|
Abstract
Müllerian agenesis (Mayer-Rokitansky-Küster-Hauser syndrome) is typically described as missing uterus and fallopian tubes with malformation of the upper vagina. Isolated uterine anomaly is a rare variant of the syndrome. A 16-year-old female with primary amenorrhea and rudimentary uterus on the magnetic resonance imaging (MRI) was reported. The ovaries, vaginal canal and other abdominal and pelvic organs were normal. The patient’s sexual, physical and developmental characteristics were normal. The serum follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol, prolactin, testosterone and thyroid-stimulating hormone (TSH) were also normal. Thus, this patient represents an important variant of the Müllerian agenesis syndrome.
Keywords: Amenorrhea; Mullerian aplasia.
Introduction
Primary amenorrhea is defined as absence of menses at 15 years of age with normal growth and sexual characteristics.1 Chromosomal anomalies account for about 50% of the causes.2 The second most common etiology is Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. This rare (about 1 in 5,000 female births) entity describes specific malformations of the Müllerian duct, resulting in absence or hypoplasia of the uterus and fallopian tubes with variable malformations of the upper two thirds of the vagina. These findings can be isolated (type I) or associated with renal, skeletal, auditory or cardiac anomalies (type II, known as Müllerian duct aplasia, renal aplasia, and cervicothoracic somite dysplasia, or MURCS).3 Otherwise, patients have normal female karyotype and functional ovaries.3,4 Isolated uterine anomaly (rudimentary uterus) is a rare variant of the syndrome and is reported here.
Case Report
This 16-year-old girl was seen for evaluation of absent menses. The development of her breast, pubic hair, axillary hair and external genitalia were also normal. Her review of systems, past-medical history and family history were otherwise unremarkable. The patient had normal height, weight and sexual characteristics (sexual maturity rating V). The serum levels of FSH, LH, estradiol, prolactin, testosterone and TSH were all normal. Chromosomal analysis showed normal female karyotype (46XX). Pelvic and abdominal ultrasound and MRI revealed isolated uterine anomaly (rudimentary uterus; size: 1.73 cm x 1.22 cm x 1.70 cm), Fig. 1-2. The ovaries and vaginal canal were normal (Fig.1-2). The patient had no associated renal, skeletal or other anomalies and she was counseled on the option of uterine transplantation along with her family.
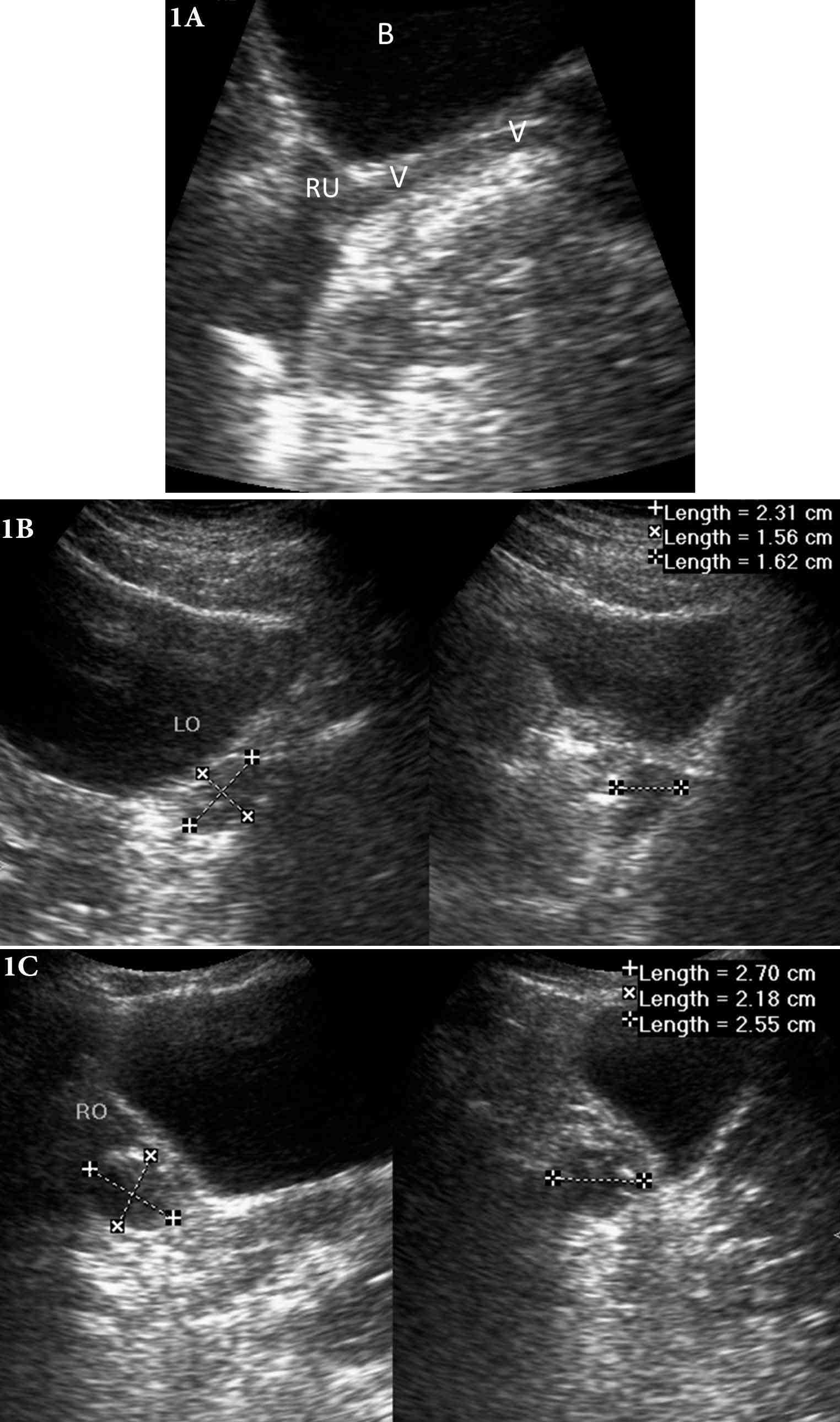
Figure 1: Trans-abdominal sagittal ultrasound of the lower pelvis. Panel A: Vagina (V) and rudimentary uterus (RU) (1.73 x 1.22 x 1.70 cm) located behind the urinary bladder (B). Panel B: Left ovary (LO) with measurements, 2.31 x 1.56 x 1.62 cm. Panel C: Right ovary (RO) with measurements, 2.7cm x 2.18 cm x 2.55 cm (2).
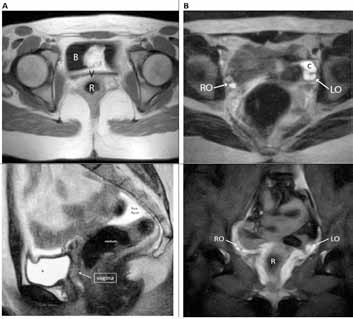
Figure 2: MRI of the pelvis. Panel A: Axial T1 weighted MRI at the level of the upper vagina B=urinary bladder, V=vagina, R=rectum. Panel B: Axial T2 weighted MRI of the lower pelvis. RO= right ovary, LO= left ovary, C=cyst. Panel C: Mid sagittal T2 weighted MRI of the lower pelvis, vagina and small rudimentary uterus, small amounts of free pelvic fluid, most likely after ovulation. B=urinary bladder, RU=rudimentary uterus. Panel D: Coronal T2-STIR MRI showing the ovaries. RO=right ovary, LO= left ovary, R=rectum.
Discussion
MRKH syndrome was first described by Mayer et al. in 1829, as Müllerian agenesis. Subsequently, Rokitansky and Küster defined the syndrome as absence of the uterus, fallopian tubes and upper vagina. The ovaries and external genitalia are characteristically normal.3 Magnetic resonance is considered as the most specific diagnostic tool.5
Sixteen patients with the syndrome were reported in Saudi Arabia; four had other anomalies (two had renal anomalies, one had skeletal anomalies and one had hyperprolactinemia).6,7 A case was reported in United Arab Emirates, describing MRKH patient with renal abnormality and utero-ovarian inguinal hernia.8 Sporadic reports from Oman and Kuwait also pointed to associated anomalies, such as renal diseases.9,10 The treatment option for these patients is neovagina, which gives opportunity for a normal sexual life.3,4 Surrogate pregnancy is the only method for having a child.4 The outcome of surrogate pregnancies with MRKH patients as the genetic mothers suggests the syndrome is a polygenic (multifactorial) trait.6
Screening newly diagnosed patients for psychological distress identifies individuals who may benefit from long-term counseling.9 MRKH syndrome has a lasting negative impact on affected women (phobic anxiety, psychoticism, depression and anxiety) and self-esteem (body image, identity and femininity impairment).11,12
In animal model, there was successful pregnancy in a rabbit with transplanted uterus.13 Successful human uterine transplantations were reported recently.14-16 One of the reported recipients had menarche 20 days after the transplant.14 The described patient with isolated uterine anomaly (rudimentary uterus) is the best candidate for this intervention.
Conclusion
This reported case represents an important variant of the Müllerian agenesis syndrome and raises several challenges in management. These include lifelong supportive counseling, corrective neovagina surgery, the possibility of surrogate pregnancy and the potential of undergoing successful human uterine transplantation.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Practice Committee of the American Society for Reproductive Medicine. Current evaluation of amenorrhea. Fertil Steril 2006 Nov;86(5)(Suppl 1):S148-S155.
2. Reindollar RH, Byrd JR, McDonough PG. Delayed sexual development: a study of 252 patients. Am J Obstet Gynecol 1981 Jun;140(4):371-380.
3. Ozkurt H, Cenker M, Keskiner F, Basak M. Cases of Mayer-Rokitansky-Küster-Hauser Syndrome with situs inversus totalis: coincidence or co-Existence? case report. J Pediatr Adolesc Gynecol 2009;22:57-60.
4. Morcel K, Camborieux L, Guerrier D; Programme de Recherches sur les Aplasies Müllériennes. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. (Review). Orphanet J Rare Dis 2007;2:13.
5. Pizzo A, Laganà AS, Sturlese E, Retto G, Retto A, Dominici R, et al. Mayer-Rokitansky-Kuster-Hauser Syndrome: Embryology, Genetics and Clinical and Surgical Treatment, review article. ISRN Obstet Gynecol 2013;628717:10.
6. Al-Najashi S, Khwaja S, Al Sibal M, El Yahia A. Mayer-Rokitansky-Kuster-Hauser Syndrome: A Study of Fifteen Cases. Bahrain Med Bull 1995;17:3.
7. Al-Jaroudi DH, Nasser AM. Mayer-Rokitansky-Kuster-Hauser syndrome with hyperprolactinemia. Saudi Med J 2008 Jun;29(6):901-903.
8. Al Omari W, Hashimi H, Al Bassam MK. Inguinal uterus, fallopian tube, and ovary associated with adult Mayer-Rokitansky-Küster-Hauser syndrome. Fertility and Sterility, 2011; 95(3):1119.e1-4
9. Pandey B, Hamdi IM. Mayer-Rokitansky-Küster-Hauser syndrome of Müllerian agenesis [corrected]. Saudi Med J 2003 May;24(5):532-534.
10. Wani MM, Mir SA. Chronic kidney disease in Mayer-Rokitansky-Kuster-Hauser Syndrome. Indian J Nephrol 2010 Oct;20(4):214-216.
11. Szarras-Czapnik M, Lew-Starowicz Z, Zucker KJ. A psychosexual follow-up study of patients with mixed or partial gonadal dysgenesis. J Pediatr Adolesc Gynecol 2007 Dec;20(6):333-338.
12. Laggari V, Christogiorgos S, Deligeoroglou E, Tsiantis J, Creatsas G. [Uterovaginal agenesis and polycystic ovary syndrome: psychological disturbance in adolescence]. Psychiatriki 2012 Jul-Sep;23(3):203-211.
13. http://www.huffingtonpost.co.uk/2013/01/01/womb-transplant-woman-cou_n_2391934.html
14. Ozkan O, Akar ME, Ozkan O, Erdogan O, Hadimioglu N, Yilmaz M, et al. Preliminary results of the first human uterus transplantation from a multiorgan donor. Fertil Steril 2013 Feb;99(2):470-476.
15. Hansen A. Swedish surgeons report world’s first uterus transplantations from mother to daughter. BMJ 2012;345:e6357.
16. Brosens I, Ghaem-Maghami S, Pijnenborg R. Uterus transplantation in the human: a complex surgical, medical and ethical challenge. Hum Reprod 2013 Feb;28(2):292-293.
|