Oman has experienced a rapid epidemiological transition from dominant infectious diseases to higher rates of lifestyle-related diseases such as diabetes, hypertension, and ischemic heart disease.1-3
Diabetes is a major public health problem and one of the most common endocrine disorders. Type 2 diabetes (T2DM) affects more than 8% of the global adult population.4,5
It is estimated that the number of people with T2DM will be 300 million by 2025.6 Three Arabian Gulf countries are among the top ten countries in the world with the highest prevalence of T2DM: Saudi Arabia (24%), Kuwait (23.1%), and Qatar (22.9%).7 In addition, the prevalence of obesity in these countries is alarming.8
The prevalence of T2DM in Oman increased from 9.6% in 1991 to 11.6% in 2000 and 12.3% in 2008.9-11 It was observed that most of the increase between 2000–2009 occurred in individuals aged 40–59 years old compared to individuals aged 20–39 years or above 60 years old.12 This phenomenon was also observed globally.13
T2DM is associated with long-term microvascular and macrovascular complications.14-16 These complications depend largely on the degree of glycemic and intensive control of cardiovascular risk factors as shown in the United Kingdom Prospective Diabetes Study (UKPDS) and other studies.17-19
Nowadays, clinicians perform glycated hemoglobin A1c (HbA1c) tests every three to six months as a standard tool for glycemic control.20 Well-structured international21-23 and national24 guidelines have been published to achieve best practices in the management of T2DM. However, adequate control of T2DM remains a challenge.
Many challenges affect the care of T2DM patients in Oman such as financial constraints, inadequate diabetes experts, health care organization, scarcity of new medications, lack of laboratory support, and patient and society support.25
Screening programs for T2DM have been proven to be cost-effective and reduce mortality.26 The national screening program for non-communicable chronic disease was launched in Oman in 2008. This program is predetermined to provide a screening service for all Omanis aged 40 and above who do not have a chronic disease. This program was successful as it caught many undiagnosed cases of T2DM.20
T2DM has serious economic impacts and burdens.27 The costs are not only those of managing T2DM but include the lost productivity and future complications.28 With its high prevalence, increasing incidence, low glycemic control rates, and associated financial impacts, T2DM is a public health priority and challenge. This cross-sectional study presents the clinical and epidemiological characteristics of T2DM registered patients in the Dhank province of Oman.
Methods
Dhank is one of the major provinces in Al-Dhahira governorate located in the North of Oman. Three health centers in Dhank provide primary health care services, including managing T2DM patients. The three centers: Dhank Health Center (DHC), Qumaira Health Center (QHC), and Fida Health Center (FHC) serve a total population of 20,367 (16,811, 1205, and 2351 people, respectively). All health services, including medications, are free of charge. Dhank province is located near the border of United Arab Emirates and between three major provinces of Oman: Ibri, Yanqul, and Buraimi. All Dhank health centers are primary health care centers and rely on Ibri Referral Hospital as a secondary care hospital.
We performed this cross-sectional study of the data of T2DM registered patients in Dhank province using their data registers and computer records. Data was collected from the diabetic national registers in the three health centers.
The annual visit characteristics of all T2DM registered patients who were alive and actively followed-up in these centers were included. The hard copy of the diabetic registers and the local electronic records were used for data collection. In Oman, a trained nurse in a diabetic register records T2DM patients’ data manually. The register includes demographic data, macro- and microvascular complications, and annual laboratory investigations values (HbA1c, lipid profile, creatinine, etc.). These data are also stored in an electronic health information program. The study period was from January 1998 to June 2015. The local health team collected the data and entered it into an electronic format. The data was reviewed, verified, and corrected by the authors.
Characteristics were identified according to age, sex, location, body mass index (BMI), blood pressure (BP), diabetic neuropathy, diabetic retinopathy, diabetic foot, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides (TG), HbA1c, and estimated Glomerular Filtration Rate (eGFR). Treatment was classified as diet only, oral hypoglycemic agents (OHA), and insulin therapy.
We used the Oman National Diabetic Manual (2010) as a reference for the normal values.
Age was divided into three groups (< 30, 30–60, and > 60 years) and the percentage of patients in each age group was calculated. The duration of diabetes was also divided into three intervals (≤ 5, 6–10, and > 10 years). The percentage of patients in each interval was calculated.
In our study, the American Diabetes Association (ADA) standards of medical care in diabetes (2013) were used.29 Glycemic control was defined by the HbA1C goal of < 7%. HbA1C control was divided into two categories: good (< 7%) and poor (> 7%). HbA1c was measured in Ibri Referral hospital using Hitachi 911, 912, or 902 automated chemistry analyzer (Boehringer Mannheim).
The BP goal was defined as systolic (< 140 mmHg) and diastolic (< 80 mmHg). The guidelines of the American National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) III (2001/2004) was used for serum lipids goals30 LDL cholesterol (optimal < 2.59 mmol/L); TG (desirable <1.69 mmol/L); and HDL cholesterol (high >1.0 mmol/L).
BMI was categorized as underweight (< 20), normal (20–24.9), overweight (25–29.9), obesity-1 (30–34.9), obesity-2 (35–35.9) and morbid obesity (>40).
Diabetic retinopathy was diagnosed according to the regional hospital’s ophthalmologist report. The eGFR were calculated by the modification of diet in renal disease (MDRD) equation.31 It was classified as normal (> 90), mild (61–90), moderate (31–60), severe (16–30), and renal failure (< 15).
The study was approved by the local Ethics and Research Committee of the Ministry of Health.
We estimated the prevalence of registered T2DM patients stratified by age for binomial events. Mean, standard deviation (SD), and proportions were calculated for the variables (clinical characteristics and diabetes-related complications). The Pearson’s chi-square test was used to compare categorical data according to sex and age while an unpaired Student’s t-test was used to compare continuous variables. A two-tailed value of p < 0.050 was considered statistically significant. Statistical calculations were performed using SPSS Statistics (SPSS Statistics Inc., Chicago, US) version 22.
Results
A total of 567 patients were identified. The demographic and clinical characteristics of the patients are shown in Table 1. Of the total 567 patients, 254 (44.8%) were men. Obesity and overweight were more prevalent among patients in the 30–59 years old compared to patients aged < 30 or ≥ 60 years (p < 0.001) [Figure 1].
The progression of BMI is associated with poor glycemic control. Those who had BMI > 40 had the worst glycemic control (p < 0.001) [Table 2].
Table 1: Demographic and clinical characteristics of 567 patients with T2DM.
|
Age, years |
55.8±15.6 |
|
Sex, n (%) |
|
|
Male |
254 (44.8) |
|
Female |
254 (44.8) |
|
Duration, years |
5.9±4.0 |
|
BMI |
29.7±6.0 |
|
LDL, mmol/L |
3.3±7.6 |
|
HDL, mmol/L |
1.4±4.2 |
|
TG, mmol/L |
2.0±7.2 |
|
HbA1c level (%) average |
8.7±2.3 |
|
HbA1c level, n (%) |
|
|
< 7.0% |
161 (28.4) |
|
> 7.0% |
406 (71.6) |
|
eGFR, mL/min/1.73 m2, n (%) |
|
|
< 15 |
2 (0.4) |
|
15-29 |
4 (0.7) |
|
30-59 |
32 (5.6) |
|
60-89 |
140 (24.7) |
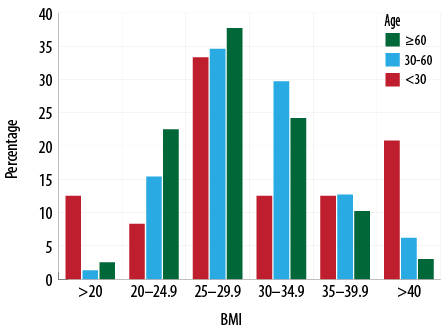
Figure 1: Relationship between body mass index and age.
Table 2: The relationship between body mass index and HbA1C.
|
< 20 |
76.9 |
|
20–24.9 |
71.3 |
|
25–29.9 |
70.0 |
|
30–34.9 |
70.2 |
|
35–35.9 |
72.7 |
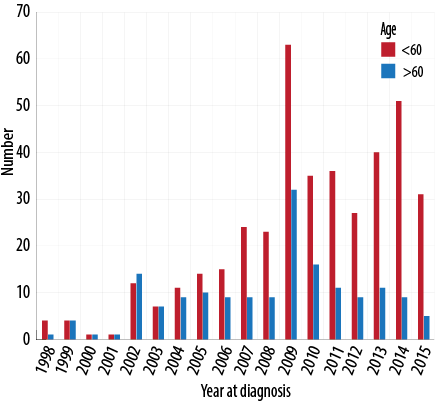
Figure 2: Year of diagnosis for patients age above and below 60 years old.
Of a total population of 16,462, 5,508 were aged 20 years or above, 567 had T2DM, which corresponds to a prevalence of 10.2%. Of these, 44.8% were men. The prevalence increased to 24% in patients aged > 60 years.
In total, about 28.4% of patients had HbA1c levels within the ADA's recommendations for good glycemic control (< 7%). Controlled HbA1c rates in the DHC, FHC, and QHC centers were 27.0%, 40.0%, and 28.5%, respectively. Glycemic control does not have sex difference or age relationship
(p = 0.700 and p = 0.240, respectively).
The majority of patients (93%) had an eGFR of ≥ 60 mL/min/1.73m2, 63.3% of patients had an HDL cholesterol level of < 1.0 mmol/L and 60.0% of patients had LDL cholesterol levels of > 2.6 mmol/L. Over one-third (34.6%) of patients had TG levels of > 1.7 mmol/L, and 43.4% of patients had a BMI > 30.
Analysis of the total number of registered T2DM patients per year showed that the number of diagnosed individuals aged under 60 increased gradually over the last seven years (2008–2015) compared to above 60 years (p = 0.017) [Figure 2].
The analysis showed the total patients were managed using lifestyle measures (14.2%) or one/two OHA (50%) while 35.7% started insulin therapy (alone or with OHA).
Discussion
The national estimate of T2DM prevalence (12.3%) is a population prevalence from a national household survey.1 Our estimated prevalence of 10.2% does not represent the true prevalence but the prevalence of the registered diabetics only. Since the Dhank province is located near the country’s border, people tend to move in and out to seek health services. Also, Dhank’s population age pyramid shows a higher population under the age of 30 (66.5%). This might indicate the migration of the older generation to nearby towns. This is supported by the fact that Dhank province is located between three major provinces: Ibri, Buraimi, and Yanqul.
Our study demonstrates that about two-thirds of patients with T2DM did not achieve the ADA goal of HbA1C (> 7). Several studies done in Oman showed different estimates of uncontrolled glycemic state: 50%,32 70%,33 65%,34 and 77.2%.35
Several international studies explored the percentage of patients with good glycemic control. One study in the USA found that only 42.3% of patients had HbA1C < 7.36
Lower rates of glycemic control could be attributed to accelerated lifestyle changes and a shift from rural labor-demanding jobs to office-based jobs leading to increased biological and behavioral risk factors.18
Although we studied the relationship between several factors and glycemic control, other major factors like health education, physical inactivity, diet control, and genetically inherited hemoglobinopathies were not studied. This might bring about the need for qualitative focused group studies.
D'souza et al,32 reported that younger age, female gender, higher education, non-tobacco use, and exposure to diabetes education programs were associated with better glycemic control. Two other studies also confirmed that hypertension (60%) and obesity (26.4%) among adults with T2DM led to poorly controlled HbA1C (67%).37,38
Although there is a rapid expansion of the primary health care (PHC) centers network throughout the country, most of the primary healthcare professionals are not adequately trained to deal with advanced diabetes cases.18 Only five family physicians are available in the Al-Dhahira governorate to supervise the management of all diabetes cases. Also, to date, new evolving diabetes medications are still flawed and lacking and is another drawback in the attempt to control T2DM.
Al-Shafaee et al,39 showed a gap between the recommended DM care guidelines and current practice in PHC centers in North Batinah. Al-Mandhari et al,40 clarified that the current interventions in Oman should highlight health education, training of primary care physicians and other patient care providers in behavioral change, and a redesign of the local systems of care delivery.
As a routine practice in the Ministry of Health (MOH), the final reading of HbA1c is used to estimate the glycemic outlook of each case. We applied this practice in our study to calculate the percentage of controlled patients. However, we strongly recommend that the average annual HbA1c value be used because this will give results that are more accurate.
This study showed that the FHC patient’s glycemic control rate was higher than that those of the DHC (FHC = 40%, DHC = 27%). FHC is considered a rural area. People in rural areas tend to be more active and live healthy lifestyles compared to people in urban areas. This finding needs more elaboration through qualitative research. Another study also observed higher prevalence rates of T2DM in urban areas (18%) compared to rural areas (11%) of the country.38
Our study revealed that the progression of BMI is associated with poor glycemic control. However, the waist circumference should be considered before reaching a conclusion. Al-Asfoor and Al-Lawati41 showed that BMI is not independently associated with T2DM once waist circumference is taken into account.41 Also, another study reported that there was no association between high BMI and poor glycemic control; however, they found a significant relationship between small waist circumference and better glycemic control.32 One-fifth of the Omani adult population is obese (of which 36.8% are diabetics).37,42
After 2008, the majority of T2DM patients were aged < 60 years old. This could be credited to the successful national screening program that was implemented in 2008. Additionally, community awareness about diabetes has increased over the last decade, and more people are interested in taking part in screening.
Although there are many publications in this field, this is the first study to assess the characteristics of T2DM patients in the Dhank province. The major strength of our study was the inclusion of all T2DM patients who were actively followed-up in Dhank.
This study can be used as a reference for the Al-Dhahira governorate to study the demographics of the people living in the area as it represents a population that carries almost the same characteristics of disease distribution. This study is limited by its cross-sectional design and is not a causal study. Other factors that are associated with glycemic status (physical inactivity, diet, and tobacco smoking) were not studied.
Oman’s health system needs to work hard to tackle the threat of non-communicable diseases, especially T2DM. The shift from acute medicine to chronic disease prevention requires huge financial resources. In 2000, Oman was ranked eighth in the world in overall health performance, according to the World Health Organization (WHO) health system attainment and performance estimates.43 Despite this, Oman’s per capita expenditure on health in 2013 ($796, USD) was still lower than those of other Arabian Gulf countries (UAE $2,233, KSA $1,681, Bahrain $1,900 and Kuwait $2,375, USD).44
Conclusion
The prevalence of the registered T2DM patients in Dhank is less than the national figure. This may be attributed to the location of Dhank as a border province. Further qualitative studies are recommended to elaborate on the factors that lead to poor glycemic control.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
We would like to thank those who participated in entering the data of this study. This includes Dr Yousef Abdulla Hamed (DHC), Dr Islam Mohammed Sheta (DHC), Alya Ghareeb Al-Yaqoubi (DHC), Beverli Notorio (QHC), and Mohammed Rafeeq Jalgaonkar (FHC).
references
- 1. Ministry of Health. World Health Survey 2008. Department of Research, Directorate General of Planning, Ministry of Health, Oman. 2011.
- 2. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008 Oct;359(15):1577-1589.
- 3. Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008 Feb;358(6):580-591.
- 4. American Diabetes Association. Standards of medical care in diabetes–2010. Diabetes Care 2010 Jan;33(Suppl 1):S11-S61.
- 5. IDF Clinical Guidelines Task Force. Global Guideline for Type 2 Diabetes: recommendations for standard, comprehensive, and minimal care. Diabet Med 2006 Jun;23(6):579-593.
- 6. Alyaarubi S. Diabetes Care in Oman: Obstacles and solutions. Sultan Qaboos Univ Med J 2011 Aug;11(3):343-348.
- 7. Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature 2001 Dec;414(6865):782-787.
- 8. Ministry of Health Manual of Diabetes Mellitus management guideline, third Edition 2014.
- 9. Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care 2005 Sep;28(9):2130-2135.
- 10. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004 May;27(5):1047-1053.
- 11. Davies M, Day J. Screening for diabetes. BMJ 1994; 308:1160–1161.
- 13. National Institute for Health and Clinical Excellence. Management of type 2 diabetes—managing blood glucose levels. Guideline G. [cited Aug 2015]. Available from: https://www.nice.org.uk/guidance/ng28/resources/type-2-diabetes-in-adults-management-1837338615493
- 13. Selvin E, Ning Y, Steffes MW, Bash LD, Klein R, Wong TY, et al. Glycated hemoglobin and the risk of kidney disease and retinopathy in adults with and without diabetes.Diabetes 2011 Jan;60(1):298-305.
- 14. Al-Adawi S. Emergence of diseases of affluence in Oman: where do they feature in the health research agenda? Sultan Qaboos Univ Med J 2006 Dec;6(2):3-9.
- 15. American Diabetes Association; European Association for the Study of Diabetes; International Federation of Clinical Chemistry and Laboratory Medicine; International Diabetes Federation. Consensus statement on the worldwide standardisation of the HbA1c measurement.Diabetologia 2007 Oct;50(10):2042-2043.
- 16. Genuth S, Eastman R, Kahn R, Klein R, Lachin J, Lebovitz H, et al; American Diabetes Association. Implications of the United kingdom prospective diabetes study. Diabetes Care 2003 Jan;26(Suppl 1):S28-S32.
- 17. Khaw KT, Wareham N. Glycated hemoglobin as a marker of cardiovascular risk. Curr Opin Lipidol 2006 Dec;17(6):637-643. CrossRefMedlineWeb of Science.
- 18. Al-Lawati J. Mabry R, Mohammed AJ. (2008) Addressing the threat of chronic diseases in Oman. Preventing chronic disease;5(3). [cited Jul 2015]. Available from: http://www.cdc.gov/PCD/issues/2008/jul/07_0086.htm.
- 19. Directorate General of Planning. Annual health reports. Muscat: Ministry of Health, Oman; 2000-2009.
- 20. International Diabetes Federation. IDF Diabetes Atlas, 5th ed. 2011 [cited July 2015]. Available from: http://www.idf.org/sites/default/files/EN_6E_Atlas_Full_0.pdf
- 21. Department of non-communicable diseases surveillance and control directorate general of health affairs. guideline for the national screening programme for chronic diseases. Ministry of health, Oman.
- 22. International Diabetes Federation International diabetes atlas. sixth edition. [cited: Aug 2015]. Available from: http: www.idf.org/sites/default/files/EN_6E_Atlas_Full_0.pdf.
- 23. Ng SW, Zaghloul S, Ali HI, Harrison G, Popkin BM; Ng SW. The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Arabian Gulf States. Obes Rev 2011 Jan;12(1):1-13.
- 19. Javitt JC. Chiang Y. Economic impact of diabetes. In: National Diabetes Data Group, editors. Diabetes in America. 2nd ed. Bethesda, MD: National Institutes of Health; 1995:601-611. (NIH publication No 95-1468.)
- 25. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study.BMJ 2000 Aug;321(7258):405-412.
- 26. Ganguly SS, Al-Shafaee MA, Al-Lawati JA, Dutta PK, Duttagupta KK. Epidemiological transition of some diseases in Oman: a situational analysis. East Mediterr Health J 2009 Jan-Feb;15(1):209-218.
- 27. Asfour MG, Samantray SK, Dua A, King H. Diabetes mellitus in the sultanate of Oman. Diabet Med1991 Jan;8(1):76-80.
- 28. Al-Lawati JA, Al Riyami AM, Mohammed AJ, Jousilahti P. Increasing prevalence of diabetes mellitus in Oman. Diabet Med 2002 Nov;19(11):954-957.
- 29. American Diabetes Association. Standards of medical care in diabetes–2013. Diabetes Care 2013 Jan;36(Suppl 1):S11-S66.
- 30. Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, et al; National Heart, Lung, and Blood Institute; American College of Cardiology Foundation; American Heart Association. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004 Jul;110(2):227-239.
- 31. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al; Chronic Kidney Disease Epidemiology Collaboration. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 2006 Aug;145(4):247-254.
- 32. D’souza MS, Venkatesaperumal R, Karkada SN, Amirtharaj A. Determinants of Glycosylated Haemaglobin among Adults with Type 2 Diabetes Mellitus. J Diabetes Metab 2013;4:265.
- 34. Al-Lawati JA, N Barakat M, Al-Zakwani I, Elsayed MK, Al-Maskari M, M Al-Lawati N, et al. Control of risk factors for cardiovascular disease among adults with previously diagnosed type 2 diabetes mellitus: a descriptive study from a middle eastern arab population. Open Cardiovasc Med J 2012;6:133-140. Published online 2 Nov 2012.
- 35. Al Balushi KA, Al-Haddabi M, Al-Zakwani I, Al Za’abi M. Glycemic control among patients with type 2 diabetes at a primary health care center in Oman. Prim Care Diabetes 2014 Oct;8(3):239-243. Published online 26 Jan 2014.
- 36. Venugopal S, Kunju R, Al Harthy S, Al Zadjali N. Hemoglobin A1c in Muscat, Oman - A 3 year study. Oman Med J 2008 Jul;23(3):170-172.
- 37. Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988-2002.Ann Intern Med 2006 Apr;144(7):465-474.
- 38. Al-Riyami AA, Afifi MM. Accuracy of self-reporting of diabetes mellitus and hypertension and its determinants among Omani adults. Saudi Med J 2003 Sep;24(9):1025-1026.
- 39. Al-Moosa S, Allin S, Jemiai N, Al-Lawati J, Mossialos E. Diabetes and urbanization in the Omani population: an analysis of national survey data. Popul Health Metr 2006;4:5-12.
- 40. Al-Shafaee M, Al-Farsi Y, Al-Kaabi Y, Banerjee Y, Al-Zadjali N, Al-Zakwani I. Quality of diabetes care in primary health centres in north Al-batinah of oman. Open Cardiovasc Med J 2014;8:48-54. .
- 41. Al-Mandhari A, Al-Zakwani I, El-Shafie O, Al-Shafaee M, Woodhouse N. Quality of Diabetes Care: A cross-sectional observational study in Oman. Sultan Qaboos Univ Med J 2009 Apr;9(1):32-36.
- 42. Al-Asfoor DH, Al-Lawati JA, Mohammed AJ. Body fat distribution and the risk of non-insulin-dependent diabetes mellitus in the Omani population. East Mediterr Health J 1999 Jan;5(1):14-20.
- 44. Al-Lawati JA, Jousilahti PJ. Prevalence and 10-year secular trend of obesity in Oman. Saudi Med J 2004 Mar;25(3):346-351.
- 46. The world health report 2000 - Health systems: improving performance [cited Mar 2016]. Available from: http://www.who.int/whr/2000/en/whr00_en.pdf
- 47. Countries. Saudi Arabia. [cited: Jul 2015[. Available from: http://www.who.int/countries/sau/en/.