Aggressive angiomyxoma (AA) is a rare soft-tissue tumor that is typically found in the perineum of females of reproductive age.1,2 Steeper and Rosai1 described this disease for the first time in 1983. Since that time hundreds of cases have been reported in the literature. Commonly, the tumor is misdiagnosed as a Bartholin’s cyst, abscess, or hernia because most patients complain of pain in the perineum, labia, or pelvis.3 Surgical excision is the treatment of choice for AA; however, it has a high rate of recurrence.4 Because of its typical imaging appearance and high recurrence rate, cross-sectional imaging is important in the diagnosis and long-term follow-up of the disease. We report a case of AA in a 38-year-old woman with typical magnetic resonance imaging (MRI) features. We also present the typical radiological features of this disease based on a review of the literature.
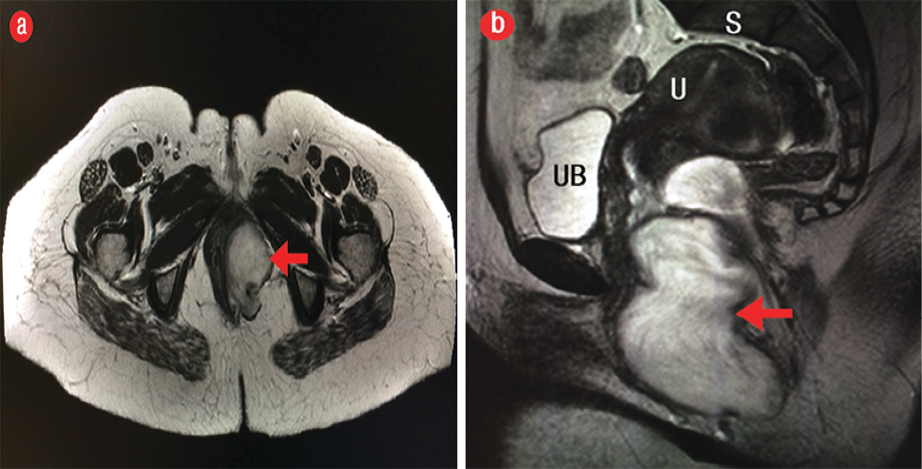
Figure 1: (a) Axial and (b) coronal T2-weighted magnetic resonance imaging revealed a hyperintense mass in the left perineal region (red arrows). UB: urinary bladder, S: sacrum, U: uterus
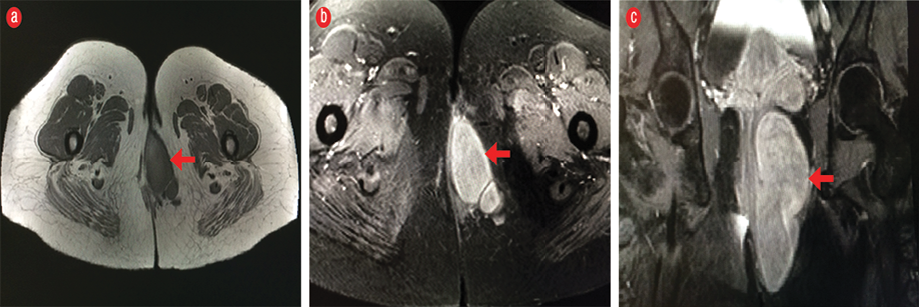
Figure 2: (a and b) Axial pre-contrast and (c) coronal post-contrast fat-suppressed T1-weighted magnetic resonance imaging show avid enhancement (arrows) after the administration of intravenous gadolinium contrast.
Case report
A 38-year-old healthy woman presented with a three-year history of a painless swelling on the left labia majora. The swelling was gradually increasing in size. There was no history of discharge. On physical examination, the patient was not pale or jaundiced, and the examination of head, neck, chest, and abdomen was unremarkable. Local examination revealed a non-tender 4 × 8 cm swelling in the left labia majora. Blood workup including tumor markers, and liver and renal function tests were unremarkable. The clinical diagnosis was Bartholin’s cyst.
The patient was evaluated with contrast-enhanced MRI of the pelvis, using 3.0 Tesla scanner, which showed a large branching mass measuring
11 × 5.4 × 3.8 cm that was confined to the left perineal region with no evidence of invasion into adjacent structures. The lesion was isointense relative to muscle on the T1-weighted image and hyperintense on the T2-weighted image with a swirled appearance [Figure 1]. The mass enhanced avidly after the administration of intravenous gadolinium contrast [Figure 2]. The patient underwent surgery to remove the tumor. The histopathology results confirmed the diagnosis of AA.
Discussion
AA is a rare mesenchymal tumor that predominantly affects the perineum and pelvis of females of childbearing age, usually between the second and fourth decade of life.1 The most common clinical presentation of AA is a vulvar or vaginal soft mass, which is usually mistaken as Bartholin’s duct cyst, lipoma, vulvar mass or vulvar abscess, Gardner’s duct cyst, vaginal cyst, vaginal prolapse, or levator hernia.3
AA is a benign tumor; however, because it is associated with a high rate of local recurrence after surgery, it is called aggressive. Up to 72% of cases recur locally two to four years after surgical excision.4 The best management of AA is wide local excision of the tumor with a clear excision margin on histology in order to reduce the risk of recurrence.5 On cross section imaging, the tumor is typically a well-defined mass, displacing rather than infiltrating adjacent organs (such as the urethra, vagina, anal sphincter, and rectum).6
On CT, AA is hypodense relative to muscles with a layering or swirled pattern after contrast administration.7 On MRI, owing to high water content and loose matrix, AA is isointense relative to muscle on T1-weighted imaging, hyperintense on T2-weighted imaging, and enhanced avidly after the administration of gadolinium indicating hypervascularity. Enhancement of the fibrovascular stroma of the tumor results in the characteristic layered pattern or swirled appearance. This has been described in 83% of cases on T2-weighted MRI, or on T1-weighted MRI following contrast administration.6,8 Preoperative CT or MRI is very useful in assessing the extent of tumor, which is crucial in planning the surgical approach to remove the tumor completely and to reduce the recurrence rate.
The high recurrence rate makes MRI an ideal imaging modality for follow-up.6 Our patient had a follow-up MRI after six months, which showed an enhancing lesion at the surgical site suggestive of tumor recurrence. The patient declined treatment with radiotherapy. She was started on hormonal treatment but was unable to tolerate the side effects and the treatment was stopped. The patient was followed-up with MRI of the pelvis every three months for one year, and then once annually. The size of the tumor remains unchanged.
Conclusion
Although AA is a rare tumor, it has characteristic imaging features of swirled or layered internal architectures on contrast CT and MRI. Preoperative diagnosis is possible if the radiologist is aware of this diagnosis and the characteristic CT and MRI features. Cross-sectional imaging is also important for determining the extent of the tumor in order to optimize the surgical approach and reduce the incidence of recurrence.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Smith HO, Worrell RV, Smith AY, Dorin MH, Rosenberg RD, Bartow SA. Aggressive angiomyxoma of the female pelvis and perineum: review of the literature. Gynecol Oncol 1991 Jul;42(1):79-85.
- 2. Fetsch JF, Laskin WB, Lefkowitz M, Kindblom LG, Meis-Kindblom JM. Aggressive angiomyxoma: a clinicopathologic study of 29 female patients. Cancer 1996;78(1):79-90.
- 3. Elchalal U, Lifschitz-Mercer B, Dgani R, Zalel Y. Aggressive angiomyxoma of the vulva. Gynecol Oncol 1992; 47:260-262.
- 4. Salman MC, Kuzey GM, Dogan NU, Yuce K. Aggressive angiomyxoma of vulva recurring 8 years after initial diagnosis. Arch Gynecol Obstet 2009 Sep;280(3):485-487.
- 5. Simó M, Zapata C, Esquius J, Domingo J. Aggressive angiomyxoma of the female pelvis and perineum. Report of two cases and review of the literature. Br J Obstet Gynaecol 1992 Nov;99(11):925-927.
- 6. Jeyadevan NN, Souhaib SA, Thomas JM, Jeyrajah A, Shepherd JH, Fisher C. Imaging features of aggressive angiomyxoma. Clin Radiol 2003;58(2):157-162.
- 7. Heffernan EJ, Hayes MM, Alkubaidan FO, Clarkson PW, Munk PL. Aggressive angiomyxoma of the thigh. Skeletal Radiol 2008 Jul;37(7):673-678.
- 8. Outwater E, Marchetto BE, Wagner BJ, Siegelman ES. Aggressive angiomyxoma: findings on CT and MR imaging. Am J Roentgenol 1999;172(2):435-438.