Off-Pump Coronary Artery Bypass Grafting Through Left Antero-Lateral Thoracotomy (Thora-Cab) – Case Report and Review of Literature
Hilal Al-Sabti, Paresh Kumar Kuba, Suresh Chengode, Ashok Kumar Sharma
ABSTRACT
We report the first case of off-pump complete myocardial revascularization through antero-lateral thoracotomy (Thora-CAB) in Middle-East. 69 year old gentleman having angina pectoris for last three years with severe double vessel disease involving the left anterior descending artery (95% proximal lesion) and the circumflex system (80% mid circumflex lesion with significant osteal disease in obtuse marginal) and insignificant disease in right coronary artery with moderate left ventricular impairment underwent Thora-CAB. Post-operatively, he had minimal pain, quick symptomatic improvement and no complications. He was discharged home on 5th post-operative day. This indicates that the thoracotomy approach is safe and practical for CABG. It is well tolerated hemodynamically with no/ minimal post-operative morbidity.
Keywords: Anterolateral thoracotomy; Coronary artery bypass grafting; Thoracab.
Submitted: 02 Aug 2008
Reviewed: 19 Aug 2008
Accepted: 09 Sept 2008
From the Cardiothoracic Surgery Unit, Sultan Qaboos University Hospital, P.O. Box 35, Al-Khod, Post Code 123, Muscat, Sultanate of Oman.
Address correspondence and reprint requests to: Dr Ashok Kumar Sharma, Cardiothoracic Surgery Unit, Sultan Qaboos University Hospital, P.O. Box 35, Al-Khod, Post Code – 123, Muscat, Sultanate of Oman.
Email: drashoksharma1@gmail.com
There are very few studies in literature, which have reported complete primary revascularization of the coronary arteries via a thoracotomy incision. Conventional coronary bypass surgery is associated with substantial morbidity with or without cardiopulmonary bypass (CPB) and median sternotomy. This report describes an innovative technique to perform complete revascularization through a lateral thoracotomy without CPB (thoraCAB).
A 69 year old euglycemic, normotensive gentleman with stable angina for last three years was referred from The Royal Hospital, Oman. The symptoms had gradually worsened over time. He underwent a coronary angiogram which showed severe double vessel disease involving the left anterior descending artery (95% proximal lesion) and the circumflex system (80% mid circumflex lesion with significant osteal disease in obtuse marginal) and insignificant disease in right coronary artery with moderate left ventricular dilatation, hypokinesia of inferobasal and diaphragmatic segment and moderate impairment of left ventricular function (EF = 35%)
After a detailed discussion with the patient and relatives about the different management options and due explanation of risks and benefits of surgery including conventional and thoracotomy CABG, he underwent off-pump coronary artery bypass grafting through left anterolateral thoracotomy.
Operative Details
Anaesthetic Considerations
Patient had premedication with Tab. Lorazepam 2mg on the morning of surgery. Invasive and non-invasive monitoring modalities as applicable to routine conduct of anaesthesia for coronary artery bypass grafting were employed. After intravenous induction of anaesthesia with Midazolam 5mg. Fentanyl 500 micrograms and Sevoflurane, trachea was intubated with a 9.0 size single lumen endotracheal tube (SLETT). Left lung isolation, which is mandatory for the left anterolateral approach, was achieved with a Cohen endobronchial blocker. The blocker was guided and properly positioned in the left main bronchus with the help of a 2.8 mm OD fibreoptic bronchoscope by manipulating the inbuilt tip control mechanism on the bronchial blocker. Anaesthesia was maintained with inhaled Sevoflurane through air- oxygen mixture and Fentanyl and Cis-Atracurium infusion. Left lung was collapsed just before the intercostal muscles were cut.
Reexpansion of the lung was done only after the pericostal sutures were taken. The skin of 5th intercostal space was infiltrated with 0.125% Sensorcaine before incision. Patient required 5-micrograms/ kg/min of Dopamine infusion to support the heart during the procedure, which was discontinued on completion of graft placements. An inter pleural catheter was placed before the chest was closed and post operative analgesia was maintained with an infusion of a mixture of Fentanyl 0.5 micrograms/ml and Sensorcaine 0.0625% at 10 ml / hr. Patients trachea was extubated with in 2 hours into the post surgical ICU. Haemodynamics remained stable throughout the postoperative period with negligible pain and was shifted out of the ICU with in 48 hrs.
Position
Supine with slight right lateral tilt using 15o wedge below left shoulder blade
Surgical Procedure
Under single lung ventilation and the patient positioned at 15o to the horizontal the thoracotomy was performed through the left 5th intercostal space, starting medial to the left nipple and extending to the anterior axillary line. Using a Finochetto retractor, the left internal mammary artery, which is visualized very well through this approach, was harvested under direct vision right from its origin down to its bifurcation into the musculophrenic and superior epigastric artery, using harmonic scalpel. Patient was heparinized using 3mg/kg Heparin and the activated clotting time was maintained at more than 350seconds. The activated clotting time was repeated at 20-minute intervals to ensure this.
The internal mammary artery was divided next and a small clip applied at its end. This was followed by a generous ante-phrenic pericardiotomy, from the apex of the left ventricle to the ascending aorta. Pericardial stay sutures were placed on both edges of the incision. Pulling on the traction sutures and securing it onto the retractor, helped bring the ascending aorta and even the right atrial appendage into full view. This was especially helpful while doing the proximal anastomoses (Figure 1).
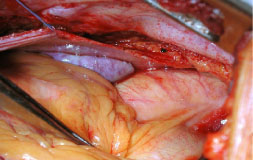
Figure 1: Exposure of the Ascending Aorta and the Right Atrial Appendage.
Aorta was found to be too much on right side and was partially clamped using side-biting clamp. Two pieces of saphenous vein of adequate length were anastomosed to the ascending aorta using 6-0 prolene. The proximal anastomoses of the vein to the ascending aorta preceded the distals, since it gave a better lie to the venous grafts. Extreme caution must be exercised while applying side biting clamps on the aorta. The mean systemic blood pressure was kept low, with systolic blood pressures maintained between 70 to 90 mm Hg. For improved exposure of the lateral and inferior territories, the stay sutures on the left pericardial edge were put under traction.
Without the use of cardio-pulmonary bypass, using myocardial stabilizer, distal anastomosis of Left Internal mammary artery was done to the left anterior descending artery using 7-0 proline and the two pieces of saphenous veins were anastomosed to first and second obtuse marginal arteries using 7-0 proline ( Figure2). The second obtuse marginal artery was small in size. Placing the patients in deep Trendelenburg position helped to maintain hemodynamic stability whilst grafting the circumflex system.
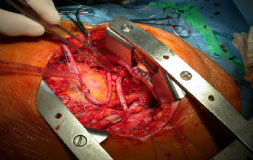
Figure 2: Internal Mammary Artery Anastomosis and the Proximal Anastomosis
Electrocardiogram (ECG) and hemodynamic parameters were continuously monitored throughout the procedure. Heparin effect was reversed with protamine at the end of the procedure, and the thoracotomy closed over a single basal drain after ensuring thorough haemostasis. Intrapleural catheter was placed for regular analgesia
Post-operative Period
Patient was shifted to the intensive care unit on minimal doses of dopamine and noradrenaline. Since, the patient remained hemodynamically stable with minimal drainage from the chest drain, he was extubated within two hours of the surgery and the inotropes were gradually weaned over few hours. The patient was mobilized and was shifted to the ward on second post-operative day after removal of chest drains and all lines. Pain control was adequate with continuous infusion of bupivacaine with fentanyl through the intra-pleural catheter at the rate of 10ml/hour and oral paracetamol as and when required. There were no post-operative complications and the patient was discharged home on 5th post-operative day.
DISCUSSION
Coronary artery bypass grafting with cardiopulmonary bypass is a well-established and effective method of myocardial revascularization.1,2 However, despite advances in perfusion, anesthesia, and surgical techniques, Cardiopulmonary bypass is still associated with a systemic inflammatory response that may lead to postoperative morbidity, such as bleeding, fluid retention, arrhythmias, and temporary organ dysfunction.1-3 Coronary revascularization on the beating heart was first proposed by Benetti and colleagues,4 and Buffolo and coworkers,5 for its potential benefits of maintaining the function of major organs. In 1996, there was a revival of interest in off-pump through various means of minimal incisions, like left anterior small thoracotomy and inferior median sternotomy.4-9 these techniques were only applicable in the majority of cases to single-vessel revascularization. It was soon realized that the natural evolution of the technique to achieve complete coronary revascularization was by performing grafts on the beating heart through a median sternotomy.
Several retrospective as well as prospective randomized studies have provided evidence for reduced morbidity associated with off-pump surgery when compared with conventional on-pump cardiopulmonary bypass.2,3,10-12 In particular there is evidence of reduction of chest infection, inotropic requirement, incidence of arrhytmias, blood loss and consequent requirement for blood transfusion, intubation, and intensive care unit and hospital length of stay. The left anterolateral thoracotomy approach was chosen because potentially it offered all of the benefits of off-pump coronary revascularization, while at the same time avoiding the morbidity associated with median sternotomy. The results of studies on this approach are encouraging. It is possible to perform complete revascularization in the majority of patients.13
From the anaesthetic point, isolation of the lung is better tolerated using a bronchial blocker than a double lumen tube (DLT). This obviates the need of exchanging the DLT with a SLETT at the end of the procedure and the stress of intubation and extubation with a DLT is higher than a SLETT, which is of paramount concern in patients with coronary artery disease.
Thoracic approach for coronary artery bypass grafting has traditionally been advocated for reoperations. There is usually a patent and functioning Internal Mammary artery graft lying anteriorly on the heart and supplying the important left anterior descending territory, with blocked venous grafts to the lateral and/or the inferior areas. In such situations approaching the heart through the traditional sternotomy approach could endanger the patent mammary graft. Some surgeons thus prefer revascularizing the lateral and inferior territories through a thoracotomy incision. Another situation where one would consider a thoracic approach is while doing minimally invasive coronary artery bypass wherein single grafts especially to the LAD territory is done through a small 2-3 inch incision.14 The other indications are as explained below:
Indications for Off-Pump CABG by Thoracotomy
1. Risky Sternotomy due to:
a. Bypass graft(s) at risk
b. Cardiac structure adherent to sternum
c. Previous sternal wound infection
d. Mediastinal radiation therapy
2. Cardiopulmonary bypass undesirable:
a. Calcified ascending aorta
b. Diffuse atherosclerosis
c. Multiple comorbidities
3. Blood conservation
There are also certain proven advantages of coronary revascularization by thoracotomy approach which include very low incidence of hemodynamic instability(possibly because of less manipulation of the heart during positioning), post-operative atrial fibrillation,7,13 minimal pain, faster convalescence, reduced requirements of blood transfusion. Another significant advantage of this approach is the avoidance of mediastinitis and sternal dehiscence, one of the most devastating complications of cardiac surgery.14 Moreover, the access and exposure is much better as compared to median sternotomy, especially for the circumflex system. In a rare event that the patient may require to be taken on cardiopulmonary bypass due to hemodynamic instability, it can be easily done by aortic and atrio-caval cannulation through the same approach or through the femoro-femoral route.
There have been very few studies on this relatively new technique of coronary artery bypass grafting through the anterior thoracotomy approach. The most significant ones include the study by Srivastava Sudhir P. et.al. from Texas,7 Maximo Guida et.al. from Venezuela,13 and Japadman Bhaskar &Sharma A.K.14 from New Zealand. All of them have reported good results with this technique as detailed below. Srivastava Sudhir P. et.al. have reported their experience with 200 cases from February 2000 to April 2001 with complete revascularisation through this approach using an average of 2.9 grafts per patient and have reported a mortality of 0.5% only. Only two patients required a conversion to cardiopulmonary bypass and three (1.5%) required ventilation beyond 48hours, with no strokes throughout the study period.
Maximo Guida et.al.13 have reported a series of 255 patients from November 2002 to July 2005. Complete revascularization was achieved in all patients using 3.3 + 1.0 grafts. There were no conversions to cardiopulmonary bypass, and 3 patients died (1.2%). 237 patients (93.3%) were extubated in the operating room, and 164 patients (65.1%) were discharged home within 48 hours after surgery. Only two patients (0.8%) experienced a stroke. There were 14 patients (5.5%) who experienced postoperative atrial fibrillation.
Jayapadaman Bhaskar and Sharma A.K.14 have reported early results using this technique of anterior thoracotomy. They have reported 27 cases where complete revascularization was achieved through this approach using an average of 2.40 grafts. The blood loss during the first 6 hours was 380 ± 169 ml. None of the patients needed emergency conversion to cardiopulmonary bypass / sternotomy. Post operatively 4 patients had on table extubation.1 patient was re-explored due to bleeding from the thoracotomy. There was no peri-operative Myocardial infarction and the mortality was nil. The average hospital stay was 6.4 ±1 days.
CONCLUSION
Coronary revascularization on the beating heart through anterolateral thoracotomy is a relatively new technique of coronary artery bypass grafting. It is a form of Minimally Invasive Direct Coronary Artery Bypass Grafting (MIDCAB) and is a step forward towards totally endoscopic coronary artery bypass grafting and robotic CABG. There are very few studies conducted in this field and have so far yielded satisfactory results, although long term results are still awaited.
-
Edmunds LH Jr. Extracorporeal Perfusion in Cardiac Surgery in the Adult. In Edmunds LH Jr, Ed. Cardiac Surgery in the Adult. McGraw-Hill, New York 1997:255-294.
-
Ascione R, Angelini GD. Off-pump Coronary Artery Bypass Surgery: The Implications of the Evidence. J Thorac Cardiovasc Surg 2003; 125:779-781.
-
Calafiore AM, Teodori G, Di Giammarco G, Vitolla G, Maddestra N, Paloscia L, et. al. Multiple Arterial Conduits Without Cardiopulmonary Bypass: Early Angiographic Results. Ann Thorac Surg 1999; 67:450-456.
-
Benetti FJ, Naselli G, Wood M, Geffner L. Direct Myocardial Revascularization without Extracorporeal Circulation. Chest 1991; 100:312-316.
-
Buffolo E, Andrade JCS, Branco JNR, Teles CA, Aguilar LFA, Gomez WJ. Coronary artery Surgery without Cardiopulmonary Bypass. Ann Thorac Surg 1996; 61:63-66.
-
Fonger JD, Doty JR, Sussman MS, Salomon NW. Lateral MIDCAB Grafting via Limited Posterior Thoracotomy. Eur J Cardiothorac Surg 1997; 12:399-404.
-
Srivastava SP, Kirit NP, Skantharaja R, Barrera R, Nanayakkara D, Srivastava V. Off‑pump Complete Revascularization Through a Left Lateral Thoracotomy (ThoraCAB): The First 200 cases. Ann Thorac Surg 2003; 76:46-49.
-
Calafiore AM, Angelini GD. Left Anterior Small Thoracotomy (LAST) for coronary artery revascularisation. Lancet 1996; 347:263-264.
-
Ascione R, Reeves BC, Taylor FC, Seehra HK, Angelini GD. Beating heart against cardioplegic arrest studies (BHACAS 1 and 2): Quality of life at mid-term follow-up in two randomized controlled trials. Eur Heart J 2004; 25:765-770.
-
Van Dijk D, Nierich AP, Jansen EW, Nathoe HM, Suyker JL, Diephuis JC, et al. for the Octopus Study Group. Early outcome after off-pump versus on-pump coronary bypass surgery: Results from a randomized study. Circulation 2001; 104:1761-1766.
-
Puskas JD, Williams WH, Duke PG, Staples JR, Glas KE, Marshall JJ et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: A prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg 2003; 125:797-808.
-
Gulielmos V, Eller M, Thiele S, Dill HM, Jost T, Tugtekin SM, et al. Influence of median sternotomy on the psychosomatic outcome in coronary artery single-vessel bypass grafting. Eur J Cardiothorac Surg 1999; 16:34-38.
-
Máximo C. Guida, Giuseppina Pecora, Álvaro Bacalao et.al. Multivessel Revascularization on the Beating Heart by Anterolateral Left Thoracotomy, Ann Thorac Surg 2006; 81:2142– 2146.
-
Jayapadman Bhaskar, Ashok Kumar Sharma. Off-Pump coronary artery revascularization via left thoracotomy –Early results, Ind J Thorac Cardiovasc Surg2007; 23:236-239.