|
INTRODUCTION
Urinary tract infection (UTI) is the second most common clinical indication for empirical antibiotic treatment in primary and secondary health care settings, and urine samples constitute the largest single category of specimens examined in most medical microbiological laboratories.1 34% of self-reported adults had at least one occurrence of UTI in the United States within the period of 1988 and 1994.2 Diabetes mellitus is a complex metabolic syndrome caused by lack of insulin resulting in inappropriate high blood glucose levels.3 The incidence of diabetes mellitus (DM) throughout the world is increasing strikingly and is becoming a serious public health problem especially in the developing countries.4 Diabetes mellitus is associated with many complications and in the long run it has some major effects on the genitourinary system which makes diabetic patients more liable to UTI and particularly to upper urinary tract infections.5 It has a long term effect on the incidence of UTI and it has been reported to be around four times higher in diabetics compared to non-diabetic patients.6 Although the exact reasons for this trend remains unclear, a few studies have shown that the reason could be the presence of static pools of urine due to dysfunctional bladders contracting poorly, which serves a favorable media for bacterial growth while others suggest that hyperglycemic urine promotes rapid bacterial growth and colonization.7,8 A series of studies from 1959-2005 have also provided evidence that UTI is distinctly more common among female diabetics compared to healthy females.9
The most common organisms causing UTI are E. coli while Proteus, Klebsiella, Streptococcus and Staphylococcus epidermis also commonly the causative agents.9 Both in community and hospital settings, antimicrobial resistance among uropathogens causing urinary tract infections is also increasing.10 E. coli is the most frequently found bacteria in UTI patients from both these settings which accounts for 80-90% of UTI cases.11-13
A study of the susceptibility of the host and the prevalence of the different strains of UTI pathogens are of primary importance in the development of infections. Therefore, the aim of this study is to determine the prevalence of different kinds of uropathogens in diabetic patients and the resistance pattern of antibiotics in various pathogens.
METHODS
This was a retrospective study where the retrospective urine culture assay data from 85 patients who suffered from both UTI and diabetes were randomly studied. Data was collected from log and register book of Popular Diagnostic Center and Medinova Diagnostic center in Dhaka for a six months period between August 2009 and January 2010. The data was analyzed statistically using Microsoft® Excel 2002 (10.6854.6845) SP3 software.
The age of all patients included in this survey was above 18. Subjects were included only when they were clinically diagnosed to be diabetic patients and had a blood sugar level greater than 7.8 mmol/l and exhibited glycosouria. All of the subjects were clinically diagnosed as UTI patients with a corresponding uro-culture showing a bacterial count of more than 105 cfu/ml.
RESULTS
The distribution of the infections according to the age and sex of the diabetic patients is summarized in Table 1. Out of the 85 patients randomly reviewed within the 6 months period, 25.9% (22 patients) were males and 74.1% (63 patients) were females. Overall, all the females were aged between 26-83 years while the males were aged between 43-70 years. Among the population infected with E. coli, the number of male patients was 18 while that of females was 49 with the age range of 43-70 years and 26-83 years respectively. In case of Streptococcus sp. the number of females infected was 7 with just a single male patient in the group and age ranged between 30-70 and 60 years respectively. The occurrences of other pathogenic infections were higher among females compared to male patients.
The prevalence of the uropathogens in diabetic patients is shown in Fig. 1. The results from the reviewed reports of the patients showed an extremely high prevalence of E. coli infections (78.8%, 67 cases) whereas Streptococcus sp. were found in 8 cases proportion of Acinetobacter and Klebsiella pneumoniae were 3.5% and 2.4% respectively while of the other pathogens accounted for 5.9% of infections.
Table 1: Frequency distribution of patients according to pathogens. sex and age range
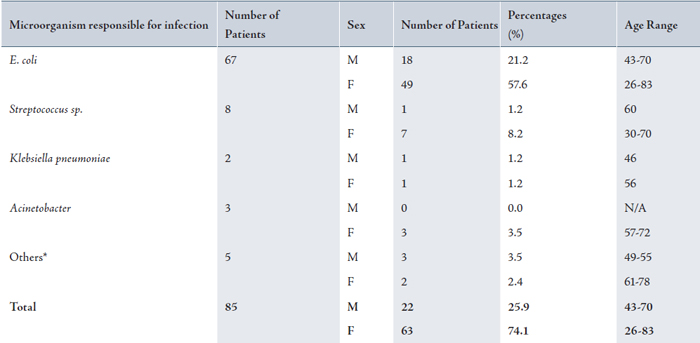
F: Female; M: Male; Others* = Enterobacter sp., Hafnia alvei, Pseudomonas sp., Staphylococcus aureus
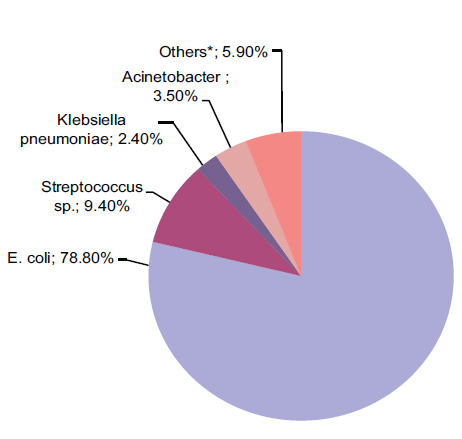
Figure 1: Prevalence of various pathogens responsible for UTI of diabetic patients in Dhaka, Bangladesh.
The resistance pattern of the discussed antibiotics is summarized in Fig 2. E. coli exhibited high resistance with amoxicillin and ciprofloxacin with 94% and 79% resistance respectively. All the cephalosporins showed moderate activity against the E. coli infection; cephradine, cefixime, ceftriaxone, and cefepime exhibited 68.7%, 62.7%, 61.2%, and 46.3% resistance respectively. Gentamicin demonstrated only 26.9% resistance while meropenem showed no resistance at all. Amikacin also proved to be very active against E. coli with only 3% resistance and so did nitrofurantoin with just 11.9% resistance.
Streptococcus sp. on the other hand, showed an overall greater resistance than E. coli. Streptococcus sp. exhibited most resistance with gentamicin (87.5%), amikacin (75%) and ciprofloxacin (75%). Average resistances were observed with amoxicillin (62.5%) and the cephalosporins which were cephradine (50%), cefixime (50%), ceftriaxone (50%) and cefepime (37.5%). Though meropenem was very effective against Streptococcus sp, showing only 25% resistance. The lowest resistance was observed with nitrofurantoin which exhibited only 12.5% resistance.
Both Acinetobacter and Klebsiella pneumoniae showed moderate resistance with amoxicillin (33.3% and 100% respectively) and all the cephalosporins with cephradine (33% vs. 50%), cefixime (33.3% vs. 50%), ceftriaxone (33.3% vs. 50%), and cefepime (33.3% vs. 50%). Stronger resistance was observed with nitrofurantoin (10% vs. 50%). Meropenem and Amikacin showed no resistance among these two strains while the resistance for gentamicin was 0% vs. 50%. It was also revealed that Acinetobacter is very susceptible to ciprofloxacin with no resistance at all; however the drug is completely useless for Klebsiella pneumoniae infections.
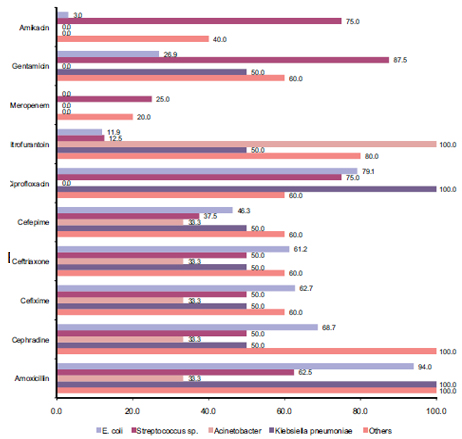
Figure 2: Pattern of antibiotic resistance of various pathogens found in urine culture of diabetic patients. Overall resistance pattern in decreasing order of various commonly used antibiotics is Amoxicillin (78.0%)>Ciprofloxacin (62.8%)>Cephradine (60.4%) >Cefixime (51.2%)>Ceftriaxone (50.9)>Nitrofurantoin (50.9%)> Cefepime (45.4%)>Gentamicin (44.9%)>Amikacin (23.6%)> Meropenem (9%).
DISCUSSION
This study confirmed that overall, UTI is more common in females than males (3 times more) agreeing with other previous studies.9,14 E. coli and Streptococcus sp. were found to be the major group of pathogens responsible for the infections which also support other research reports from other countries.15-18 In the diabetic group of patients, the age range of infected females (26-83 years) was also much broader compared to that of males (43-70 years). E. coli was the most prevalent pathogen among the UTI patients as confirmed by other studies.14 This study revealed that after E. coli and Streptococcus sp. were the most prevalent pathogens followed by Acinetobacter and Klebsiella pneumoniae.
When the effectiveness of various antibiotics was studied for UTI based on the resistance patterns, it pointed out that the most effective antibiotic overall is meropenem followed by amikacin. The once blockbuster antibiotics such as amoxicillin, ciprofloxacin, cephradine showed most resistance with 78.0%, 62.8%, 60.4% resistance respectively and cephalosporins such as cefixime, cefepime and ceftriaxone showed around 50% resistance. These findings are clearly alarming as our country could be running out of effective antibiotics if this trend continues.
E. coli exhibited a 94% resistance to amoxicillin and a striking 79% resistance to ciprofloxacin, which should be a matter of consideration. Resistance to cephalosporins was also well above 60% in most cases. E. coli was most inhibited by meropenem, amikacin and nitrofurantoin. Streptococcus showed similar patterns but it exhibited a profound resistance of 87.5% to gentamicin and also an alarming 75% to amikacin. Acinetobacter and Klebsiella pneumoniae also showed similar resistance patterns to that of E. coli. Other pathogens, including Enterobacter sp., Hafnia alvei, Pseudomonas sp. and Staphylococcus aureus exhibited complete resistance to amoxicillin, cephradine. Resistance to nitrofurantoin was also 80%. Most other commonly used antibiotics including the cephalosporins showed more than 50% resistance. Hence, the best acting antibiotic was found to be meropenem.
CONCLUSION
The significance of the study lies in the determination of common pathogens in diabetic patients with UTI and the resistance pattern of antibiotics so that physicians and pharmacists get the proper information rationalizing the use of antibiotics. This study also demonstrated that antibiotics including amoxicillin, ciprofloxacin, cephalosporins (1st generation, 2nd generation, 3rd generation in some cases) and nitrofurantoin are mostly resistant to pathogens with few exceptions including gentamicin, amikacin and meropenem (most effective one). Thus this study should provoke policy makers to formulate an antibiotic policy for rational use of antibiotics.
ACKNOWLEDGEMENTS
The authors are kind enough to show their gratitude to the microbiologists and technicians of Popular and Medinova Diagnostic center who helped a lot in different ways. The authors reported no conflict of interest and no funding was received on this work.
|