, Proc Nutr Soc 2015;74:164-170. Available from: https://www.cambridge.org/core/services/aop-cambridge core/content/view/0FB561F47C354DBAA80B01F5ADDA6546/S0029665115000075a.pdf/designing_interventions_to_change_eating_behaviours.pdf.
- 96. Govender R, Smith CH, Taylor SA, Grey D, Wardle J, Gardner B. Identification of behaviour change components in swallowing interventions for head and neck cancer patients: protocol for a systematic review. Syst Rev 2015 Jun;4(89):89.
- 97. Beard E, Lewis JJ, Copas A, Davey C, Osrin D, Baio G, et al. Stepped wedge randomised controlled trials: systematic review of studies published between 2010 and 2014. Trials 2015 Aug;16(353):353.
- 98. Laba TL, Bleasel J, Brien JA, Cass A, Howard K, Peiris D, et al. Strategies to improve adherence to medications for cardiovascular diseases in socioeconomically disadvantaged populations: a systematic review. Int J Cardiol 2013 Sep;167(6):2430-2440.
- 99. Curtis KE, Lahiri S, Brown KE. Targeting parents for childhood weight management: development of a theory-driven and user-centered healthy eating app. JMIR Mhealth Uhealth 2015 Jun;3(2):e69.
- 100. Robinson E, Higgs S, Daley AJ, Jolly K, Lycett D, Lewis A, et al. Development and feasibility testing of a smart phone based attentive eating intervention. BMC Public Health 2013 Jul;13(13):639.
- 101. Connell LA, McMahon NE, Redfern J, Watkins CL, Eng JJ. Development of a behaviour change intervention to increase upper limb exercise in stroke rehabilitation. Implement Sci 2015 Mar;10(34):34.
- 102. Murphy AL, Gardner DM, Kutcher SP, Martin-Misener R. A theory-informed approach to mental health care capacity building for pharmacists. Int J Ment Health Syst 2014 Nov;8(1):46.
- 103. Gould GS. Exploring the barriers and enablers to smoking cessation in pregnant aboriginal and Torres Strait islander women with the behaviour change wheel. Australas Epidemiol 2014 Oct;21(2):31-35.
- 104. Webster B. Development of a theory-based interactive digital intervention to improve condom use in men in sexual health clinics: an application of qualitative methods using the behaviour change wheel. Lancet 2013;382:S102.
- 105. Gnich W, Bonetti D, Sherriff A, Sharma S, Conway DI, Macpherson LM. Use of the theoretical domains framework to further understanding of what influences application of fluoride varnish to children’s teeth: a national survey of general dental practitioners in Scotland. Community Dent Oral Epidemiol 2015 Jun;43(3):272-281.
- 106. Busse M, Quinn L, Dawes H, Jones C, Kelson M, Poile V, et al. Supporting physical activity engagement in people with Huntington’s disease (ENGAGE-HD): study protocol for a randomized controlled feasibility trial. Trials 2014 Dec;15(1):487.
- 107. Martin R, Murtagh EM. An intervention to improve the physical activity levels of children: design and rationale of the ‘Active Classrooms’ cluster randomised controlled trial. Contemp Clin Trials 2015 Mar;41:180-191.
- 108. Bailey JV, Webster R, Hunter R, Freemantle N, Rait G, Michie S, et al. The Men’s Safer Sex (MenSS) trial: protocol for a pilot randomised controlled trial of an interactive digital intervention to increase condom use in men. BMJ Open 2015 Feb;5(2):e007552.
- 109. Newlands R, Duncan EM, Prior M, Elouafkaoui P, Elders A, Young L, et al; Translation Research in a Dental Setting (TRiaDS) Research Methodology Group. Barriers and facilitators of evidence-based management of patients with bacterial infections among general dental practitioners: a theory-informed interview study. Implement Sci 2016 Jan;11(1):11.
- 110. Atkins L, Wood C, Michie S. How to design and describe behaviour change interventions. Health Psychol Update 2015;24:36-42.