| Introduction
Hepatitis B virus (HBV) infection is one of the most common infectious diseases in the world. The global prevalence of HBV carriers varies widely, from high (10-20%) in southeast Asian and China, to intermediate (2-7%) in the Mediterranean region, Japan, Central Asia, and the Middle East, and low (<2%) in the United States, Canada, Western Europe and Australia.1 It is estimated that over 35% of Iranians have been exposed to HBV. The prevalence of hepatitis B surface antigen (HBsAg) in Iran, a Middle Eastern country, varies from 1.7% in Fars to over 5% in Sistan-Balouchestan. However, the global prevalence is lower than 3%.2
One of the most important routes for HBV transmission is from asymptomatic carrier mothers to their infants. Mother to child transmission occurs often in the uterus or through exposure to blood or blood contaminated fluids at or around birth. Such perinatal transmission is believed to account for 35% to 50% of HBV carriers.3 It has been concluded that over 50% of Iranian carriers have contracted the infection perinataly, making this the most likely route of HBV transmission in Iran.2
In the Islamic Republic of Iran (I.R. Iran), mass vaccination of neonates against HBV infection began in 1993 as a national program in routine neonatal care. The program was supposed to affect the prevalence rate of HBV infection through the country and decrease the rate of infection. Therefore, a recent study in Iran showed that the rate of hepatitis B carriers varied between zero and 3.9% with an average of 1.7%.4 Also, 3.6% of the population was HBsAg positive, putting Khorassan among the highly affected areas in Iran.4,5 HBV prevalence has decreased dramatically in the Iranian population during the last decade.5 Generally, it is estimated that approximately 1.5 to 2.5 million people are suffering from HBV infection in I.R. Iran, and some of them are carriers who may unintentionally transmit the infection to others.4,5
The age at which HBV infection occurs influences the long-term outcome and determines the primary targets of a vaccination program. Thus, perinatal transmission from mother to child soon after birth results in approximately 90% chronic carriage, with long-term complications of chronic hepatitis, cirrhosis and hepatocellular carcinoma, leading to death by middle age, particularly among men.5
Infected children have a 25% or greater chance of dying from primary hepatocellular carcinoma or liver cirrhosis.6 To eliminate the risk of perinatal transmission of HBsAg from mothers to their infants; a program of combined active and passive immunization has been established.7 Infants born to HBsAg positive mothers are immunized at birth with Hepatitis B Immunoglobin (HBIG) and HBV vaccine, and then subsequent hepatitis B vaccination at 1 and 6 months of age.8 The effectiveness of HBIG and HBV vaccines vary in various parts of the world.9,10
Evaluation of Serologic markers and risk factors in HBV infected people is important for designing the strategies to control the disease. The compliance and efficacy of the immunoprophilaxis program have not been followed rigorously in scientific reports until now. This study assesses the impact of HBIG and HBV vaccine in children born to HBsAg positive mothers in Amol, Mazandaran province, Northern Iran. Children detected with HBsAg, Antibody to HBV surface antigen (Anti-HBs) and antibody to hepatitis B core antigen (Anti-HBc) were assessed.
Methods
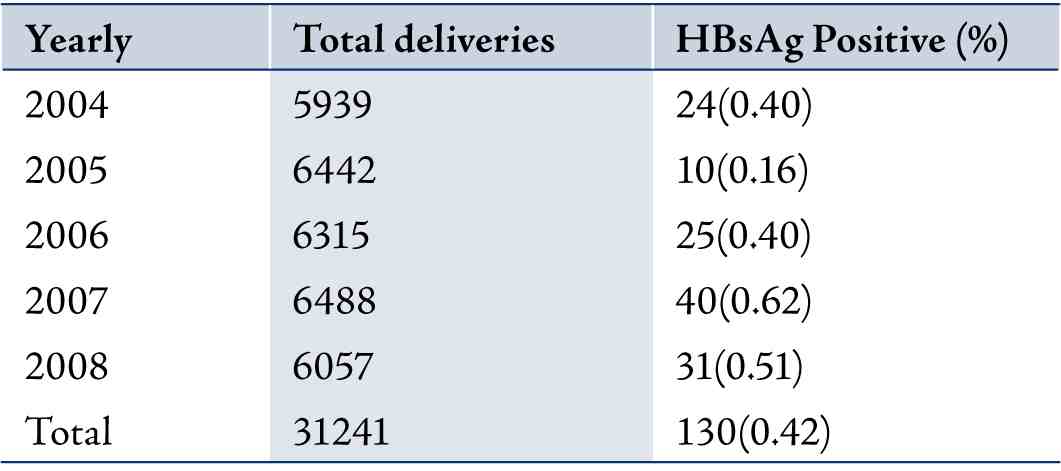
Amol is located in Mazandaran province in the north of Iran, near the Caspian Sea and is home to around 400000 residents; accounting for approximately 0.6% of the general population of Iran.11 Approximately 1.65% of Amol’s inhabitants were persistently infected with HBV in the past.12 During the 5 years from 2004 to 2008, 31241 pregnant women were tested for HBsAg and 130 (0.42%) were detected during their pregnancy. All children born to HBsAg positive mothers underwent immunoprophilaxis and were followed for markers of HBV infection. Attempts were made to contact all HBsAg positive women reported to Amol Health Center and maternity hospital, between April 1, 2004 and December 21, 2008. All mothers involved gave their written informed consent on testing their children for HBV markers and were enrolled into the study from September 2009.
Serum samples were taken from the attending children aged as follows; less than 13 months, 13-24, 25-36, 37-48 and 49-60 months. During the 5 year-studied period from 2004 to 2008, of the 95 children enrolled into the study; 53 children were aged less than 24 months and 42 children were aged between 25 to 60 months. The infants of mothers found to be HBsAg positive were given 0.5 ml Hepatitis B Immune Globulin (Talecris Biotherapcutics, USA) and 0.5ml HBV vaccine (Hepavax-Gene, Green Cross Vaccine Crop, Korea) intramuscularly at the time of delivery.
The second and third doses of the vaccine were injected at 1 and 6 months of age (according to Iran’s Ministry of Health Expanded Program on Immunization) at the local Health Services center. The youngest child enrolled into the study was 9 months of age. All children were tested for HBsAg and for the corresponding antibodies (anti-HBs) and anti-HBc. An informed consent for testing of HBV markers in coded serum samples from the children was obtained from their legal guardians.
For the detection of HBsAg, anti-HBs and anti-HBc, commercially available enzyme immunoassay kits (BIOKIT, S. A. Barcelona-Spain) were used. Immunogenicity was assessed using anti-HBs titers 9 months after birth. A value ³10 mIU/ml in terms of anti-HBs concentrations was considered to be protective level. Statistical analyses were done using the Chi Square (X2) and Fisher’s exact tests to analyze the data obtained by SPSS 11.5 software. The differences or association with p<0.05 were considered statistically significant.
Results
All the expectant mothers in Amol were tested for HBsAg in serum and much of the data were recorded from 2004 to 2008, with results summarized in Table 1. Of the 130 deliveries from the expectant mothers, only 95 infants participated in the study. Therefore, 95 cases who received immunoprophylaxis during the 5 years studied period from 2004 to 2008 participated in the study and their outcomes are shown in Table 2. Table 1 also shows the average prevalence positivity of HBsAg at delivery (0.42%).
Table 1: Yearly deliveries and expectant mothers tested for HBsAg in Amol, Mazandaran province, north of Iran.
Of the 95 subjects enrolled, 50.5% were male. The data showed that among the 95 children born to HBsAg positive mothers who received immunoprophylaxis, 1.05% were HBsAg positive, suggesting that these children were infected with HBV two years after birth despite immunoglubin and hepatitis B vaccine.
Table 2: Prevalence of HBV serologic markers in children born to HBsAg positive mothers by Age group.
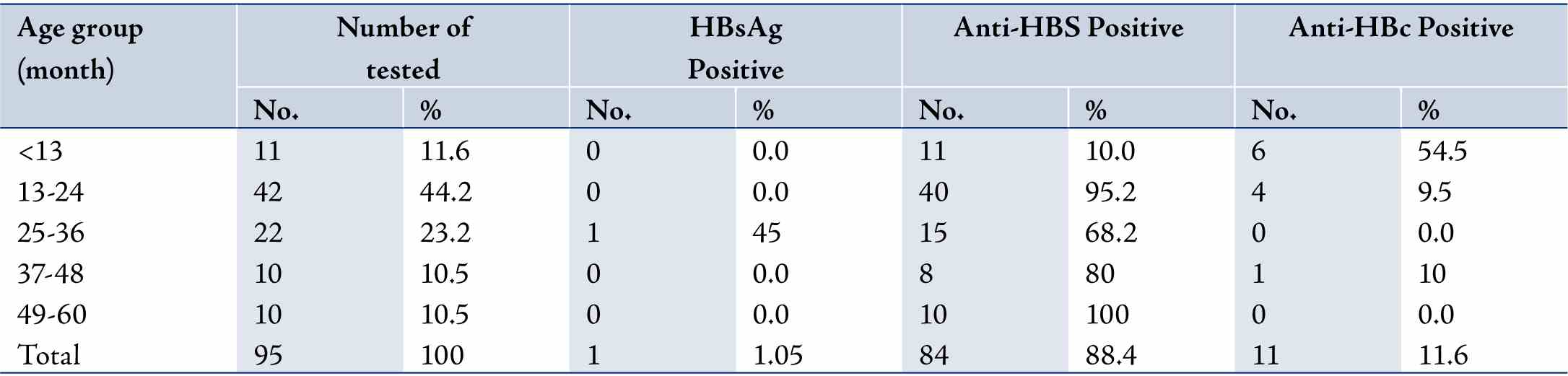
Table 3. Responder Rate of Anti-HBs in children born to HBsAg positive mothers by Age group.
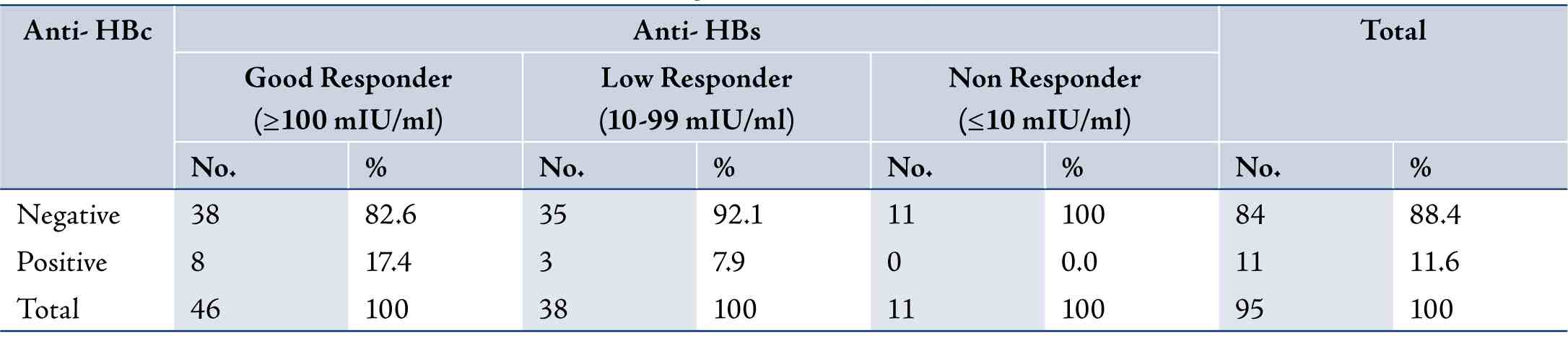
Table 4: Responder Rate of Anti-HBs in children born to HBsAg positive mothers by Age group.
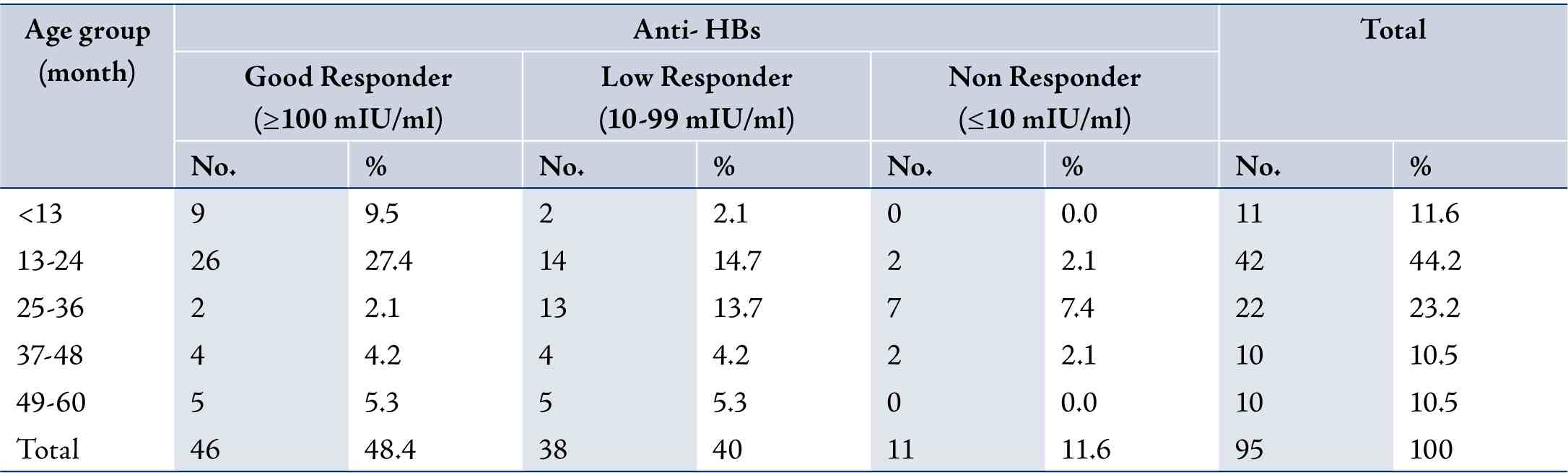
From the 94 children who were not infected, 11 (11.6%) had anti-HBs levels below 10 mIUml at the time of the serotest. Patients with Anti-HBs levels ≤10 mIU/ml were categorized as a Non Responders, while Anti-HBs levels between 10 and 99 mIU/ ml were categorized as low Responders and levels ≥100 mIU/ml were considered as Good Responders to the immunization. Eleven children (11.6%), had previous exposure to HBV, as demonstrated by the presence of anti-HBc at the time of the study (Table 3), and among them, 10 children were aged less than 25 months. (Table 2)
On the other hand, 84 children (98%) were not previously exposed to the infection, as confirmed by the absence of anti-HBc; thus 73 of them (86.9%) exhibited what would be considered as protective concentrations of anti-HBs ≥10 mIU/ml. (Table 4)(
The Fisher’s Exact test showed a significant association between the rate of seropositivity for anti-HBs and age group (p=0.0001). Thus, 42 boys (44.2%) and 42 (44.2%) girls were anti-HBs positive. The rate of seropositivity for anti-HBs and anti-HBc did not differ in neither males nor females (p=0.48).
Discussion
Hepatitis B virus (HBV) infection is the main cause of chronic liver disease in Iran.2,13 The epidemiology of HBV infection in Iran has changed during the last two decades,2 and infantile vaccination with high coverage is the main cause for this change.14,15
Amongst the target groups for vaccination in the current Iran selective program, infants born to HBsAg seropositive mothers are at highest risk of acquiring hepatitis B infection. Universal vaccination of all neonates against hepatitis B virus has been implemented in the Islamic Republic of Iran since 1993 (Ministry of Health report). The prevalence of HBsAg in children has decreased from 1.3 to 0.9% within 6 years of starting the Expanded Program on Immunization (EPI).5
Perinatal transmission of HBV from mother to infant occurs during the course of pregnancy or at the time of delivery. Approximately 5% of infants are infected in the uterus and approximately 95% at the time of birth. Infants born to HBsAg positive carrier mothers (especially in HBeAg positive cases) have a contracting chronic hepatitis B infection and of possible subsequent progression to chronic carrier state, cirrhosis and hepatocellular carcinoma.8
Many studies have found an association between recording the maternal HBV status in delivery room records and the timely administration of HBIG.16 Better rates of immunization at birth and of completion have been documented in programs that provided reminders to mothers to report their HBV status at delivery; reported maternal HBsAg status on new-born metabolic screening cards; provided reminders to antenatal care providers to report maternal HBsAg status to the delivery hospital; and those that have adopted computerized tracking systems for carriers and their children.17
When HBV vaccine and Hepatitis B hyper immunoglobulin were used together in the neonatal period, 94% protection was achieved.18 It is important to identify the children who need additional doses, because of the potential risk of transmission after the perinatal period from the mother or from other HBV infected household members.6-8
Hepatitis vaccination strategies may vary from one country to another depending on HBV endemicity, predominant transmission modes of the infection, age at time of infection, and the availability of healthcare resources.2
In our study, 0.42% of deliveries and expectant mothers were HBsAg positive. However, HBsAg positivity rate differs among countries. In Nigeria, HBsAg positivity was found to be 11.6% in pregnant women; while in Sierra Leone, it was reported to be 11.3%; 10% in Hong Kong; 0.44% in the Netherlands and in 1.4% Germany.19-23 HBsAg was detected in 0.63% of expectant mothers in Shizoka.24 Other studies in Japan reported that 1.2% of expectant mothers in Iwate were HBV carriers. In another study, the rate of HBsAg and anti-HBs in the children was reported to be 6.5% and 93.5%, respectively.25
Our results confirm the importance of immunoprophylaxis in newborn babies with HBsAg-positive mothers, while documents show the possibility of failure of the preventive measures. In our study, 11 cases of perinatal transmission were observed; the causes of this vaccination failure were not easy to determine. Eleven children (11.6%) acquired the infection as revealed by the presence of anti-HBc.
Breakthrough infections, due to S-gene mutants of HBV, have occasionally been reported among children born to HBsAgpositive mothers, but at the present time, such mutants do not pose a public health threat.26
Asymptomatic infection characterized by the presence of anti-HBc in the absence of HBsAg viremia (‘‘mild breakthrough infections’’) have been documented in vaccinated individuals.27 Rates of breakthrough infections cannot easily be compared with other evaluations, but the rate of 1.05% seen in those tested is different to the rate expected from vaccine efficacy studies.28
In our study, the rate of non-responder (anti-HBs negative) in children was 11.6%. These children were at risk of acquiring infection. Whereas, in 2002, Roshan et al. reported a 6.5% HBsAg in children born to HBV carrier mothers and 36.6% of these children were anti-HBs negative (non-responder).10 In a study conducted by Darmiani et al. on 22 neonates from HBsAg positive mothers, HBsAg rate was zero.29
Several studies have revealed a much lower non-response rate than the rate in the current study. A study performed by Gallo et al. on 85 infants born to HBsAg positive mothers showed that only two neonates (2.4%) were non-responders.30 While Poovorawan et al. in 1997, reported a 3.8% non-responder rate in neonates born to HBsAg positive mothers.31
A previous study conducted in Iran showed an efficacy rate of 85.7%.14 In the present study however, the figure for efficacy was 88.4%. Another study in Iran for HBsAg, anti-HBs and anti-HBc in 60 children born to HBsAg positive mothers showed efficacy rates of 3.6%, 85.7% and 38.7%, respectively.15 A Vietnamese study reported 92.2% seroprotection in 53 vaccinated infants.32
Also, a 15-year study on 1030 Japanese babies born to HBsAg positive carrier mothers who had received hepatitis B immunoglobulin at birth and 2 months after as well as vaccines at 2, 3 and 5 months after birth reported an efficacy rate of 95.1% and the carrier state developed in the remaining 4.6%.24 Marino et al. in Canada showed the rate of HBsAg and anti-HBs in children born to HBsAg positive carrier mothers were 2.3%, 87.9% and 5.1%, respectively.33
These studies demonstrated that HBsAg in children born to HBsAg positive mothers is different in various part of the world. In the current study, one case (10.5%) was HBsAg positive. In a study conducted by Roome et al. (1994-1997),34 and a study in Taiwan reported that 1.3% and 2.4% of infants were HBsAg carriers, respectively.35
Infants who become chronic HBV carriers despite perfect immunoprophylaxis may be have been infected in the uterus, their mothers may have a high virus load, or they may have been infected through vaccine-escape virus mutants.6,8 This infection may occur transplacentally, thus HBIG and HBV vaccine cannot prevent the infection.
In our study, of the 11 cases, 10 cases with anti-HBc positive were more than 2 years of age, and the protection level (rate of anti-HBs) in these children was 88.4%. This rate seems lower compared to rates reported in other studies. Also, in all of the 11 anti-HBc positive children, there was no significant association between the rate of seropositivity for anti-HBc and anti-HBs (p•0.05).
Anti-HBc can remain for long time in children born to HBsAg positive mothers. However, if only anti-HBc was detected in children 2 years of age, the infection may become apparent at an earlier stage. Some researchers have reported that the lack of maternal antibody to hepatitis B core antigen (anti-HBc) was strongly correlated with the transmission of HBV infection.35,36
The results from this study, although confirmed the effectiveness of the anti-hepatitis B vaccination, they highlights the need for post-vaccination follow-up, in order to prolong protection and calculate the potential need for booster doses. The study also conveyed the importance of maintaining active surveillance with the aim of improving the follow-up of chronic carriers and sensitizing families.
Conclusion
According to the study results, passive-active immunoprophylaxis in high risk children was effective and it is proposed that all children born to HBsAg positive mothers should be immunized against HBV. A study with a larger sample size is recommended.
Acknowledgements
This work was supported by a grant from Tehran University of Medical Sciences, Government of Iran. We would also like to thank Dr. Noushin Khayyer, Mr. Ali Hashemzadeh-Omran, Rahman Kazemi, Miss Zahra Saadatmand in Tehran and Miss Asadi-Pour in Amol (Imam Ali Hospital) for data collection and performing the laboratory tests, and Dr. Evangelin Foronda for English editing, and many thanks to Dr. Parsian for final editing.
|