Hamartomas are disorganized but benign masses composed of cells indigenous to the involved site. Once thought to be a developmental malformation, they may have clonal chromosomal aberrations.1 Hamartoma has been reported in almost all organs but is rare in the head and neck region, especially the pharynx.2–3 Pharyngeal hamartomas can be associated with specific syndromes such as Cowden disease and Peutz-Jeghers syndrome.4 Considering the rarity of the lesion, especially in children, we report a case of hamartoma of the palatine tonsil in a six-month-old infant.

Figure 1: Clinical photograph showing a polypoid mass protruding over the tongue of a six-month-old infant.

Figure 2: Gross photograph of tonsillectomy specimen showing a smooth whitish slender pedunculated mass.
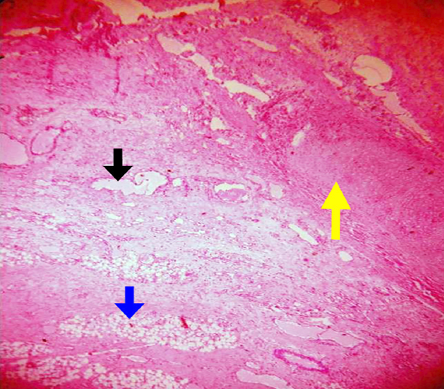
Figure 4: Microscopic photograph of stroma showing dilated lymphatic channels (black arrow) along with adipose tissue (blue arrow) and a focus of cartilage (yellow arrow). Magnification = 400 ×.
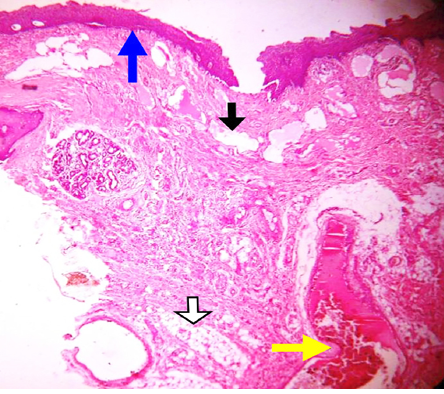
Figure 3: Microscopic photograph showing a stratified squamous epithelium lining (blue arrow) along with lymphatic channels (black arrow), adipose tissue (white arrow), and blocked blood vessel (yellow arrow). Magnification = 400 ×.
Case report
A six-month-old male infant presented to the emergency room of North Bengal Medical College with acute onset respiratory distress. He had a history of recurrent respiratory tract infections and was unable to feed properly since birth.
On clinical examination, bilateral equal vesicular breath sounds were auscultated, and there was no adventitious sound. Cervical lymphadenopathy was absent and systemic examination was unremarkable. The attending pediatrician noticed a mass protruding over the tongue and the patient was referred to an ENT surgeon. Indirect laryngoscopy showed a pedunculated polypoid mass in the throat arising from the left palatine tonsil [Figure 1]. The right tonsil was normal on examination. It was freely mobile and was neither enlarged nor inflamed. Complete hemogram and chest radiograph were normal. He underwent tonsillectomy along with removal of the polyp under general anesthesia after initial stabilization. Intraoperative and postoperative periods were uneventful.
The surgically removed specimen of the tonsillar polyp was sent for histopathological examination. On gross examination, a pedunculated whitish polypoid mass measuring 6 × 2 cm was seen [Figure 2]. Cut section was homogeneous and glistening with yellowish areas. Histopathological examination of hematoxylin and eosin stained slides showed a keratinized stratified squamous epithelium-lined polyp [Figure 3]. Stroma showed dilated lymphatic channels and clusters of mature adipocytes. One focus showed mature cartilage [Figure 4]. No evidence of any malignancy was seen. Based on the features described above, a diagnosis of hamartoma of palatine tonsil was made.
Discussion
The Greek word ‘hamartion’ gave birth to the term hamartoma, which means bodily defect.5 Benign tonsillar lesions include squamous papillomas, inclusion cysts, lymphoid polyps, lymphangiomas, fibromas, and lipomas.1,6 Polypoidal lesions of the tonsils are rare and have been reported using various nomenclature: amongst these hamartomas are
even rarer.5
Previous cases of hamartoma of palatine tonsils are reported mainly in elderly patients who usually present with sore throat, dysphagia, and continuous foreign body sensation.5 During surgery, difficult intubation may lead to the incidental discovery of a few cases. Our patient was only six-months-old, presenting to the emergency room with acute onset respiratory distress. Newborn infants have a variable ability to breathe through their mouths.7 The ability to breathe through their mouth increases with age. If there is any nasal blockage due to respiratory infection, mouth breathing serves as an alternative. Since this child had a mass in the oral cavity, compromising the oral airway, he developed breathing difficulty during respiratory infections.
The lesions described in previously reported cases were slow growing – a feature of hamartoma. In our case, the infant was only six months old at presentation indicating rapid growth of the mass. However, considering the age of the child and absence of any documentation regarding the previous size of the lesion, the possibility of the mass being congenital cannot be excluded.
Hamartoma of oropharynx and hypopharynx are pedunculated as in our case.8 The histopathological picture of our case was similar to the case reported by Kardon et al,9 and comprised of mature adipose tissue, dilated blood vessels, and mononuclear inflammatory cell infiltrate. Some may show gastric mucosa.10 Although hamartoma is a benign lesion, malignant transformation may develop rarely.11
Treatment is complete surgical excision and follow-up.4 Vascular lesions or those in contact with cerebral fossa are conditions suitable for embolization before surgery.12 Incomplete excision is associated with a risk of recurrence.3 In our case, the lesion was limited to the tonsillar parenchyma and did not infiltrate to adjacent structures. The child was followed-up for about one year without any evidence of recurrence.
Conclusion
We described the case of a six-month-old infant presenting with acute onset respiratory distress due to a fast growing (or more likely congenital origin) hamartoma arising from the palatine tonsil. It is important to perform a thorough examination of the respiratory system, including a local examination of the oral cavity in any patient presenting with respiratory distress. Rare benign lesions like hamartoma originating in the oral cavity, even in infants, can cause such a presentation.
Disclosure
The authors declared no conflicts of interest.
Acknowledgements
The authors are grateful to Dr. Bidyut Krishna Goswami, professor and head of the Department of Pathology, North Bengal Medical College, West Bengal, for his expert opinion and overall guidance.
references
- 1. Stricker TP, Kumar V. Neoplasia. In: Kumar V, Abbas AK, Fausto N, Aster JC, editors. Robbins and Cotran Pathological Basis of Disease. 8th ed. Pennsylvania; Elsevier Inc; 2010. p. 259-330.
- 2. Shirazi N, Bist SS, Selvi TN, Harsh M. Spectrum of sinonasal tumors: A 10-year experience at a atertiary care hospital in north India. Oman Med J 2015 Nov;30(6):435-440.
- 3. Sethi A, Sethi D, Bansal R. True hamartoma of the tonsil. Indian J Otolaryngol Head Neck Surg 2011 Jul;63(Suppl 1):99-101.
- 4. Meirelles RC, Neves-Pinto RM. Mesenchymal Hamartoma of the Tonsil in a Child: A Case Report. Arch Otorhinolaryngol 2005 Jul-Sep;9(3):239-241.
- 5. Lyndog RH, Devaraju S, Leena JB. A Pedunculated Hamartomatous Polyp of the Palatine Tonsil. Iranian J Pathol 2013;8(1):45-47.
- 6. Lupovitch A, Salama D, Batmanghelichi O. Benign hamartomatous polyp of the palatine tonsil. J Laryngol Otol 1993 Nov;107(11):1073-1075.
- 7. Haddad J Jr. Congenital disorders of the nose. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson textbook of Pediatrics. 18th ed. Philadelphia: Saunders; 2007. p. 1742-1744.
- 8. Wind J, Lecluse FL. Hamartoma of the hypopharynx. Arch Otolaryngol 1983 Jul;109(7):495.
- 9. Kardon DE, Wenig BM, Heffner DK, Thompson LD. Tonsillar lymphangiomatous polyps: a clinicopathologic series of 26 cases. Mod Pathol 2000 Oct;13(10):1128-1133.
- 10. Hüttenbrink KB, Stoll W. [Stridor in the neonatal period in heterotopic gastric mucosa of the hypopharynx]. Laryngol Rhinol Otol (Stuttg) 1987 Feb;66(2):67-69.
- 11. Shara KA, al-Muhana AA, al-Shennawy M. Hamartomatous tonsillar polyp. J Laryngol Otol 1991 Dec;105(12):1089-1090.
- 12. Kerber C, Cromwell L. Presurgical embolization of neurogenic hamartoma in an infant. A case report. Radiology 1975 Nov;117(2):397-398.