Correlation of Lung Function with Disease Activity
Rheumatoid Arthritis
Tarik Al-Assadi,1 Adnan Al-Shemery,2 Sami Salman3
Al-Assadi, et al. OMJ. 24, 84-88 (2009); doi:10.5001/omj.2009.20
ABSTRACT
Objectives: To find a correlation between Lung function with the disease activity in Rheumatoid arthritis (RA).
Methods: The study was carried out on 40 (35 female and 5 male) patients with active RA who fulfilled the ARA 1987 reversed criteria for the classification of RA. Patients with signs and symptoms of respiratory disease or chest injury were excluded from this study. The patients were all examined clinically by weighted and selective index for active synovitis and assessed for functional status of the follwing; ESR, Hb % level, pulmonary function tests including FEV1, VC, FEV,/ FVC and DLCO. Another group of 30 (27 female and 3 male) patients with active RA served as a control group.
Results: The results showed that Hb level ranged between (7-13.3 gm/dl), ESR ranged between 11-131 mm/hr and restrictive ventilatory defect was observed in 15 (37.5%) patients. Obstructive ventilator defect was presented in 10 (25%) patients. A decreased in DLCO was detected in 23 (51.5%) patients. There was a positive correlation between PETS with Hb%, ESR, Disease duration and activity of synovitis (P<0.005).
Conclusion: Lung function can be used to stratify abnormalities in a clinically useful manner and can be used as an indicator of disease activity in RA.
From the 1Department of Orthopedic Surgery, Ministry of Health, Baghdad Iraq 2Department of Rheumatology, Ministry of Health, Baghdad, Iraq, 3Medical City, Baghdad Iraq.
Received: 30 Dec 2008
Accepted: 26 Feb 2009
Address correspondence and reprint request to: Dr. Tarik Al-Assadi, Department of Orthopedic Surgery, Ministry of Health, Baghdad Iraq
E-mail: dr.tarik_assadi@yahoo.com
INTRODUCTION
The first clinical description of Rheumatoid Arthritis (RA) is credited to Lander-Beauvais (Paris, 1800), but it was Alfred Baring Garrod (1859) who first used the term “Rheumatoid” arthritis.1 Rheumatoid Arthritis (RA) is a chronic inflammatory, systemic disease that produces its most prominent manifestations in the dirhrodial joints.2 The most common form of the disease is demonstrated by symmetrical, destructive and deforming polyarthritis affecting small and large synovial joints with associated systemic disturbances, in addition to a variety of extra-articular features and the presence of circulating antiglobulin antibodies (rheumatoid factors).3
The initial event inciting the inflammatory response is unknown. An infection’s etiology of RA has been vigorously pursued without yielding convincing evidence, genetic and environmental factors control the progression, extent and pattern of the inflammatory response and thereby responsible for the heterogeneous clinical features.2
The disease has a global distribution and involves all ethnic groups. The prevalence varies from 0.3% to 1.5% worldwide, while its prevalence in Iraq is 1%, and it is 2.5 times greater in females than in males.2
The physical examination of joints is considered to be pivotal in the assessment of RA disease activity; several articular indices have been developed in attempt to standardize the clinical measurement of joint destruction. These indices were formulated on empirical basis and are fundamentally different in their construction. They include: Ritchie articular index, American Rheumatism association index, Lunsbury index, and weighted and selective index.5,6,7,8 Other measurements of disease activity include the duration of morning stiffness, the patients’ assessment of pain (visual analog score), the patients global assessment of disease activity, the patients assessment of physical function (disability) and the acute phase reactant value namely; Erythrocyte Sedimentations Rate (ESR), C-Reactive protein (CRP) and hemoglobin concentration (Hb%).9
Pulmonary involvement is one of the most common extra-reticular manifestation of RA and the second cause of death by infection.
Clinical symptoms of pulmonary insufficiency occur less frequently than the histological changes because RA imposes limitations that make physical exertion difficult, thus respiratory involvement may be asymptomatic. However, the mortality rate from pulmonary disease in RA is twice that of the general population.2
Pulmonary Function Tests (PFTS) are widely used to provide objective measure of Lung function for detecting and quantifying pulmonary impairment in cardio-pulmonary diseases and monitoring response to therapy, monitoring the effect of environmental, occupational and drug exposures-associated with Lung diseases.
After arterial blood gas measurement, the most common test of gas transfer across the Lung is the carbon monoxide diffusing capacity (DLCO) also called transfer factor (TLCO) which measures the rate of transfer of carbon monoxide (CO) from the Lung to the blood.10
METHODS
This was across sectional study carried out at the unit of Rheumatology in Baghdad teaching hospital from October 2002 until March 2003. The sample consisted of 40 Iraqi patients (35 females and 5 males) with active Rheumatoid Arthritis as defined by the American Rheumatism Association ARA 1987 for the classification of RA.11 Informed consent had been obtained from the patients. All the patients were life long non smoker’s and with no evidence of respiratory diseases nor did they show any signs and symptoms (Cough, dyspnes, chest, pain, sputum production, cyanosis, oedema and clubbing) attributed to respiratory diseases.
The patients had no evidence of dry eyes or mouth, had no history of chest injury or exposure to radiation and had no chest infections three months prior to participating in the study. Assessment of disease activity was achieved by clinical and laboratory tests as well as pulmonary function tests; all of which were performed on the same day.
Step I
Clinical assessment was performed by weighted and selective index for activity of synovitis which depends on the degree of tenderness and swelling with weighted factor related to the joints’ surface area, (table 1 and 2) as this index- produces an excellent estimate of total joint inflammation, and is more sensitive in detecting changes in disease activity than any of the other indices.6,7,8
The duration of morning stiffness and the presence of Rheumatoid nodules were reported. The patients’ assessment for classification of functional status were recorded (disability), (table 3) as well as information about treatment was obtained including the type of medication taken [Non steroidal Anti inflammatory drugs (NSAID), Corticosteroids and disease-modifying Anti Rheumatic Drugs (DMARD)] and duration and regularity of intake were also noted.2
Table 1: Weighted and Selective Index for Activity of Synovitis
Joint |
Weighted factor (related to joint surface area) |
Degree of tenderness and swelling (scale 0 to 3) |
Joint score |
|
Elbow |
|
|
|
|
|
R |
48 |
- |
- |
|
L |
48 |
- |
- |
Wrist |
|
|
|
|
|
R |
32 |
- |
- |
|
L |
32 |
- |
- |
MCP (Separately) |
|
|
|
|
|
R |
|
- |
- |
|
L |
|
- |
- |
PIP (Separately) |
|
|
|
|
|
R |
5 |
- |
- |
|
L |
5 |
- |
- |
Knee |
|
|
|
|
|
R |
95 |
- |
- |
|
L |
95 |
- |
- |
Ankle (Mortice) |
|
|
|
|
|
R |
32 |
- |
- |
|
L |
32 |
- |
- |
First MTP |
|
|
|
|
|
R |
8 |
- |
- |
|
L |
8 |
- |
- |
Second to fifth |
|
|
|
|
MTP separately |
|
|
|
|
|
R |
5 |
- |
- |
|
L |
5 |
- |
- |
R: Right; L: Left; MCP: Metacarpophalangeal joint PIP: Paroximal Interphalangeal MTP: Metatarsophalangeal joint |
||||
Table 2: Method of Scoring the Severing of Tenderness and Swelling of each Joint examined
Score |
Tenderness |
Soft tissues swelling |
0 |
Not tender |
None |
1 |
Tender |
Probable swelling |
2 |
Tender, with wince |
Definite swelling |
3 |
Tender, with wince and withdraw response |
Tense swelling |
Table 3: Criteria for Classification of Functional Status in Rheumatoid Arthritis
Class |
Functional Status in Rheumatoid Arthritis |
Class I : |
Completely able to perform usual activities of daily living (self-care, vocational, and avocational). |
Class II: |
Able to perform usual self-care and vocational activities, but limited in avocational activities. |
Class III: |
Able to perform usual self-care activities, but limited in vocational and avocational activities. |
Class IV: |
Limited in ability to perform usual self-care, vocational, and avocational activities. |
Usually self-care activities include dressing, feeding, bathing, grooming, and toileting, while vocational activities are patient-desired and are often age and sex-specific.2 They can include recreational and/or leisure activities at work, school, or domestic activities
Step II
Laboratory assessment was performed by assessing the Erythrocyte sedimentation Rate (ESR), hemoglobin concentration (Hb%) and latex agglutination tests which took place at the teaching laboratories of Baghdad medical city.
Step III
Pulmonary function tests were performed at the pulmonary function unit at Baghdad teaching hospital by a senior technician.
Spirometry Parametesr Include
The Forced Vital Capacity (FVC) test which was performed by having the patients inhale a Total Lung Capacity (TLC), then take maximum forced exhalation into a Spirometer. Traditionally, exhaled volume is measured as a function to indicate flow, but it can also be measured to illustrate the function of exhaled volume.
Forced Expiratory Volume in one second (FEV1) is the volume of air expelled in the first second of a forced expiration starting from full inspiration, which is measured in liters.
The three primary spirometic indices in the forced test are FVC, FEV1 and their Ratio FEV1/FVC.
A minimum of the three vital capacity and forced expiratory volume determinations were performed and the two best values within 5% of each other were averaged. Spirometric measurements were considered abnormal when more than two residual Standard Deviates (SD) below the predicted value.
In terms of diagnosis, spirometry is used only to classify patients as having normal air flow or having obstructive or restrictive Lung disease.
The diffusing capacity for carbon monoxide (DLCO) was measured using a single breathing technique, which was performed as follows: The patient exhales to residual volume, a valve is open and the patient then inhales to full vital capacity. The test gas, which in addition to nitrogen contains 0.3% carbon monoxide an inert insoluble tracer gas Helium and 18-21% Oxygen. The patient relaxes into a breath-hold at total Lung capacity for 10 seconds and then exhales rapidly.10
The diffusing capacity for carbon monoxide corrected for hemoglobin and is considered abnormal when the value is more than two Standard Deviations (SD) below or above the predicted value.
A randomly selected sample group of 30 (27 females and 3 males) patients with inactive Rheumatoid arthritis matching for age and gender, served as a control group.
Statistical analysis of the data collected was performed using statistical packages for social science version 10.1 (Spss version 10.1).
The data was presented in simple measures of frequency, percentage, mean and SD.
The data was statistically analysed using the following tests:
1. Students- t test for the comparison of two means of quantitative data.
2. Chi. Square test (X2) for the comparison of qualitative data. p value of <0.005 was used as level of statistical significance.
RESULTS
The study included 40 (35 female and 5 males) patients with active Rheumatoid Arthritis. The mean age was 37.5 ± 9.5 years (Ranging from 22-58 years). The mean disease duration was 6.6 ± 4.6 years (ranging beween from 2-19 years). The demographical characteristics of the study patients with active RA are shown in table 4.
Table 4: Demographical Characteristic of Patients with active RA
Patients |
Female |
Male |
Total number of patients 40 |
35 |
5 |
|
87.5% |
12.5% |
Mean (range age in years) 37.5 (22-58) |
37.8 |
35.2 |
|
(22-55) |
(22-58) |
Mean (range) disease duration in years 6.6 (2-19) |
6.8 |
5 |
|
(2-16) |
(2-8) |
Ratio: Female: male = 7:1
The parameters of disease activity are shown in table 5.
Table 5: Parameters of Disease activity
Laboratory Test |
Range |
Mean |
SD |
Hb level (g/dl) |
7-13.3 |
10.28 |
1.82 |
ESR level (mm/h) |
11-131 |
53.77 |
27.53 |
Ar. Index |
307-604 |
446 |
80.88 |
Hb: Hemoglobin; ESR: Erythrocyte Sedimentation Rate; Ar: Aortic regurgitation; SD Standard Deviation |
|||
All the study patients tested postitive for the presence of Rheumatoid factors. All the patients were found to belong to either class III or IV of the functional classification. All the study patients experienced morning stiffness lasting more than one hour. None of the patients in either the study group or the control group were smokers.
Pulmonary function test abnormalities showed restrictive ventilator defect in 15 (37.5%) patients and obstructive ventilator defect in 10 (25%) patients.
The tests also showed decreased diffusing Lung capacity for carbon monoxide (DLCO) in 23 (57.5%) patients.
Tables 6: Results of Pulmonary Function in Patients.
Function Test |
Range |
Mean |
SD |
FEV1/Lit |
1.01-4.83 |
2.21 |
0.88 |
FEV1/FVC |
28-219 |
78.55 |
30.43 |
FVC/lit |
1.12-4.40 |
2.67 |
0.76 |
DLCO (mmol/min/kpa) |
5.01-11.61 |
7.12 |
1.60 |
FEV1: Forced Expiratory Volume; FVC: Forced Vital Capacity; DLCO: Diffusing Capacity of the Lung for Carbon Monoxide; SD: Standard Deviation |
|||
All the patients received treatment of non steroidal anti-inflammatory drugs, Corticosteroid and disease modifying anti Rheumatoid drugs.
The results of pulmonary function tests in the study group and control group are show in figure 1.
Table 7: Case –Control Comparison of PFTS defects in RA
PFTs Defect |
Case |
Control |
|
N=40 No. (%) |
N=30 No. (%) |
Restrictive |
|
|
Ventilator defect |
15 (37.5) |
2 (6.6) |
Obstructive |
|
|
Ventatory defect |
10 (25) |
1 (3.3) |
Decrease DLCO |
23 (57.5) |
2 (6.6) |
PFTS: Pulmonary Function Tests; DLCO: Diffusing Capacity of the Lung for Carbon Monoxide |
||
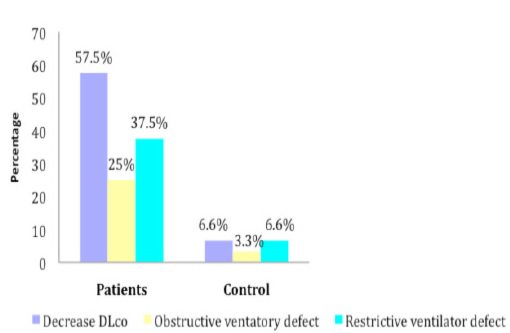
Figure 1: Bar chart show case-control difference in PFT abnomalities
DISCUSSION
Spirometry is the most common and most useful lung function test. It has extensive clinical implications. It is the least expensive test to perform and it should be the test most widely available at doctors’ offices, clinics and hospitals.
The reduction in diffusing lung capacity of carbon monoxide reported acted as an early indicator for the presence of both emphysema and interstial fibrosis.10
A case report by Kawamura et al reported an incident of Rheumoatoid Lung disease in which lung involvement preceded arthritis.12
This study was limited to patients with confirmed RA defined by ARA criteria with active disease, and all the patients in the study were free from respiratory signs and symptoms. Lung function tests are different from other medical tests in that many of them require patients to participate actively and vigorously. Since some patients would have been unable to perform the tests, the age of the study patients was limited to no more than 58 years old. It is widely accepted that RA is one of many chronic inflammatory diseases which is predominant in women, this was also reflected in this study where the female to male ratio was 7:1. This finding probably reflects the out patient population.
From analyzing the data obtained from disease activity parameters and pulmonary function tests in this cross sectional study of 40 active rheumatiod Iraqi patients (35 female and 5 males), the results demonstrated a definite correlation between FEV1 and FEV1/FVC with Hb% (P=0.0001) and an inverse relationship observed with ESR level and articular index and disease duration(P=0.0001).
There was also a clear correlation between FVC and Hb% (0.0001) and an inverse relation with ESR level, articular index and disease duration (P=0.0001). Additionally DLco correlation with Hb% and inversely with ESR level, articular index and disease duration (P=0.0001). When comparing this study to a study by Saravanan et al,13 which demonstrated clear correlation between FEF1 and Hb% (P~0.01) and borderline inverse relationship between FEF1 and ESR (P=0.05). Additionally DLco correlated with both Hb% (P=0.03) and ESR (P=0.01).
A study by Pelucchi-A et al, confirmed that Lung function and DLCO in patients with juvenile arthritis are related to the clinical sub types of the disease and the disease activity.14 The exact mechanism for the development of air way obstruction in RA is unknown, however, it is possible that the mucosal edema secondary to pre-existing air way inflammation may lead to bronchial narrowing and hence cause air way obstruction.15
The measurement of respiratory volumes and capacities is an essential tool for determining how well the lung is functioning.16 The decreased DLCO measurement was indicative of the pathology of pulmonary diseases such as reduced lung surface area in Emphysema, altered structural component of alveolar-capillary membrane as is characteristic of Pulmonary Fibrosis, obstructed or obliterated pulmonary capillaries observed in Pulmonary Embolism.10
Vergnenègre et al recently reported a significant relationship between Forced Expiratory Flow (FEF 25-75), duration of articular disease, FEV1/FVC and Ritchie index, and also a parallel evolution of pulmonary exacerbation and flares of articular disease in some patients.17,18 The health assessment questionnaire (HAQ), disability index (DI) was also an important risk factor for the decline in both DLCO and FVC.19
All the study patients were positive for Rheumatoid factors, which suggests that there may be a significant positive correlation between the presence of Rheumatiod Factor (RF) and abnormal PFTS which correlate with other studies.20
Furthermore, a study by Donagh et al. reported that pulmonary function was often impaired in a pattern similar to that of advanced interstitial Lung disease.21 While a study by Cannon et al, reported that Disease modifying anti Rheumatic drugs were observed to cause interstitial Lung disease.22
CONCLUSIONS
1. Pulmonary function tests can be used as indicators of disease activity in Rheumatoid Arthritis.
2. Lung function data can be used to stratify abnormalities in a clinically useful manner.
3. Longitudinal studies are needed to ascertain the effect of therapy on these abnormalities.
4. Overall, the results from this study demonstrated that the high incidence of pulmonary dysfunction observed in the study patients was unexpected and suggests that all patients with RA should undergo PFTS for complete assessment.
ACKNOWLEDGMENTS
The authors reported no conflict of interest and no funding has been received on this work.
-
Maini RN, Feldmann M. Rheumatoid Arthritis in: Maddison pj, lesnberg DA, Woo p, Glass DN (Eds). Oxford Textbook of Rheumatology. 2nd ed. Vol 2 Oxford, New York, Tokyo: Oxford University Press, 1998; 983-1031.
-
Goronzy J, Weyand CM. Rheumatoid arthritis In: Klippel JH, Crofford LJ, Stone JH, Weyand CM (Eds). Primer on the Rheumatic Disease, 12th ed. Atlanta, Georgia. Arthritis foundation. 2001; 209-232.
-
Nuki G, Ralston SH, Luqmani R. Disease of the connective tissues, joints and bones in: Haslett C, Chilvers ER, Hunter JA, Boon NA (Eds). Davidson’s principle and practice of medicine, 18th ed. London: Churchill Livingstone 1999; 801-875.
-
AL- Rawi ZS, AL-Azzawi AJ, AL-Ajili FM, AL-Wakil R. RA in population samples in Iraq. Ann Rheum Dis 1978; 73-75.
-
Thompson PW, Silman AJ, Kirwan JR, Currey HLF. Articular indices of joint inflammation in Rheumatoid Arthritis, correlation with the Acute-phase Response. Arthritis and Rheumatism vol. 30 No. 6 1987; 618-623.
-
Stuki G, Stucki S, Bruhlmann P, Maus S, Michel BA. Comparism of the validity and reliability of self – reported articular indices. Br J Rheumatol 1995; 34:760-766.
-
Van den Bink HR, van der Heide A, Jacobs JW, van der Veen MJ, Biilsma JW. Evaluation of the Thompson articular index. J Rheumatol 1993; 20:28-32.
-
Harris ED, Clinical features of rheumatoid arthritis. In: Kelly Wn, Ruddy S, Harris ED, Sledyne CB (Eds). Textbook of rheumatology, 5th ed. Philadelphia: WB Saunders Co. 19997; 898-968.
-
David M lee, Michael L. Weinblatt Rheumatoid Arthritis. The Lancet Vol 358. 2001; 903-909.
-
Baum GL, Crapo JD, Celli BR, Karlinsky J. Pulmonary function testing textbook of pulmonary disease 6th ed. 1998; 199-217.
-
Arnett FC, Edworthy SM, Bloch AD, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Associational 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988; 31:315-324.
-
Kawamura T, Mochizuki Y, Nakahara Y, Watanabe S, Sasaki S, Kobashi Y. A case of rheumatoid lung disease in which Lung involvement preceded arthritis. Nihon-kokyuki- Gakkai-Zashi, 2001; 39:131-14 (Medline).
-
V. Saravanan Laura Jones, Kelly CA. Correlation between disease activity and Lung function in patients with RA. Annuls of the Rheumatic disease July, 2000 Vol 59 Supp I.
-
Pelucchi A, Lomater C, Gerloni V, Foresi A, Fantini F, Marazzini L. Lung function and diffusing capacity for carbon monoxide in patients with juvenile chronic arthritis: effect of disease activity and low dose methotrexate therapy. Clin- Exp-Rheumatol. 1994; 12:675-679.
-
Hassan Wu, Keaney NP, Holland CD, Kelly CA. Bronchial reactivity and air flow obstruction in RA. Ann. Rheum Dis 1994; 3:511-514.
-
Tortroa GJ, Anagnostakos NP. Principles of anatomy and physiology Harper international Edition 4th ed 1984. The respiratory system, Ch 23:560.
-
Vergnenègre A, Pugnère N, Antonini MT, Arnaud M, Melloni B, Treves R, et al. Air way obstruction and rheumatoid arthritis, Eur. Respir. J. 1997: 10:1072-1078.
-
Bach, F 1948 Penicillin for the rheumatoid type of arthritis Ann. Rheum. Dis. 7:25-28.
-
Saag KG, Kolluri S, Koehnke RK, Georgou TA, Rachow JW, Hunninghake GW, et al. Rheumatoid arthritis lung disease determinants of radiographic and physiologic abnormalities. Arthritis – Rheum. 1996; 39:1711-1719.
-
Lawrence JS, Locke GB, Ball J. rheumatoid serum factor in population in the UK. Lung disease and rheumatoid serum factor clin. Exp Immunol, 1971; 8:723-739.
-
McDonagh J, Greaves M, Wright AR, Heycock C, Owen JP, Kelly C. High resolution computerized tomography of the lung in patients with RA and interstitial lung disease. Br. J. Rheumatol 1994; 3:118-127.
-
Cannon GW. Pulmonary complication of Ant rheumatic drug therapy. Semin Arthritis Rrheum 1990; 19:353-364.