|
Abstract
The risk of thrombosis is high in patients with essential thrombocythemia. Special precaution needed for those patients who will undergo Coronary artery bypass grafting. We are reporting a 62 years old patient with ischemic heart disease who was found to have essential thrombocythemia. This report explains the preoperative management and the postoperative risks anticipated due to the treatment.
Keywords: Coronary Artery Bypass Grafting; Essential Thrombocythemia; Hydroxyurea; Case Report.
Introduction
Essential Thrombocythemia (ET) is a nonreactive, chronic myeloproliferative disorder characterized by a sustained elevation of platelet number with a tendency for thrombosis and hemorrhage.1 Platelet-mediated arterial, venous occlusive thromboses and bleeding represent the major causes of postoperative mortality associated with ET that can also induce severe neurological, cardiac or peripheral vessels complications.1-7 The management is difficult because there is no definite guidelines available in the literature discussing this issue.2 For the moment, there are several reports about preoperative treatment with aspirin, warfarin, melfalan, hydroxyurea, low-molecular heparin, interferon therapy and thrombocytapheresis, followed by coronary artery bypass grafting (CABG).2-7
Case report
A 62-year old male with stable angina who was presented to Sultan Qaboos University Hospital complaining of central chest pain radiating to the left shoulder that occurred with exertion and was relieved by rest. The chest pain had started approximately half a year ago. He denied any palpitation, syncope or sweating. The case was known for ET, and the patient had been taking acetylsalicylic acid for the prevention of cardiovascular thromboses. He had a history of urinary tract infection and urinary obstructive symptoms, which had been treated adequately.
Age, gender and ET were the only known risk factors for coronary artery disease in this patient. The physical examination on the whole was non-remarkable. The coronary angiography (CAG) showed a normal left main trunk and triple vessels disease. In the ventriculography, the basal and inferior segments appeared akinetic. The echocardiography showed moderate hypokinesis of the posterior wall and mild mitral regurgitation with an ejection fraction of 58%. The electrocardiography did not reveal any ischemic changes. The ultrasound of the abdomen showed splenomegaly and a moderately enlarged prostate gland, but no ascitis or hydronephrosis.
In a routine preoperative work-up, the only pathological changes that could be found were an increased level of white blood cell count (WBC) 19, and a platelet count of 1020 × 10(9)/L. Further testing revealed a positive result for JAK2V617F mutations, which was strongly suggestive of ET as one of the three myeloproliferative disorders. The elimination of possible chronic myeloid leukemia was achieved by determining the absence of BCR/ABL transcripts in the peripheral blood. In addition to this, the patient was glucose-6-phosphate dehydrogenase (G6PD) deficient, which is a quite frequent event among the local population.
Based on the clinical presentation, general examination and CAG findings, elective coronary artery bypass surgery was indicated. At this stage, it was difficult to assess adequately the risk for surgery. The hematology team was involved, and a method of cytoreduction was the chosen pretreatment with Hydroxyurea (HU) 500 mg two times daily for one week. However, this was suboptimal and needed to be increased to 1000 mg two times daily for another week. The platelet count gradually came down to 459 × 10(9)/ L and the patient underwent CABG, grafting left anterior descending artery, intermediate artery and posterior descending artery using internal mammary artery and vein conduits consequently.
After the uneventful surgery, the patient had excessive non-surgical bleeding by a total of 2.5 L in the first 16 hours with the absence of clot formation, a subnormal coagulation screen of 12.6 sec prothrombin time, 42.1 sec activated partial thromboplastin time and international normalized ratio (INR) of 1.13. During that period of time, the patient received different blood components such as; 6 units of packed red blood cells, 8 units of fresh frozen plasma, 8 units of platelets, and 6 units of cryoprecipitate. The patient was extubated after 14 hours postoperatively, the bleeding gradually stopped and the chest tubes were removed on day 2 after the operation. Postoperatively, the patient developed acute thrombocytopenia and neutropenia. (Figs. 1, 2)
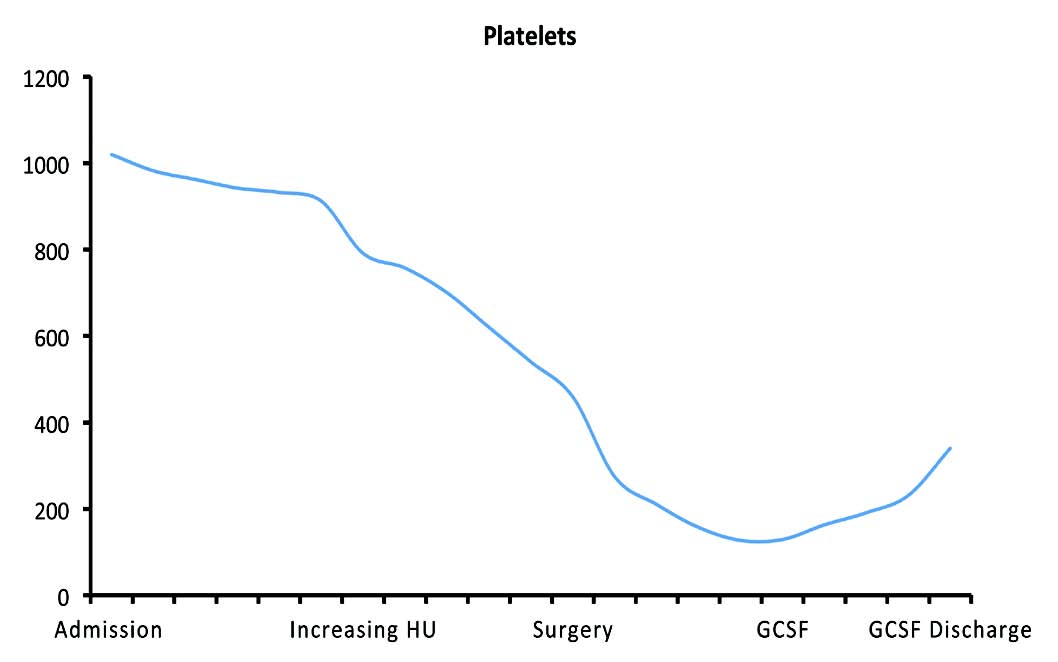
Figure 1: Platelets count from admission till discharge. (HU: Hydroxyurea. GCSF: granulocyte colony-stimulating factor)
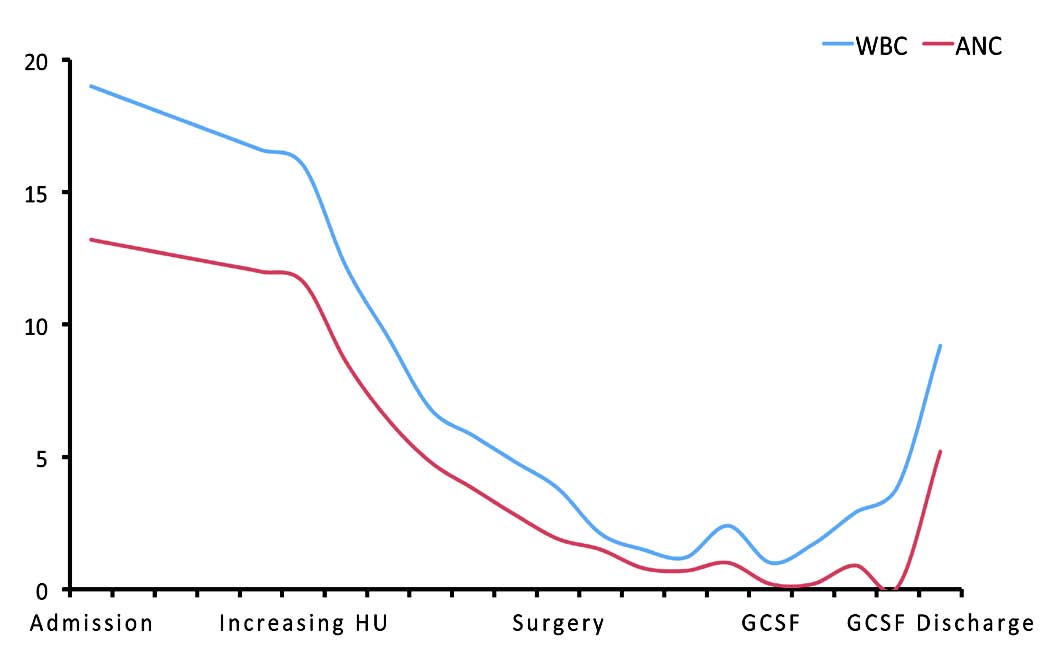
Figure 2: Drop in the White Blood Cell (WBC), Absolute Neutrophil Count (ANC) and the Recovery after GCSF was given.
The patient received two single doses of granulocyte colony-stimulating factor (GCSF) analog at an interval of 3 days to stimulate the proliferation and differentiation of granulocytes. Also, an empiric broad-spectrum antibiotic was given to prevent opportunistic infections until bone marrow function returned to normal. After eight days of therapy, the patient was discharged from the hospital. He was discharged on Aspirin and to be followed in Hematology clinic if he will need to be put back on Hydroxyurea or not.
Discussion
Coagulation and platelet activation have turned out to be tightly integrated processes. Decreasing the platelet count or functionality is one of the goals in preparation for open-heart surgery on patients with ET. However, determining the method of cytoreduction is a challenge, as it is important to achieve a balance between such dangerous postoperative complications as vascular thrombosis and excessive hemorrhage. With this in mind, previously, a variety of medications and procedures has been used.2-7 Hydroxyurea emerged as the preferred platelet-lowering agent in high risk ET patients and is presently the drug of choice as it is safe, low cost and available. Complete preparation of the patient in our case took about two weeks.
The dose adjustment and timing of ‘readiness’ for surgery was decided according to the laboratory results. We believe that one of the optimal managements would be to reduce the platelet count gradually until a platelet count is 1.5 times the upper level of normal, which was achieved under the meticulous supervision of a hematologist. Postoperatively, we faced the problem of lowering white blood cells (WBC), mainly neutrophil subtype where administration of GCSF effectively increased the number of leucocytes in the blood. In view of the low WBC and recent surgery, a short course of oral antibiotic prophylaxis was prescribed (Figs. 1, 2). Since this group of patients has a high risk of bleeding, we also recommend using blood salvage devices, such as the cell saver that might reduce transfusion requirements.
Conclusion
Essential thrombocythemia, although rare, is an ominous comorbidity for coronary artery bypass surgery with an unpredictable prognosis. It is necessary to implement perfect perioperative management to make sure that the result of surgery is excellent. Hydroxyurea is the drug of choice to achieve effective cytoreduction in patients with symptoms of ET – who are intended to undergo cardiac surgery. A multidisciplinary approach is warranted to act on the prevention of the postoperative complications.
Acknowledgements
The author reported no conflict of interest and no funding was received for this work.
References
1. Brière JB. Essential thrombocythemia. Orphanet J Rare Dis 2007;2:3.
2. Schölzel BE, Endeman H, Dewilde W, Yilmaz A, de Weerdt O, Ten Berg JM. Cardiac surgery in a patient with essential thrombocythemia: a case report. Neth Heart J 2010 Aug;18(7-8):378-380.
3. Das SS, Bose S, Chatterjee S, Parida AK, Pradhan SK. Thrombocytapheresis: managing essential thrombocythemia in a surgical patient. Ann Thorac Surg 2011 Jul;92(1):e5-e6. .
4. Kohno K, Takeuchi Y, Gomi A, Nakatani H, Yamanaka J. [A case report of aorto-coronary artery bypass surgery in patient with essential thrombocythemia]. Nihon Kyobu Geka Gakkai Zasshi 1997 Jan;45(1):55-58. Jpn J Thorac Cardiovasc Surg.
5. Momiyama T, Hiranaka T, Nomura F, Tominaga H, Nishioka T. Coronary artery bypass grafting for left main trunk coronary artery lesion associated with essential thrombocythemia. Clin Cardiol 1993 Sep;16(9):691-693.
6. Iemura J, Sato T, Yamada T, Ando F. [A case report: coronary artery bypass grafting for the patient with essential thrombocythemia]. Nihon Kyobu Geka Gakkai Zasshi 1991 Aug;39(8):1237-1241. Jpn J Thorac Cardiovasc Surg.
7. Ohto T, Shihara H, Miyauchi Y, Nakajima N. [A case of coronary artery bypass surgery using left internal thoracic artery and right gastroepiploic artery for a patient with essential thrombocythemia]. Jpn J Thorac Cardiovasc Surg 1998 Aug;46(8):767-771.
|