Congenital Nasal Pyriform Aperture Stenosis:
First Case Report in Oman
Rashid Al Abri,1 Hashim Javad,2 Sudesh Kumar,1 Deepa Bharga,1 RL Koul,2Amna Al Futaisi,2 Dilip Sankla3.
ABSTRACT
Congenital nasal pyriform aperture stenosis (CNPAS) is a recently defined clinical entity that causes airway obstruction in the neonate as a result of narrowing of the nasal pyriform aperture. The pyriform aperture is the narrowest, most anterior portion of the nasal airway, and a slight decrease in its cross sectional area will significantly increase the nasal airway resistance. This entity should be kept in the differential diagnosis of any neonate or infant with signs and symptoms of upper air way obstruction. The CNPAS presents with symptoms of nasal airway obstruction, which are often characterized by episodic apnea and cyclic cynosis.
Key words: Congenital nasal pyriform aperture stenosis; Neonates.
Submitted: 09 Jan 2008
Reviewed: 27 Feb 2008
Accepted: 21 Mar 2008
From the 1Department of Otolaryngology and Head Neck Surgery, 2Department of Pediatrics, 3Departments of Radiology, Sultan Qaboos University Hospital, Al khod, Oman.
Address correspondence and reprint requests to: Dr Rashid Al Abri, Department of Otolaryngology and Head Neck Surgery, Sultan Qaboos University Hospital, P. O. Box 38, Postal Code 123, Al Khod, Muscat, Sultanate of Oman.
E-mail: ralabri@hotmail.comINTRODUCTION
Neonatal nasal obstruction due to congenital nasal pyriform aperture stenosis is very rare and uncommon.1,2,3 The usual clinical presentation is respiratory distress, cyclic cyanosis, apnoeas, and feeding difficulties. A bony overgrowth of the maxillary nasal processes is thought to be responsible for this deformity. The diagnosis is suggested by history and physical examination; however, it should be confirmed radiologically by a CT scan of the nasal cavity. It has been suggested that a pyriform aperture width less than 8 mm in a term infant is diagnostic of CNPAS.2 This anomaly has been reported as an isolated feature or can be associated with craniofacial or central nervous system anomalies. Surgery is indicated in cases of severe respiratory distress, feeding difficulties, and when there is no benefit with conservative methods.1 We are reporting first case in Oman of a female baby diagnosed with CNPAS and was managed in our Sultan Qaboos University Hospital.
CASE REPORT
A full-term female baby, first child of consanguineous parents was born by emergency caesarian section because of fetal distress. The mother had gestational diabetes and was on insulin during the pregnancy. The birth weight was 2.6 kg and the neonate had an appearance, pulse, grimace, activity, respiration (APGAR) score of 2 at 1 minute and five at 5 minutes respectively. She was intubated immediately after delivery and was shifted to Neonatal Intensive Care Unit. The neonate was on ventilator support for two weeks, and was not able to maintain saturation after extubation albiet mask inhalation of oxygen. There were periods of cyanosis and apnea. The neonate had difficulty in breast feeding. After this the possibility of choanal atresia was one of the differential diagnoses. On examination the infant had dysmorphic features like low set ears, small chin, high arched palate and the cry was also very weak. The external nasal pyramid and nasal vestibular opening were normal and there was marked decrease in mist formation on spatula test bilaterally suggesting obstruction. There was marked nasal obstruction and it was not possible to pass nasogastric tube through both nostrils for feeding. All the cranial nerves were normal on examination and there was central hypotonia with preserved deep tendon reflexes. There was no coloboma of eye and the cardiovascular examination was normal. There was no ear anomaly. Deafness and throat examination was normal. The neonate underwent complete pituatary hormonal assay which was found to be normal. Other investigations like chest X-ray, ECG, Echocardiogram and Brain CT were also normal. The CT scan of the Nose and paranasal sinuses revealed narrow anterior nasal inlet and bony overgrowth of maxillary nasal process suggestive of congenital nasal pyriform aperta stenosis ( figure 1and 2).
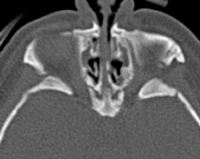
Figure 1: Preoperative CT scan showing narrowing of pyriform aperture.
Figure 2:
Preoperative CT scan at level of floor of nasal
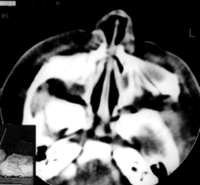
cavity showing narrowing
of pyriform aperture
The patient was taken up for nasal endoscopy and dilatation under general anaesthesia. Initially even the 2.7 mm paediatric endoscope was non negotiable through the nasal pyriform aperture. The nasal cavity was dilated gradually with boogies and then flexible nasal endoscope was passed underneath the inferior turbinate up to the posterior nasal space which revealed bilateral narrow nasal cavity and there was no chaonal artesia. The 3 mm end tracheal tube was passed bilaterally and kept as the stent. After extubation the infant was able to maintain saturation at room air and there was no cyclical cyanosis and apnoeic spells. After 2 weeks both stents were removed and repeat nasal endoscopy was done which showed bilateral adequate nasal cavity. The infant remained comfortable in room air and was able to bottle feed and started to gain weight. The patient is on regular follow up for last 18 months and is doing well.
DISCUSSION
Neonatal nasal obstruction can present at birth as severe birth asphyxia. It is a potentially life-threatening condition unless timely identified and treated and can cause respiratory distress in neonates as they are obligate nasal breathers. Severe bilateral nasal obstruction can lead to apnea, cyanosis, and respiratory distress. The differential diagnosis of neonatal nasal obstruction includes traumatic lesions (sub luxated septum and septal hematoma), cysts (dacryocystocele, dermoid or epidermoid cysts), skull base defects (meningoencephalocele and encephalocele), tumoral processes (glioma, hemangioma, lymphangioma, teratoma, rhabdomyosarcoma), nasal hypoplasia (chondrodysplasia punctata, warfarin teratogenicity), and bony obstruction.4, 5 Unilateral or bilateral bony or fibrous obstruction of the nasal cavity owing to choanal atresia has been recognized as an important cause of congenital neonatal airway obstruction. The choanal atresia can be a part of CHARGE syndrome.6
Congenital nasal pyriform aperture stenosis is a rarer cause of nasal bony obstruction in neonates.2, 3 The nasal pyriform aperture is a pear-shaped bony inlet of the nose formed by the nasal and maxillary bones. The origin and embryological development of CNPAS remains undetermined. The narrowing of the nasal aperture results probably from a bony overgrowth of the maxillary nasal processes during maxillary ossification.2 CNPAS has been described as an isolated anomaly or can be associated with a range of craniofacial and brain anomalies.3, 7, 8, 9 CNPAS is frequently associated with a solitary maxillary central incisor,10 which has been reported as an isolated morphogenic defect or associated with other midline developmental defects such as holoprosencephaly and or pituitary deficiencies.10, 11, 12, 13 Holoprosencephaly has been associated with other clinical features of premaxillary dysgenesis (hypotelorisim and flat nasal bridge) and chromosomal abnormalities (trisomy 13 and 18).3, 7, 9 The presence of associated brain, pituitary and chromosomal anomalies should be excluded by the mean of magnetic resonance imaging, endocrinologic and genetic evaluation.
Neonatal nasal obstruction can present as respiratory distress, cyclic cyanosis, which is relieved by crying and usually associated with sleeping difficulties and feeding problems. By passing a nasal suction catheter the nasal patency can be easily assessed. The etiology and extent of nasal obstruction can be evaluated by an axial CT scan of nose and paranasal sinuses. Each pyriform aperture less than 3mm, or whole pyriform aperture width less than 8mm confirms the diagnosis of CNPAS. Other radiological findings include the presence of a narrowed anterior nasal inlet and bony overgrowth of the maxillary nasal process.12
Early and prompt recognition with appropriate treatment is crucial to avoid the complications of severe respiratory distress. Initially, respiratory distress can be managed using an oral airway or McGovern nipple.2 Nasal patency can be improved with the use of saline solutions or decongestive nasal drops.14 If conservative treatment fails, surgical therapy is indicated. Early surgery (within 10 days) should be performed when the nasal obstruction results in respiratory distress with cyanosis, apnea, or persistent feeding difficulties with inappropriate weight gain.2, 3, 13, 14 Some authors advocate that failure to pass a 5F catheter through the nasal cavity is an indication for surgical repair.8, 14Surgical management of CNPAS includes dilation and stenting or through a sub labial approach to the premaxilla depending upon the extent of stenosis. In our case, nasal obstruction also was relieved by gradual dilatation by boogies and stenting as the nasal bone in neonatal period is soft and can be dialted.15 The narrowed nasal aperture can be enlarged by drilling out the nasal process of the maxilla with diamond burrs and dissection instruments. To allow the nasal mucosa to become attached to the new bony margins and to avoid recurrent stenosis nasal, stents are left in place for at least 7 days or longer.3
 Figure 3: Postoperative CT scan showing patent pyriform aperture. |
CONCLUSION
CNPAS is an unusual case of neonatal nasal obstruction. Early prompt recognition of neonatal nasal obstruction and timely management is necessary to relieve respiratory distress. In all cases of CNPAS, a multidisciplinary approach is required to rule out other craniofacial or midbrain abnormalities.
-
Philippe JP, Wojciechowski M, Koninckx M, Kurotova A, Claes J. Congenital nasal pyriform aperture stenosis: A rare cause of neonatal nasal obstruction. Journal of Pediatric surgery 2006; 41:5-7.
-
Brown OE, Myer III CM, Manning SC. Congenital nasal pyriform aperture stenosis. Laryngoscope 1989; 99:86–91.
-
Van Den Abbeele T, Triglia JM, Francois M, Narcy P. Congenital nasal pyriform aperture stenosis: diagnosis and management of 20 cases. Ann Otol Rhinol Laryngol 2001; 110:70–75.
-
Lowe LH, Booth TN, Joglar JM, Rollins NK. Midface anomalies in children. Radiographics 2000; 20:907–922.
-
Leraillez J. Neonatal nasal obstruction. Arch Pediatr 2001; 8:214–220.
-
Kenman MA. Congenital Disorders of Nose. 16th ed. Nelsons Text Book of Paediatrics, 2000 p. 1258.
-
Arlis H, Ward RF. Congenital nasal pyriform aperture stenosis. Isolated abnormality vs developmental field defect. Arch Otolaryngology Head Neck Surg 1992; 118: 989–991.
-
Hui Y, Friedberg J, Crysdale WS. Congenital nasal pyriform aperture stenosis as a presenting feature of holoprosencephaly. Int J Pediatr Otorhinolaryngol 1995; 31:263–274.
-
Tavin E, Stecker E, Marion R. Nasal pyriform aperture stenosis and the holoprosencephaly spectrum. Int J Pediatr Otorhinolaryngol 1994; 28:199–204.
-
Lo FS, Lee YJ, Lin SP, Shen EY, Huang KJ, Lee KS. Solitary maxillary central incisor and congenital nasal pyriform aperture stenosis. Eur J Pediatr 1998; 157:39–44.
-
Beregszaszi M, Leger J, Garel C, Simon D, Francois M, Hassan M, et al. Nasal pyriform aperture stenosis and absence of the anterior pituitary gland: report of two cases. J Pediatr 1996; 128:858–861.
-
Belden CJ, Mancuso AA, Schmalfuss IM. CT features of congenital nasal piriform aperture stenosis: initial experience. Radiology 1999; 213:495–501.
-
Lee KS, Yang CC, Huang JK, Chen YC, Chang KC. Congenital pyriform aperture stenosis: surgery and evaluation with three-dimensional computed tomography. Laryngoscope 2002; 112:918–921.
-
Lee JJ, Bent JP, Ward RF. Congenital nasal pyriform aperture stenosis: non-surgical management and long-term analysis. Int J Pediatr Otorhinolaryngol 2001; 60:167–171.
-
Raghvan U, Fuad F, Gibbin KP. Congenital midnasal stenosis in an infant. Int J Pediatr Otorhinolaryngol 2004; 68:823-825.