Herbal medicines, including herbs, herbal preparations, and finished herbal products, contain as active ingredients parts of plants or other plant materials perceived to have therapeutic benefits.1 About 80% of the population worldwide use a variety of traditional medicine, including herbal medicines, for the diagnosis, prevention and treatment of illnesses, and for the improvement of general well-being.2 In the Arab world, traditional medicine has always been practiced despite the advances in modern medicine. The concept of traditional Arabic herbal medicine has increasingly generated worldwide interest among the herbalists and the scientific community.3
Pregnancy is a condition associated with immense physiological alterations resulting in many pregnancy- related problems, including nausea, vomiting, constipation, and heartburn.4 These aliments usually result in pregnant women self-medicating using over-the-counter (OTC) medications, seeking prescribed medications, or using herbs.5 Herbal products are preferred over prescription medications due to the belief that herbs are safer for the fetus than modern medicine. Despite the fact that evidence on the safety profile of herbal products is inadequate to substantiate their use in pregnancy, it is increasingly used by expectant mothers. The prevalence of herbal medicine utilization in pregnancy ranges between 7% and 55% in different geographical, social and cultural settings, and ethnic groups.6
Medications, herbs, and supplements should be used with extreme caution during pregnancy as they can result in deleterious outcomes for the mother and fetus.7 The use of herbal medicines in pregnancy constitutes a major challenge for health care providers as most of them are not made aware of their use.8 When prescribed appropriately traditional herbal medications are safe, with rare incidences of life-threatening events.9 Injudicious use of herbs or interaction of these herbs with prescribed medications can have unknown effects in pregnancy or cause serious complications in the fetus.10
The use of herbal medications does not have strict regulations like modern medicines and, in light of this rising trend in their use, the use of these products, particularly in pregnancy, is a matter of concern. Here we reviewed the available literature on the prevalence of herbs and herbal products use in pregnancy in the Middle East and the attitudes of pregnant women on herbal medications. The results of this review will help health care providers in patient education and counseling patients about the use of herbal medicine.
Methods
A publication search was conducted in the MEDLINE, Proquest, Google Scholar, and EMBASE databases, using a combination of medical subject headings (MeSH) terms and keywords. The MeSH terms included herbs, herbal medicine, herbal products, pregnancy, and pregnant women. We also used the names of different countries in the Middle East as search terms (including Bahrain, Egypt, Iran, Iraq, Israel, Jordan, Kuwait, Lebanon, Oman, Palestinian Territories, Qatar, Saudi Arabia, Syria, United Arab Emirates, and Yemen). A total of nine papers published between January 1990 and December 2012 met the selection criteria and were included in the review.11-19 An overview of the review process is given in Figure 1.
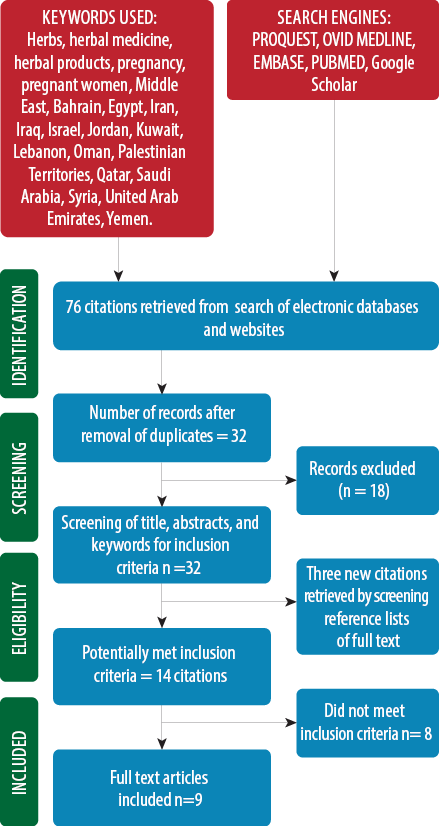
Figure 1: Flowchart showing overview of the review process
All published English language full-text articles from the Middle East region on the use of herbal products and therapies during pregnancy were selected. We independently identified and evaluated all relevant scientific medical literature that provided information about the use of herbs, and herbal products and therapies during pregnancy including the prevalence, type of herbal products, condition of use, source of information, referral source and perception, and self-reported evaluation of herbal medicine by pregnant women. Each journal article was scrutinized as per the selection criteria and was referenced for the review. The results of this initial screening by both authors were cross-referenced between them and full-text records obtained for all potentially relevant reports. The reference lists of all the included articles were also checked. Disagreements between the authors about the studies to be included were resolved through discussion. The information extracted from each study included the study characteristics, participants, user prevalence, pattern of use, referral and information sources, and perception and self-reported evaluation. The results of the analysis have been given in Tables 1, 2, and 3. As the study results were diverse, we did not proceed with meta-analysis and, instead, a separate presentation of the results from each study in a structured format was performed.
Results
Of the nine studies included in the review, there were four articles from Iran, two from Palestine and one article each from Oman, Qatar, and Egypt.11-18 Eight of the articles were original research articles published in journals and the study from Iran was a dissertation. All nine articles employed questionnaires/surveys among pregnant women on use of herbal medicine during pregnancy, type of herbal products, condition of use, source of information, referral source.11-19 Six studies discussed the perception and evaluation of herbal medicine in pregnancy. The findings of the were extracted and the results compiled under three themes: user profile, prevalence, pattern of use and referral, information sources, and perception and self-reported evaluation. The sociodemographic profile of the pregnant women from nine studies included for this review is shown in Table 1.
Table 1: User profile of studies on herbal medicine use among pregnant women from the Middle East.
|
Al-Riyami et al, 201111 |
Oman |
139 |
28±5
Range: 19–45 |
No schooling: 2.2%; primary:15.8%; secondary: 44.6%; college:17.3%; higher education: 20.1% |
Employed: 36%
Unemployed: 64% |
|
|
First: 7.2%
Second: 36.0%
Third: 56.8% |
|
Tabatabaee et al, 201112 |
Iran |
513 |
≤25 (56.3%); 26–30 (30.0%)
31–35 (9.7%); >36 (3.9%) |
≤8 years: 63.5%; 9–12 years: 25.1%; >12 years: 11.3% |
Homemaker: 94.3% |
Urban: 29.6%
Rural:70.4% |
Primipara: 58.5%
Multipara:41.5% |
|
|
Dabaghian et al, 201213 |
Iran |
600 |
27.03±4.8 |
Uneducated: 2.5%; <12 years: 23.3%; 12 years: 51. 8%; >12 years: 22.4% |
Homemaker: 87.2%
Others 12.8% |
Urban: 81.7%
Rural:18.3% |
1.6(0.81) |
|
|
Sattari et al, 201214 |
Iran |
400 |
26.4±5.2 |
High school: 46.0%; diploma: 36.8%;
graduate: 17.3% |
|
Urban:72.3%
Rural:27.8% |
None: 50.0%
One: 31.8%
Two: 13.5% |
|
|
Sawalha et al,
200715 |
Palestine |
218 |
28.1±5.7 |
Elementary:40.8%; high school: 39.9%; university: 19.3% |
|
Urban: 24.8%
Rural: 70.2%
Others: 5.0% |
3.8(2.4) |
First: 6.0%
Second: 8.7%
Third: 67.0% |
|
Hashim et al, 200516 |
Qatar |
393 |
29 |
Primary school :3.5%; secondary school: 21.9%; university: 74.6% |
|
|
Multiparous 66.7% |
|
|
Khadivzadeh et al, 201217 |
Iran |
919 |
25.7 ±5.1 |
Illiterate:2.7%; elementary school:24. 6%; high school: 66.2%; academic studies: 5.9%; missing: 0.6% |
Unemployed: 95.8%
Other workers: 0.8%
Employe: 2.7%
Missing:0.7% |
Urban: 13.7%
Rural: 86.0%
Missing: 0.3% |
|
|
|
Orief et al, 201218 |
Egypt |
300 |
26.9± 4.9 |
Illiterate:4.0%; basic education: 19.0%; secondary or higher: 77.0% |
|
|
1.2± 1.0 |
First: 33.3%
Second: 33.3%
Third: 33.3% |
The prevalence of use of herbal medicines among pregnant women from the Middle East varied from 22.3% to 82.3%. The most commonly used herbs were: peppermint, ginger, thyme chamomile, sage, aniseeds, fenugreek, green tea, and garlic. The herbs were most frequently used to treat gastrointestinal disorders such as nausea, vomiting, bloating, and stomach aches followed by cold and flu symptoms.
Their use varied with each trimester, and depending on the pregnancy-related problems associated. Ginger was used for nausea and vomiting in the first trimester and for treating symptoms of the common cold.
Across all the trimesters, green tea was used as a laxative and a relaxing agent; peppermint, thyme, and cinnamon were used for bloating and stomach aches. Thyme was also used for common cold and urinary tract infections and garlic was used for urinary tract infections. Chamomile was used as a relaxing agent during the first and third trimesters. Sage, aniseeds, and fenugreek were used across all trimesters for flatulence and in the third trimester for their oxytocic effect.
The majority of the studies reported the highest use of herbs during the first trimester with the frequency varying from 17.3% to 67.5%.11,12,16,17,19 Women were most commonly advised to try herbal medications by family and friends. Some studies also reported health care professionals (e.g. general practitioners, obstetricians, and midwives) as the source of information concerning use of herbal medicines.18,19
Table 2 summarizes the prevalence, pattern of herbal medicine use, and referral and information sources reported by the studies.
Two studies reported that women informed their physicians of their herbal medicine use. This number was 37.2% in a study from Iran13 and 65.8% in a study from Palestine.19
Table 3 reveals details of the pregnant mother’s perception and self-reported evaluation of herbal medicine.
Six studies discussed the perception/self-evaluation of herbal medicine in pregnancy. The majority of these studies reported that the women believed that herbal medicines were more effective than conventional medicine and had fewer side effects especially during pregnancy. The other common perception was that herbal medicines were more accessible without a doctor’s prescription.
Discussion
The prevalence of herbal medicines use among pregnant women from the Middle East varied from 22.3% to 82.3%. Most women in the studies were from rural areas, homemakers, and had an educational qualification below graduation. This was in accordance with studies outside the Middle East which reported higher usage of herbs among women from rural areas that were less educated.20-23 Commonly used herbs were peppermint, ginger, thyme, chamomile, sage, aniseed, fenugreek, and green tea. The frequently used herbs in most studies were similar to other studies from the Middle East. In contrast, the herbs most commonly used in Australia, Norway, and Tuscany were raspberry, fennel, and St. John’s wort.24-26
The use of the herbal products varied with the trimester and associated pregnancy-related problems. Although herbal products may offer a benefit, it is important to detect even small risks that would significantly affect the risk-benefit ratio in pregnancy.
Table 2: Prevalence and pattern of herbal medicine use, referral, and sources of information among pregnant women from the Middle East.
|
Al-Riyami et al, 201111 |
23.8% |
Ginger: 7.9%; honey: 6.5%; thyme: 5.0%; green tea: 3.6% |
Flu and cold: 9.4%; flatulence: 6.5%
Nausea: 5.0%; infection: 4.3% |
NR |
NR |
First:17.3%
Second:17.1%
Third:15.0% |
|
Tabatabaee et al,
201112 |
82.3% |
Ammi: 22.6%; saatar: 12.6%; sweet basil: 28.0%; peppermint: 9.0%; ginger: 5.4%; cinnamon: 5.4%; chamomile: 4.5% |
GI related problem: 32.1%; nausea and vomiting:20.2%; prevent neonatal hyperbilirubinemia:14.7%; common cold:11.0%
Urinary tract infection:5.5%; sedation: 4.6%
increase child intelligence: 3.7% |
Family: 87.3%; primary maternity care providers: 7.6%; friends; neighbors: 2.5%; midwife: 2.5% |
NR |
First: 36.7%
Second:15.2%
Third: 31.0%
Any time: 17.1% |
|
Dabaghian et al, 201213 |
67.0%
Mean: 2.7±1.9 herbs/individual |
Peppermint: 32.8%; olibanum: 26.3% |
Bloating, stomach ache:30.2%; respiratory infections:18.7%; nausea; vomiting:11.5%;
heart burn:8.7%; anxiety:4.7%,
Sleep disorders:4.7%; skin problems:2.9% |
Family/friends: 77.5%; herbalists/pharmacist/other pregnant women; gynecologist: 9.7%; general physician: 5.2% |
Family, friends: 60.2%
Books/newspapers/magazines/internet: 49.7%
Herbal store/
pharmacy: 26.7%
Television: 15.5%
Physician: 12.8% |
NR |
|
Sattari et al, 201214 |
22.3% |
NR |
NR |
NR |
Physicians: 46.0%
Family/friends: 9.0%
Self: 44.9% |
NR |
|
Sawalha et al,
200715 |
45.8% |
Sage, aniseeds, chamomile,
thyme, fenugreek, mixture of herbs, garlic, ginger |
Abdominal pain:36.0%; anxiety: 14.5%; Flu: 13.3%; cough: 9.6%. |
Self: 55.1%; families; friends:27.6%; herbalists; pharmacists; other pregnant women; gynecologist:9.7%; general physician:5.2% |
NR |
NR |
|
Hashim et al, 200516 |
65.2% |
Herbal mixes: 24.0%; ginger:17.0%; aniseed: 1.0%; fenugreek: 9%; mint: 9.0%; thyme, sage; lemon: 8.0%;
chamomile: 6.0% |
Indigestion, cold and flu, tension relief, urinary tract infection (UTI), constipation, stomach pain. vomiting, abdominal cramps, good for health |
NR |
Friends/family: 65%, Magazines/TV/newspapers: 13.0%, Internet: 7.0%,
General practitioner: 4.0%, Gynecologist: 4.0%
Herbalist: 2.0% |
First:67.5%
Second:37.7%
Third: 28.9%
(usage of herbal medicine alone not reported) |
|
Khadivzadeh et al, 201217 |
49.2% |
Traditional herb: 73.2%
Herb based drugs: 26.8% |
Increase child’s intelligence: 49.5%; heartburn: 10.5%; cold and flu: 6.1%; nausea; vomiting: 5.7%; strong; beautiful child: 5.3%; gastric pain:1.4%; bloating:1.4% |
NR |
Friends/family: 33.5%; obstetricians/midwives: 41.5%; books/magazines: 6.7%; traditional; healers: 3.6%; Radio/TV: 5.1% |
First:64.3%
Second: 28.9%
Third: 5.4%
(usage of herbal medicine alone not reported) |
|
Orief et al,
201218 |
27.3% |
Ginger: 29.3%; peppermint: 11.0%; fenugreek: 31.7%; green tea: 19.5%; garlic: 22.0%; aniseed: 40.2% |
Nausea/vomiting: 28.0%; abdominal colic: 47.6%; dysuria: 9.7%; headache: 2.4%
no indication: 18.2% |
|
Physicians: 11.0%; self: 18.3%; friends: 28.0%
Family: 42.7% |
|
NR: not reported
Table 3: Perception and self-reported evaluation of herbal medicine use among pregnant women from the Middle East.
|
More effective than conventional medicine |
15.7% |
42.9% |
NR |
64.6% |
91.7% |
56.2% |
|
More effective than conventional medicine for some medical conditions |
14.9% |
NR |
NR |
NR |
NR |
NR |
|
Herbal medicine together with conventional medicine are effective |
6.5% |
NR |
NR |
NR |
NR |
NR |
|
Less side effects than conventional medicine |
23.4% |
NR |
39.8% |
NR |
82.5% |
52.4% |
|
Less side effects than conventional medicine during pregnancy |
21.6% |
53.0% |
NR |
NR |
NR |
NR |
|
More accessible than conventional medicine |
18.7% |
NR |
NR |
NR |
NR |
NR |
|
Less expensive than conventional medicine |
14.9% |
NR |
NR |
NR |
NR |
NR |
|
Accessible without doctor’ prescription |
21.6% |
NR |
NR |
NR |
8.3% |
NR |
|
In some conditions, herbal medicine effects faster than conventional medicine |
9.7% |
NR |
NR |
NR |
NR |
NR |
|
Agree with use of herbal medicine during pregnancy |
18.4% |
NR |
NR |
NR |
NR |
NR |
|
Prefer to use herbal medicine for some conditions during pregnancy |
19.9% |
NR |
NR |
NR |
NR |
NR |
|
If conventional medicine don’t work, I would try herbal medicine |
13.7% |
NR |
NR |
NR |
NR |
NR |
NR: not reported
Evidence on efficacy and safety in pregnancy for most of these herbs is limited. A meta-analysis reported that ginger is safe and efficacious in nausea and vomiting during pregnancy.27 A high incidence of threaten miscarriages and preterm labor have been reported with the use of chamomile and licorice during pregnancy.28 In a review on the herbs used for morning sickness, chamomile and peppermint were reported as unsafe in 6% of studies and ginger and raspberry leaf were cited as unsafe in 12% and 15% of the studies, respectively.29 Excess use of peppermint is contraindicated in early pregnancy due to its emmenagogue effects.30 Fenugreek also needs to be consumed with caution during pregnancy due to its hypoglycemic effect and its stimulatory effect on oxytocin secretion resulting in uterine contraction.18
Most of the herbs are safe when used in moderation; and excessive consumption can produce unknown effects.31 For example, although the caffeine content in green tea is 30–60% less than in coffee, it is recommended to avoid consumption of large quantities due to its interference with various metabolic processes.32 The fact that these unsafe herbs are among those commonly used is a matter of concern.
The majority of studies reported maximum use of herbs during the first trimester; probably due to the higher incidence of pregnancy-related problems during this period. Most women are unaware that the first trimester is the most critical period of pregnancy when fetal organogenesis occurs and utmost care should be taken to reduce the risk of fetal morbidity and mortality.33 It is a well-documented fact that the risk in pregnancy is unknown for 91.2% of the approved medications.34 The use of herbal products which are not usually tested in clinical trials during pregnancy could result in immense risk to the mother and fetus.35
Since herbal medicines are a part of traditional medicine, they are not included in the FDA pregnancy categories giving a false impression of safety. The whole extracts of these herbal drugs contain numerous active molecules that could elicit adverse effects including teratogenicity.36,37 Moreover, these preparations are sold as unlicensed food supplements or as over-the-counter items, which are not regulated with the same scrutiny as conventional drugs thus increasing the probability of contamination or adulteration with poisonous metals, non-declared herbs or conventional medicines.38 Use of herbal medicine concurrently with conventional medications could result in herb-drug interactions and undesirable effects.10 Due to the widespread use of herbal drugs during pregnancy, there is a need for regulation of these drugs to ensure their safety and determine the efficacy and constituents of the preparations.
Family and friends were the common referral/ information sources in the studies. There is high prevalence of use of alternative medicine in the general population and suggestions for its use in pregnancy are typically based on individuals own experiences or of those around them.39 The scientific rationale in using these medications have to be considered and this insight may be lacking in these cases. The studies reviewed also reported healthcare professionals as the source of information (12.8–46%). In a study from Norway, 80.7% of the physicians rated their knowledge of herbal drugs to be poor.40 Therefore, health care professionals should update their knowledge on the efficacy, potential risks, possible herb-drug interactions and consequences, and the key principles applied to the administration of herbs during pregnancy and should also screen their patients for use of herbal medicines.41
Two studies, one from Iran and another from Palestine reported that 37.2% and 65.8% of pregnant women , respectively, informed their physicians about the use of herbal medicines.13,19 Data from outside the Middle East reported a physician reporting rate between 24% and 52%.33,42 This could be because the women did not perceive it to be important to notify their doctors.7
Pregnant women need to inform their physician about any herbs used preferably before use. We would also advise that physicians specifically ask about herbs usage and document it in the patient record. Pregnant mothers should be informed of the potential risks posed by herbs during pregnancy and advised to avoid their use.
Herbal medicines were commonly percieved to be more effective, have fewer side effects, and as more accessible without a doctor’s prescription than conventional medicines. Although they are considered safe, in reality it is known that the active ingredients in herbs that can cause serious adverse effects.36 Hence, pregnant women should be educated to increase their awareness regarding the effects of herbal medications and the importance of taking guidance from their healthcare provider.
This review is one of the first reports to shed light on the prevalence, utilization pattern, and perceptions of herbal medicine use among pregnant women in the Middle East. However, the prevalence identified may not represent the true prevalence due to the variations in the studies. We found majority of the published literature was predominantly from one country and no literature was found from many of the countries in the region.
Conclusion
A widespread use of herbs during pregnancy was observed in the Middle East, similar to other parts of the world. The wide ranges of herbal products used were representative of the traditions and geographical diversity of the region. Herbs with documented untoward outcomes for pregnancy and the fetus were also frequently used, which is a matter of concern. The majority of women used these herbs during the first trimester, the most critical period in pregnancy. The relative dearth of evidence of either their efficacy or safety is an important concern to be addressed by researchers. Multicentric research including representative samples from different countries in the Middle East would more accurately estimate the true prevalence in the region. Randomized controlled trials are also required to document the safety and efficacy of these therapies.
Disclosure
The authors declared no conflicts of interest.
references
- World Health Organization. Traditional medicine. Geneva. 2008. Available at http://www.who.int/medicines/areas/traditional/en/. Accessed February 4, 2013.
- World Health Organization. Traditional medicine. Fact sheet Number 134. Available at http://www.who.int/mediacentre/factsheets/fs134/en/. Accessed February 4, 2013.
- Azaizeh H, Saad B, Cooper E, Said O. Traditional Arabic and Islamic Medicine, a Re-emerging Health Aid. Evid Based Complement Alternat Med 2010 Dec;7(4):419-424.
- Lindzon G, Sadry S, Sharp J. Obstetric. In: Toronto Notes for Medical students. 27th Edition. Type & Graphics Inc. Canada, 2011.
- Wells BG. Gynecologic and obstetric disorders. In: Wells BG, Dipiro JT., Scwinghammer, LT, Dipiro CV. Pharmacotherapy handbook. 7th Edition. The McGraw-Hill Companies. United States of America, 2009.
- Dugoua JJ. Herbal medicines and pregnancy. J Popul Ther Clin Pharmacol 2010;17(3):e370-e378.
- Bercaw J, Maheshwari B, Sangi-Haghpeykar H. The use during pregnancy of prescription, over-the-counter, and alternative medications among Hispanic women. Birth 2010 Sep;37(3):211-218.
- Adams J. Growing popularity of complementary and alternative medicine during pregnancy and implications for healthcare providers. Expert Rev Obstet Gynecol. 2011;6(4):365-366 .
- Alrawi SN, Fetters MD. Traditional arabic & islamic medicine: a conceptual model for clinicians and researchers. Glob J Health Sci 2012 May;4(3):164-169.
- Holst L, Nordeng H, Haavik S. Use of herbal drugs during early pregnancy in relation to maternal characteristics and pregnancy outcome. Pharmacoepidemiol Drug Saf 2008 Feb;17(2):151-159.
- Al-Riyami IM, Al-Busaidy IQ, Al-Zakwani IS. Medication use during pregnancy in Omani women. Int J Clin Pharm 2011 Aug;33(4):634-641.
- Tabatabaee M. Use of herbal medicine among pregnant women referring to Valiasr Hospital in Kazeroon, Fars, South of Iran. J Med Plants. 2011;10(37):96-108.
- Dabaghian FH, Fard MA, Shojaei A, Kianbakht S, Zafarghandi N, Goushegir A. Use And Attitude on Herbal Medicine in a group of Pregnant Woman in Tehran. J Med Plants. 2012;11(41):22-33.
- Sattari M, Dilmaghanizadeh M, Hamishehkar H, Mashayekhi SO. Self-reported Use and Attitudes Regarding Herbal Medicine Safety During Pregnancy in Iran. Jundishapur J Nat Pharm Prod 2012;7(2):45-49.
- Sawalha AF. Consumption of Prescription and non-Prescription Medications by Pregnant Women: A Cross Sectional Study in Palestine. Islam Univ J. 2007;15(2):41-57.
- Hashim M, Johina A, Deyaa K, Fareeda M, Mohamed H, Faten A. Knowledge attitude and practice of complementary and alternative medicine (CAM) among pregnant women: a preliminary survey in Qatar. Middle East J Fam Med. 2005;7(10):6-14.
- Khadivzadeh T, Ghabel M. Complementary and alternative medicine use in pregnancy in Mashhad, Iran, 2007-8. Iran J Nurs Midwifery Res 2012 May;17(4):263-269.
- Orief YI, Farghaly NF, Ibrahim MIA. Use of herbal medicines among pregnant women attending family health centers in Alexandria. Middle East Fertil Soc J; 2012. Available at http://dx.doi.org/10.1016/j.mefs.2012.02.007. Accessed February 3, 2013.
- Adawi DH. Prevalence and Predictors of Herb Use during Pregnancy (A study at Rafidia Governmental Hospital/ Palestine). Available at http://scholar.najah.edu/sites/default/files/all-thesis/deema_adawi.pdf. Accessed February 3, 2014.
- Cuzzolin L, Francini-Pesenti F, Verlato G, Joppi M, Baldelli P, Benoni G. Use of herbal products among 392 Italian pregnant women: focus on pregnancy outcome. Pharmacoepidemiol Drug Saf 2010 Nov;19(11):1151-1158.
- Broussard CS, Louik C, Honein MA, Mitchell, AA. Herbal use before and during pregnancy. Am J Obstet Gynecol. 2010; 202(5): 443.e1-e6.
- Forster DA, Denning A, Wills G, Bolger M, McCarthy E. Herbal medicine use during pregnancy in a group of Australian women. BMC Pregnancy Childbirth 2006;6:21-29.
- Gharoro EP, Igbafe AA. Pattern of drug use amongst antenatal patients in Benin City, Nigeria. Med Sci Monit 2000 Jan-Feb;6(1):84-87.
- Forster DA, Denning A, Wills G, Bolger M, McCarthy E. Herbal medicine use during pregnancy in a group of Australian women. BMC Pregnancy Childbirth 2006;6:21-30.
- Lapi F, Vannacci A, Moschini M, Cipollini F, Morsuillo M, Gallo E, et al. Use, attitude and knowledge of complementary and alternative drugs among pregnant women: a preliminary survey in Tuscany. Evid Based Complement Alternat Med 2010 Dec;7(4):477-486.
- Nordeng H, Havnen GC. Use of herbal drugs in pregnancy: a survey among 400 Norwegian women. Pharmacoepidemiol Drug Saf 2004 Jun;13(6):371-380.
- Moradi Lakeh M, Taleb AM, Saeidi M. Efficacy and safety of ginger to reduce nausea and vomiting of pregnancy: a systematic review and meta-analysis. Payesh. 2008 Oct;7:345-354.
- Cuzzolin L, Francini-Pesenti F, Verlato G, Joppi M, Baldelli P, Benoni G. Use of herbal products among 392 Italian pregnant women: focus on pregnancy outcome. Pharmacoepidemiol Drug Saf 2010 Nov;19(11):1151-1158.
- Wilkinson JM. What do we know about herbal morning sickness treatments? A literature survey. Midwifery 2000 Sep;16(3):224-228.
- Fleming T. PDR for herbal medicines. 4th ed. Thomson health care Inc. USA. 2009, pp: 121,414, 522, 649.
- Kee JL, Hayes ER, McCuistion LE. Pharmacology: A Patient-Centered Nursing Process Approach. 8th Edition. Elsevier Health Sciences. 2014. p.61-78.
- Navarro-Perán E, Cabezas-Herrera J, García-Cánovas F, Durrant MC, Thorneley RN, Rodríguez-López JN. The antifolate activity of tea catechins. Cancer Res 2005 Mar;65(6):2059-2064.
- Ernst E. Risk associated with complementary therapies In: Dukes MNG, Aronson JK (eds) Meylers. Side - Effects of Drugs. 14th Edition. Elsevier, Amsterdam. 2000: 1649.
- Lo WY, Friedman JM. Teratogenicity of recently introduced medications in human pregnancy. Obstet Gynecol 2002 Sep;100(3):465-473.
- Marcus DM, Snodgrass WR. Do no harm: avoidance of herbal medicines during pregnancy. Obstet Gynecol 2005 May;105(5 Pt 1):1119-1122.
- Cuzzolin L, Benoni G. Safety issues of phytomedicine in pregnancy and pediatrics. In: Ramawat KJ (ed). Herbal Drugs: Ethnomedicine to Modern Medicine. Springer-Verlag Berlin Heidelberg 2009: 382.
- Tiran D. The use of herbs by pregnant and childbearing women: a risk-benefit assessment. Complement Ther Nurs Midwifery 2003 Nov;9(4):176-181.
- Aasland OG, Borchgrevink CF, Fugelli P. [Norwegian physicians and alternative medicine. Knowledge, attitudes and experiences]. Tidsskr Nor Laegeforen 1997 Jun;117(17):2464-2468.
- Elolemy AT, Albedah AM. Public knowledge, attitude and practice of complementary and alternative medicine in riyadh region, saudi arabia. Oman Med J 2012 Jan;27(1):20-26.
- Thomas K, Coleman P. Use of complementary or alternative medicine in a general population in Great Britain. Results from the National Omnibus survey. J Public Health (Oxf) 2004 Jun;26(2):152-157.
- Duraz AY, Khan SA. Knowledge, attitudes and awareness of community pharmacists towards the use of herbal medicines in muscat region. Oman Med J 2011 Nov;26(6):451-453.
- Pinn G, Pallett L. Herbal medicine in pregnancy. Complement Ther Nurs Midwifery 2002 May;8(2):77-80.