A Huge Oral Ranula
Moosa Bahnassy
Bahnassy M. OMJ. 24, 306-307 (2009); doi:10.5001/omj.2009.63
From the Department of Surgery, Gayathi Hospital,Abu Dhabi, UAE.
Received: 13 Jul 2009
Accepted: 16 Aug 2009
Address correspondence and reprint requests to: Dr Moosa Bahnassy, Department of Surgery, Gayathi Hospital,Abu Dhabi, UAE.
E-mail: mousagalal@hotmail.com
A 24- year old Indian patient was presented to the surgical out-patient clinic in Ghayathi hospital, UAE with a painless swelling on the floor of the mouth for an estimated duration of 1 and a half years. One month prior to the hospital visit, he experienced increasing difficulty in speech, mastication and swallowing. Most recently, the patient reported breathing difficulty at night. The patient also reported feeling a bilateral intermittent swelling in the upper part of the sides of the neck, more on the left side during eating. The patient had no history of chronic illness, history of any trauma or operations on the oral cavity. General physical examination was not significant, however a local trans illuminant, slightly bluish, cystic swelling (3x5x6 cm) was found on the floor of the mouth on both sides of the midline with mild deviation from the tongue to the right side,(Fig. 1).
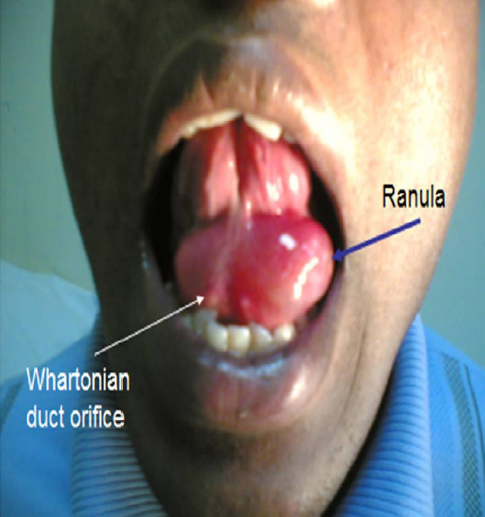
Figure 1: Showing the Ranula and the Whartonian’s Duct Orifices
The swelling did not blanch on pressure and showed crossed fluctuations across the midline. The submandibular gland orifices were quite apparent and prominent on the dome of the swelling anteriorly. The sublingual salivary glands could not be palpated. There were no other oral pathologies observed during the examination. Other salivary glands and lacrimal glands were normal. The draining cervical lymph nodes were not palpable. There were no neck swellings. The patient was diagnosed to have a large oral ranula. Results from hematological and biochemical investigations including Complete Blood Count (CBC), Erythrocyte Sedimentation Rate (ESR), Liver Function Tests (LFTs), Kindney Function Tests (KFTs), Random Blood Sugar (RBS) were all within normal limits. Chest x-ray was normal. The patient had undergone marsupialization of the ranula on the left side, however the submandibular gland duct was preserved and followed by packing of its floor for 3 days. The patient had an uneventful postoperative course and fully recovered.
Oral ranula is an extravasation pseudocyst of the sublingual salivary gland. The development of mucoceles depend on the disruption of the flow of saliva from the secretory apparatus of the salivary glands mostly due to a traumatic ductal insult or ductal occlusion.1 Ranulas are ranked 41st common oral lesions with a prevalence of 0.2 cases per 1000 people. No racial or sexual tendency has been reported for oral ranulas. They usually occur in children and young adults with a peak frequency in the second decade.2 Individuals with oral ranulas are distinguished by the presence of a painless swelling on the floor of the mouth. In very rare occasions, the mass may interfere with speech, mastication, respiration, and swallowing due to the upward and medial displacement of the tongue.
In extremely rare circumstances, as presented in this patient, these symptoms become more severe and aggravated if the swelling extends across the midline to the other side.2, 3 The management of oral ranula is usually surgical by either marsupialization or complete excision of the ranula with the offending major salivary gland. Laser abliation, either alone or after marsupialization, has been used in some patients with oral ranulas. The recurrence rate after marsupialization with packing is 0-12%.4, 5, 6
ACKNOWLEDGEMENTS
The author reported no conflict of interest and no funding was received on this work.
-
Anatassov GE, Haiavy J, Solodink P, Lee H, Lumerman H. Submandibular gland mucocele: Diagnosis and management. Oral Surg Oral Pathol Oral Radiol Endod 2000; 89:159-163.
-
Axell T. A prevalence study of oral mucosal lesions in an adult Swedish population. Odontol rev 1976; 27:1-103.
-
Harrison HD. Sublingual gland is origin of cervical extravasation mucocele. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90:404-405.
-
Morton RP, Bartley JR, Simple sublingual ranulas: Pathogenesis and management. J Otolaryngol 1995; 24:829-830.
-
Zahao YF, Chen XM, Zhang WF. Clinical review of 580 ranulas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 98:281-287.
-
Yoshimura Y, Obara S, Kondoh T, Naitoh S. A Comparison of three methods used for treatment of ranula. J Oral Maxillofac Surg 1995; 53:280-282; discussion 283.