Laparoscopic Assisted Two Port Open Appendicectomy
Vishwanath Golash
ABSTRACT
Objective: The laparoscopic appendicectomy can be performed using one to several ports. We present our experience of two port laparoscopic assisted open appendicectomy. The objective was to assess the results retrospectively in terms of complications and its limitations.
Methods: Between years 1998-2007, a two port laparoscopic assisted appendectomy was attempted in 2380 adult patients with suspected appendicitis. The patients with localized or generalized peritonitis were included. The appendicectomy was performed via an assisted two port method using 10 mm umbilical optical port and another 10 mm port in right iliac fossa. The children aged 12 and below and pregnant patients were excluded. All patients had their laparoscopic appendicectomy within 48 hours of admission.
Results: Two port laparoscopic assisted appendicectomy was successful in 86.9% of cases. Acute appendicitis was the cause of acute abdomen in 88.9% of the patients. The accessory port was required in 8.5% of patients to complete the appendicectomy and the conversion rate to open was 4.6%. The mean operation time was 25 minutes and the mean hospital stay was 1.5 days. The port site infection was seen in 14, bleeding in 20, parietal wall abscess in three cases and intra-abdominal abscesses in 4 patients.
Conclusion: This approach is simple, can be converted to total intracorporeal by inserting accessory port or to open appendicectomy when required and has advantage of full laparoscopy of abdomen. It has its limitations in cases of extreme obesity, thick mesentery, gangrenous appendix, very large and thick appendix, and difficulty in finding the appendix, control of bleeding, division of adhesions and to deal with other associated pathology. Cost was minimized by using non-disposable port. The overall morbidity was low. There were no specific complications related to this technique and incidence of port site infection was similar to other approaches of laparoscopic appendicectomy.
Keywords: Laparoscopy; Acute abdomen; Appendicitis; Two port.
Submitted: 05 Jan 2008
Reviewed: 18 Feb 2008
Accepted: 08 Apr 2008
From the Department of Surgery, Sultan Qaboos Hospital, Salalah, Governerate of Dhofar, Sultanate of Oman.
Address correspondence and reprint request to: Dr. Vishwanath Golash, Senior Consultant General and
Laparoscopic Surgeon, Head Department of Surgery, Sultan Qaboos Hospital
INTRODUCTION
Laparoscopic appendicectomy is an intracorporeal operation and requires three or more ports, endoloop/staplers for appendicular vessels and appendicular base, or the expertise in intracorporeal ligation. The aim of minimal access surgery is not only to minimize the number of ports but also the cost of surgery. Hence we adopted a laparoscopic assisted open appendicectomy approach using two non-disposable ports to save the cost and had no added morbidity.
Two port assisted open appendicectomy has the advantage of diagnostic laparoscopy and open appendicectomy. It is simple and can be converted to open or intracorporeal approach when required.
Laparoscopic appendicectomy is still not widely practiced and its advantages are not viewed similar to laparoscopic cholecystectomy. Probable limiting factors are the cost of disposable items and the availability of trained staff in odd hours. We adopted the laparoscopic approach irrespective of gender of the patients with suspected appendicitis to insure that no diagnosis is missed.1 The presence of localized or generalized peritonitis was not a contraindication. Acute abdominal pain comprises 40% of all our emergency admission in Oman and acute appendicitis was the cause of acute abdomen in 88% of the patients. The appendicectomy was always attempted via an assisted two port method in all cases as it was technically simple. We have adopted this method since several years. To minimize the cost we have used reusable instruments.
METHODS
This is a retrospective analysis of the 2380 patients who underwent laparoscopic appendicectomy from June 1998 to July 2008. Laparoscopic approach was avoided in patients with multiple previous surgeries, contraindications for general or regional anesthesia and as per the guidelines of local ethical committee in pregnant patients and children (aged 12 and below). Majority of the patients were in younger age group and females due to local demography of the country.1 All patients with suspected appendicitis with or without localized or generalized peritonitis were considered for laparoscopy. A routine work up included the blood count, C-reactive protein, urea, electrolyte, blood sugar, and urine examination. Pregnancy test, chest radiograph, abdominal radiograph, ultrasound and CT scan were performed when clinically indicated. All patients received Metronidazole on induction and penicillin with Gentamycin in peritonitis. Laparoscopy was performed within 48 hours of admission. Laparoscopy was performed with patient lying supine. We routinely establish pneumoperitoneum by open technique. A 0º laparoscope was introduced through 10 mm umbilical port and the diagnosis was established. A second 10 mm port was inserted in right iliac fossa; the table was tilted towards the right side and in Trendelenbourg position. The appendix was held by its mesentery near the tip on a grasper and delivered extracorporeally together with trocar while deflating the abdominal cavity at the same time. The ligation of vascular pedicle and the appendicectomy was done extracorporeally and stump was returned back in the abdomen after touching it with Povidine-Iodine swab and also the port site. A through peritoneal lavage was performed in all cases of peritonitis. When required, the right iliac fossa port was used for inserting the intraabdominal drain. The intracorporeal appendicectomy was done when indicated (Table 1).
Table 1: Indications for accessory ports/intracorporeal Appendicectomy 8.5 %( n=202)
Indication |
Number of Patients |
Short stumpy appendix |
11 |
Very large and thick appendix |
8 |
Thick mesentery |
23 |
Difficulty in finding the appendix |
14 |
Extreme obesity |
27 |
Control of bleeding |
5 |
Division of adhesions |
10 |
To deal with other associated pathology |
104 |
RESULTS
There was no mortality from this procedure. The two port open appendicectomy was successful in 86.9% (n=2068). The accessory ports were required in 8.5% (n=202) of the patients to complete the appendicectomy. A total 4.6% (n=109) were converted to open appendicectomy (Table 2).
Table 2: Indications for Conversion to open 4.6 %( n=109)
Indication |
Number of Patients |
Appendicular mass |
36 |
Perforated/Gangrenous appendix |
43 |
Appendicular abscess |
9 |
Injury to viscera |
3 |
Slipped appendicular artery extracorporeally |
3 |
Slipped appendicular artery intracorporeally Adhesions |
3 |
Cannot find appendix |
7 |
Difficulty in returning the cecum / appendicular stump back in abdomen |
5 |
The localized/generalized peritonitis was present in 15% (n=357) of patients. The incidence of perforated/gangrenous appendix was 9% (n=214), inflamed appendix 69% (n=1642), appendicular mass 7% (n=167), appendicular abscess 3% (n=71), and appendix looked normal laparoscopically in 12% (n=286). The appendix was removed in a bag in 7% (n=166) of the cases. There was no case of appendicular tumor reported in histopatholgy in this series. Abdominal drain was used in 16% (n=381) of patients. The appendicectomy was performed between 4-48 hours of admission. The mean operation time was 25 minutes (range, 10-65). The mean hospital stay was 1.5 days (range, 1-7). Postoperatively, out of six cases of intra-abdominal abscesses, two were treated by ultrasound guided percutaneous drainage, two required laparotomy and other two were drained laparoscopically. There were three visceral injury dealt by conversion to open. The appendicular pedicle slipped in 5 cases while tying it extracorporeally and in 3 cases intracorporeally. Laparotomy was performed in three patients to control the intraperitoneal bleeding from the slipped pedicle 24-48 hours after the surgery. Three patients developed port site hernia in follow up varying from six months to 8 years. Open drainage was performed for one rectus sheath abscess and two parietal wall abscesses.2 Wide debridement was done in one case of necrotizing fasciitis (table 3).
Table 3: Complications (n=48)
Complication |
No. of Patients |
Slipped pedicle |
10 |
Port site bleeding |
7 |
Port site wound infection |
14 |
Port site pain |
11 |
Port site hernia |
2 |
Postoperative Intraabdominal bleeding |
3 |
Injury to viscera |
3 |
Intraabdominal abscess |
4 |
Parietal wall abscess |
2 |
Rectus sheath abscess |
1 |
Necrotizing fasciitis |
1 |
DISCUSSION
The advantages of laparoscopic appendectomy are well proven in several prospective randomized trials and it can be performed using one to several ports.3-10 Each technique has its own merits and demerits. In three ports approach the appendicular artery is ligated or clipped intracorporeally; the appendicular base ligated or endoloop or endoGIA stapler. But since appendicectomy is an emergency procedure in the majority of patients a surgeon with experience of intracorporeal tying may not be available in odd hours. Depending on the surgeon’s choice and experience the use of clipper, endoloop and endo GIA adds in the cost of the operation in this approach.
In a single port approach the operating telescope is introduced through the umbilical port and through the operating channel of the telescope the appendix is grasped and brought out along with the port. This approach may be beneficial in a straight forward early appendicitis, when appendix and its mesentry is not thick or in pediatric age group where the distance between the umbilicus and the appendicular base is small. This technique requires an experienced surgeon in laparoscopy and is difficult to control bleeding, obese patients and deal with other associated pathology. Others have combined the advantages of operating telescope in umbilical with a 5mm suprapubic port but experience is limited.
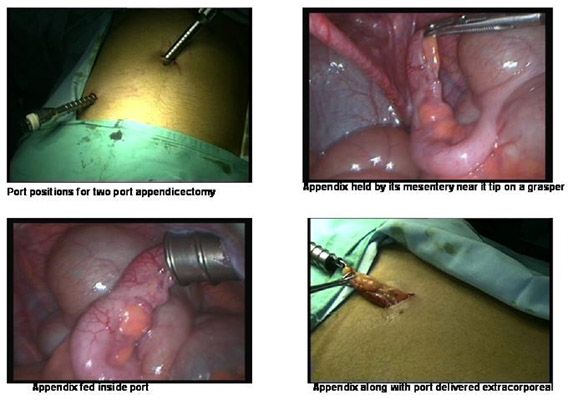
Figure 1: Steps in two port laparoscopic appendicectomy
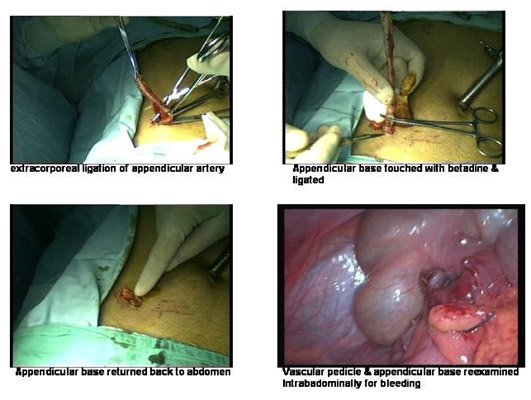
Figure 2: Steps in two port Laparoscopic appendicectomy
On the other hand the two port laparoscopic assisted open apendicectomy is simple, easy to learn and has the combined advantages of open appendicectomy and full laparoscopy of abdomen. It can be converted to open appendicectomy very quickly when required or to total intracorporeal approach by inserting accessory ports. Compared to single port approach does not require expertise of operating telescope. Cost is minimized by using non-disposable port. The overall morbidity is low. There were no specific complication related to this technique and incidence of port site infection was similar to other approaches of laparoscopic appendicectomy. appendicectomy.11 We did not encounter any increased risk of intraperitoneal abscesses and those who had parietal wall abscesses were due to perforated appendix and not per se because of the technique. The percentage of patients having laparoscopic assisted appendicectomy has steadily increased and the conversion rate has decreased in our hospital over the years.12 Although controversial, we routinely removed the normal appendix if no other cause for acute pain was found during laparoscopy.13-19 We believe this is acceptable because the pain from appendicolith, appendicular foreign body, and chronic recurrent aIn a single port approach the operating telescope is introduced through the umbilical port and through the operating channel of the telescope the appendix is grasped and brought out along with the port. This approach may be beneficial in a straight forward early appendicitis, when appendix and its mesentry is not thick or in pediatric age group where the distance between the umbilicus and the appendicular base is small. This technique requires an experienced surgeon in laparoscopy and is difficult to control bleeding, obese patients and deal with other associated pathology. Others have combined the advantages of operating telescope in umbilical with a 5mm suprapubic port but experience is limited.
On the other hand the two port laparoscopic assisted open apendicectomy is simple, easy to learn and has the combined advantages of open appendicectomy and full laparoscopy of abdomen. It can be converted to open appendicectomy very quickly when required or to total intracorporeal approach by inserting accessory ports. Compared to single port approach does not require expertise of operating telescope. Cost is minimized by using non-disposable port. The overall morbidity is low. There were no specific complication related to this technique and incidence of port site infection was similar to other approaches of laparoscopic appendicectomy.oman','serif'; font-size:18.0pt; color:windowtext; ">REFERENCES
REFERENCES
-
Golash V, Willson PD, early laparoscopy as a routine procedure in the management of acute abdominal pain: A review of 1320 patients. Surg Endosc 2005; 19:882-885.
-
Golash V. Rectus sheath abscess after laparoscopic appendicectomy. J Min Access Surg 2008; 3:64-65.
-
Hellberg A, Rudberg C, Kullman E, Enochsson L, Fenyo G, Graffner H, et al. Prospective randomized muliticentre study of laparoscopic versus open appendicectomy. Br. J Surg 1999; 86:48-53.
-
Attwood SE, Hill AD, Murphy PG, Thornton J, Stephens RB. A prospective randomized trial of laparoscopic versus open appendectomy. Surgery 1992; 112:497-501.
-
Anderson DG, Edelman DS, Laparoscopic appendectomy versus open appendectomy: a single institution study. J Soc Laparoendosc Surg 1997; 1:323-324.
-
Konstadoulakis MM, Gomatos IP, Antonakis PT, Manouras A, Albanopoulos K, Nikiteas N, et al. Two trocar laparoscopic assisted appendectomy versus conventional laparoscopic appendectomy in patients with acute appendicitis. J Laparoendosc Adv Surg Tech A. 2006; 16:27-32.
-
Fazili FM, Al-Bouq Y, El-Hassan OM, Gaffar HF. Laparoscopic–assisted appendicectomy in adults: the two trocar technique. Ann Saudi Med. 2006; 26:100-104.
-
Suttie SA, Seth S, Driver CP, Mahomed AA. Outcome after intra-and extra-corporeal laparoscopic appendectomy techniques. Surg Endosc. 2004; 18:1123-1125.
-
Nguyen NT, Zainabadi K, Mavandadi S, Paya M, Stevens CM, Root J, et al. Trends in utilization and outcomes of laparoscopic versus open appendectomy. Am J Surg. 2004; 188:813-820.
-
Ahmet Tekin H. Cemal Kurtoğlu. Video-Assisted Extracorporeal Appendectomy Journal of Laparoendoscopic & Advanced Surgical Techniques. 2002; 12:57-60.
-
Sezai Demirbas, Vedat Atay, Arman Api, Cengiz Erenoglu, Mehmet Yildiz: Laparoscopic appendicectomy Enables Military Personnel Return To Work Early. The Internet Journal of Surgery. 2007. Volume 9 Number 2.
-
Khan AR. Two port laparoscopic assisted appendectomy in a child with use of the ultrasonically activated endo-shear. Pediatric Endosc & Inovative techniques 2003; 7:193-197.
-
Oak SN, Parelkar SV, Akhtar T, Joshi M, Pathak R, Viswanath N, et al. Minimal access surgery in children-5 years institutional experience. J Min Access Surg 2005; 1:121-128.
-
Chiarugi M, Buccianti P, Decanini L, Balestri R, Lorenzetti L, Franceschi M, ey al. “What you see is not what you get”. A plea to remove a ‘normal’ appendix during diagnostic laparoscopy. Acta Chir Belg. 2001; 101:243-245.
-
Nemeth L, Reen DJ, O’Briain DS, McDermott M, Puri P. Evidence of an inflammatory pathologic condition in “normal” appendices following emergency appendectomy. Arch Pathol Lab Med. 2001; 125:759-764.
-
Bouchard S, Russo P, Radu AP, Adzick NS. Expression of neuropeptides in normal and abnormal appendices. J Pediatr Surg. 2001; 36:1222-1226.
-
Barber MD, McLaren J, Rainey JB. Recurrent appendicitis. Br J Surg. 1997; 84:110-112.
-
Grunewald B, Keating J. Should the ‘normal’ appendix be removed at operation for appendicitis? J R Coll Surg Edinb. 1993; 38:158-160.
-
Reyad Al-Ghnaniem, Hemant M. Kocher, Ameet G. Patel. Prediction of inflammation of the appendix at open and laparoscopic appendicectomy: findings and consequences. The European Journal of Surgery 2002; 168:4-7.