|
Abstract
Splenic artery aneurysm (SAA) is a rare clinical entity that carries the risk of rupture and fatal hemorrhage. Ruptured SAA, especially during pregnancy has fateful consequences for the mother, foetus or both. The role of the Radiologist is very important in preventing mortality. A diagnosis of ruptured SAA should be considered in any pregnant patient who complains of sudden epigastric or upper abdominal pain, with or without shock. This is a report of two cases where the mothers were saved but the foetuses were lost.
Keywords: USG-abdomen doppler-study; Splenic artery aneurysm; MDCT interventional studies; Laparatomy.
Introduction
Splenic artery aneurysm (SAA) is a rare clinical entity that carries the risk of rupture and fatal hemorrhage. Ruptured SAA during pregnancy can be disastrous for both the mother and the fetus. Patients with SAA are usually asymptomatic until the aneurysm ruptures. Sudden severe epigastric or left upper quadrant pain heralds the onset of rupture of the aneurysm with immediate or delayed onset of hypovolemic shock. The size of the aneurysm is also an important factor in predicting rupture. An aneurysm of two centimeters in diameter is highly prone for rupture.
Initially, bleeding remains confined to the lesser sac, which then progresses to free intraperitoneal hemorrhage and shock, causing the patient to collapse. This may take anywhere between 6-96 hours. The initial phase where hemorrhage remains confined to the lesser sac provides vital time for diagnosis and preparation for intervention.1 In pregnancy however; the development of the shock is rapid and clinical suspicion followed by Ultrasound examination forms the mainstay in diagnosis and rapid mobilization of the patient to the operating theatre. Atherosclerosis and congenital defects of the arterial wall have been described to be the major causes of SAA. The treatment for ruptured SAA is aneurysmectomy with or without splenectomy.1
Case Report
Case No. 1
A 29-years-old female, in her 34th week of pregnancy, presented to the Accident & Emergency department with pain in the epigastrium and left hypochondrium. There was no other symptom or past history of similar complaints. On examination; the patient was pale with a rapid thready pulse (160 pulses per minute), systolic blood pressure was 60 mmHg, and diastolic blood pressure was 30 mmHg, the patient also reported cold and clammy extremities. Diagnostic Ultrasound (US) of the abdomen revealed hemoperitoneum. Exploratory laparotomy was carried out after hemodynamically establishing the patient with blood transfusion. There was approximately one and a half liters of blood in the free peritoneal cavity and the lesser sac was full of blood. On opening the lesser sac and evacuating the hematoma, the source of bleeding was identified to be the proximal end of a ruptured splenic artery aneurysm involving the distal third of the splenic artery. Proximal ligation with aneurysmectomy and splenectomy was carried out. Unfortunately, the fetus did not survive. The postoperative course was uneventful and the patient was discharged on the 9th postoperative day. She continues to do well.
Case No. 2
A 37-years-old female, in the 36th week of pregnancy, presented with pain in the epigastrium and left hypochondrium. There was no other symptom or past-history of pain. On examination; the patient was very pale with a rapid thread pulse (168 pulses per minute), systolic blood pressure was 60 mmHg, diastolic blood pressure was 40 mmHg, with cold and clammy extremities. US Abdomen revealed hemoperitoneum. Doppler study revealed no flow in the splenic hilum and a big clot was observed in the region of the splenic artery. Exploratory laparotomy was carried out after hemodynamically stabilizing the patient. There was around 2 liters of blood in the free peritoneal cavity and the lesser sac was full of blood. On opening the lesser sac and evacuating the hematoma, the source of bleeding was identified as the proximal end of a ruptured splenic artery aneurysm. Proximal ligation with aneurysmectomy and splenectomy was carried out. Cesarean Section was done to remove the dead fetus. The postoperative course was uneventful and the patient was discharged on the 9th postoperative day. The patient is doing well.
Discussion
Splenic artery aneurysm (SAA) is the most common type of aneurysm found in the splanchnic arterial bed and is only second in frequency to aortic and iliac artery aneurysms, among all intra-abdominal aneurysms (Figs. 1,2).2 More than 400 cases of SAA have been reported. The literature reports a 25% mortality rate for ruptured SAA.3 The mortality rate among pregnant women is disproportionately high (75%) with a fetus mortality rate of 95%. Twelve cases have been reported where both the mother and the fetus survive. Of all splenic artery aneurysms, 65% present in pregnant women and 50% rupture during pregnancy. The incidence of rupture of the aneurysm during pregnancy is as follows: 12% of SAA rupture during the first two trimesters; 69% during the third trimester, (both cases presented in the third trimester); 13% at childbirth; and 6% at puerperium.2-4 In 25% of cases, the phenomenon of "double rupture" is reported. Initially, the bleeding remains confined to the lesser sac for around 6-96 hours, followed by free intraperitoneal hemorrhage and collapse of the patient.1-3,5
Figure 1: Anatomical relations of splenic artery.
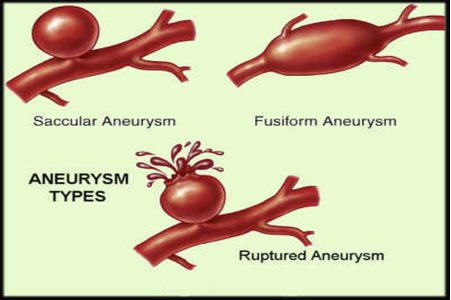
Figure 2: Tupes of splenic artery aneurysm
The etiology of true SAA is obscure. Atherosclerosis and congenital defects of the arterial wall have been described as the major causes of SAA, whereas others claim that atherosclerosis is a secondary event in SAA.1,6 Increased blood pressure is considered to promote aneurysm formation.1 Liver diseases with splenomegaly, repeated pregnancies (as in our cases), systemic hypertension and old age are certain clinical settings with a high incidence of SAA.1 Acute and chronic pancreatitis have are thought to be the major causes of pseudo aneurysm.1 Pseudo aneurysm often presents in a pancreatic pseudo cyst.3,6 During pregnancy, the uterus presses the aorta and the iliac arteries and the flow of blood in the splenic artery is increased.7 This increased blood flow may induce aneurysm formation in an already weakened arterial wall. Because the diameter of the uterus is bigger in the third trimester of pregnancy; most cases of ruptured SAA are noted during this period, as observed in our cases. Another factor postulated as being responsible for the increased incidence of rupture during pregnancy is the hormone relaxine, which probably weakens the arterial wall.1,2,5
The SAA measured about 3 cm and 4.2 cm with clots around, in the first and second cases respectively. Histologic examination of the vessel wall showed severe morphologic changes of degeneration. Apart from the history and clinical examination; Doppler ultrasound, Computerized tomography (Figs. 3), and Arteriography can help with the diagnosis.1,6

Figure 3: USG of ruptured SAA showing clots around
The management of ruptured SAA requires awareness and aggressive surgical approach. Aneurysmectomy with splenectomy or distal pancreatectomy with splenectomy, with ligation of the proximal and distal splenic artery or aneurysmectomy alone with splenic conservation are the procedures described.2,8 Splenic conservation is desirable but is difficult in the emergency setting with ruptured SAA,2,7 as in this cases. Angiography and embolization have been described for pseudoaneurysms and for unruptured true aneurysms.2
In the high-risk patients, arterial embolization using coils can be an effective early treatment,1,5,8 but arterial embolization in SAA secondary to pancreatitis was shown only to be palliative and needed surgical intervention as a definitive procedure.
Conclusion
Splenic artery aneurysm in a pregnant woman is an uncommon disease.9 Early consideration of ruptured SAA diagnosis significantly increases the chances of survival for both the mother and the fetus. Routine screening of the splenic artery by Ultrasound and Doppler should be considered in selective pregnant patients with predisposing factors like hypertension, multiparity, liver and pancreatic diseases. In both the cases presented; the mothers survived but the fetuses were lost.
Acknowledgements
We would like to thank Dr. Logesan Dhinakar, Urologist, Sultan Qaboos Hospital, Salalah and the Hospital Team of Sultan Qaboos Hospital, Salalah. No funding was received for this work.
References
1. Mattar SG, Lumsden AB. The management of splenic artery aneurysms: experience with 23 cases. Am J Surg 1995 Jun;169(6):580-584.
2. Holdsworth RJ, Gunn A. Ruptured splenic artery aneurysm in pregnancy. A review. Br J Obstet Gynaecol 1992 Jul;99(7):595-597.
3. de Vries JE, Schattenkerk ME, Malt RA. Complications of splenic artery aneurysm other than intraperitoneal rupture. Surgery 1982 Feb;91(2):200-204.
4. O’Grady JP, Day EJ, Toole AL, Paust JC. Splenic artery aneurysm rupture in pregnancy. A review and case report. Obstet Gynecol 1977 Nov;50(5):627-630.
5. Macfarlane JR, Thorbjarnarson B. Rupture of splenic artery aneurysm during pregnancy. m. J Obstet Gynaecol 1966 Aug;95(7):1025-1037.
6. Westcott JL, Ziter FM Jr. Aneurysms of the splenic artery. Surg Gynecol Obstet 1973 Apr;136(4):541-546.
7. Herbeck M, Horbach T, Putzenlechner C, Klein P, Lang W. Ruptured splenic artery aneurysm during pregnancy: a rare case with both maternal and fetal survival. Am J Obstet Gynecol 1999 Sep;181(3):763-764.
8. Barrett JM, Van Hooydonk JE, Boehm FH. Pregnancy-related rupture of arterial aneurysms. Obstet Gynecol Surv 1982 Sep;37(9):557-566.
9. He, Miao-Xia MD; Zheng, Rupture of splenic artery Aneurysm during pregnancy. Am J Forensic &Pathology March 2010 - Volume 31 - Issue 1 - pp 92-94
|