|
Abstract
Delayed herniation of the abdominal contents through a congenital diaphragmatic hernia may occur beyond the neonatal period. This report describes a 9-week-old female baby who presented with excessive crying, irritability and respiratory distress secondary to late presentation of left-sided congenital diaphragmatic hernia. The chest radiograph showed tension gastrothorax. She underwent surgical reduction of the hernia. She made an excellent recovery and was discharged a few days after the operation. It is assumed that sudden increase of the intra-abdominal pressure caused herniation of abdominal content through a pre-existing diaphragmatic defect. This report aims to increase the awareness of this condition among physicians and pediatric surgeons to allow early diagnosis and management.
Keywords: Late presentation of diaphragmatic hernia; Respiratory distress; Gastrothorax; Chest radiograph.
Introduction
Children with congenital diaphragmatic hernia (CDH) commonly present in the neonatal period with respiratory distress. Late-presenting CDH is less common and the majority present with non-specific gastrointestinal or respiratory symptoms later in childhood. Delayed herniation of the abdominal contents through a congenital diaphragmatic hernia may occur beyond the neonatal period.1 The first case was reported by Kirkland in 1959.2 CDH with mediastinal shift by hernial contents beyond the neonatal period is a rare but potentially life threatening emergency.3-5 For these reasons, late-presenting CDH is quite frequently misdiagnosed. The purpose of this report is to familiarize pediatricians and pediatric surgeons with the clinical presentations that can occur in children with CDH, in order to facilitate early management of this potentially life-threatening condition. Surgical correction has excellent outcome. The prompt diagnosis of late presentation of CDH will reduce morbidities and mortalities.
Case Report
A previously healthy 9-week-old female baby presented to the hospital with acute onset of breathlessness, grunting, irritability and excessive crying of 3 hours duration. Gestational history was unremarkable with birth weight of 3460 grams and normal Apgar scores. She was discharged after 24 hours and remained well at home. There was no history of trauma or fall from height.
On examination, she was afebrile but in severe respiratory distress, tachycardic and poorly perfused. She has moderate subcostal and intercostal recession. Air entry was reduced on the left side of the chest and heart sounds were muffled. She required fluid resuscitation with intravenous 0.9% normal saline. Chest radiograph showed a massive gastrothorax on the left side with mediastinal shift to the right side and complete collapse of the left lung (Fig. 1). She was admitted in the pediatric intensive care unit and required intubation and mechanical ventilation. She was taken for emergency surgical correction.
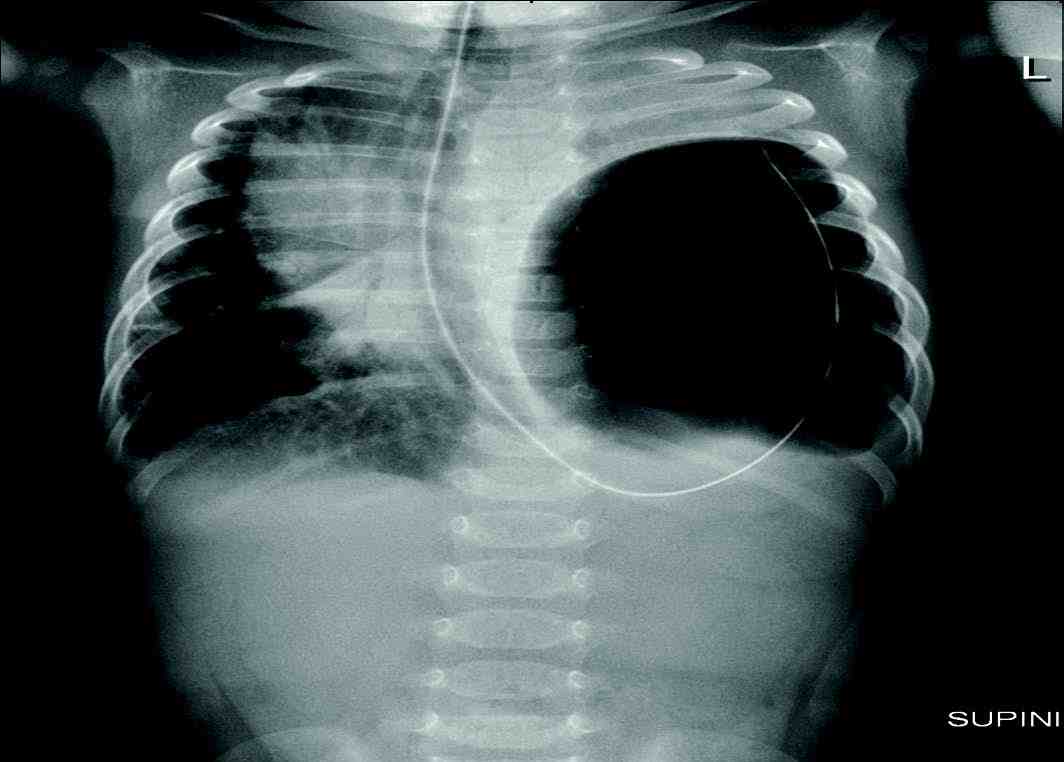
Figure 1: Pre-operative image showing gastro thorax with coiled nasogastric tube on the left side of the chest.
There was a 2 cm postro-lateral defect in the left diaphragmatic dome with whole of the stomach, transverse colon, and spleen in the left hemi-thorax that was reduced. The left lung was seen well expanded after reduction and the diaphragm was repaired. The baby remained well and extubated immediately after the surgery. Postoperative chest radiograph showed full expansion of the left lung (Fig. 2). The baby made full recovery, and two months later, the baby was followed-up again and was asymptomatic and healthy, with normal growth and developmental parameters.
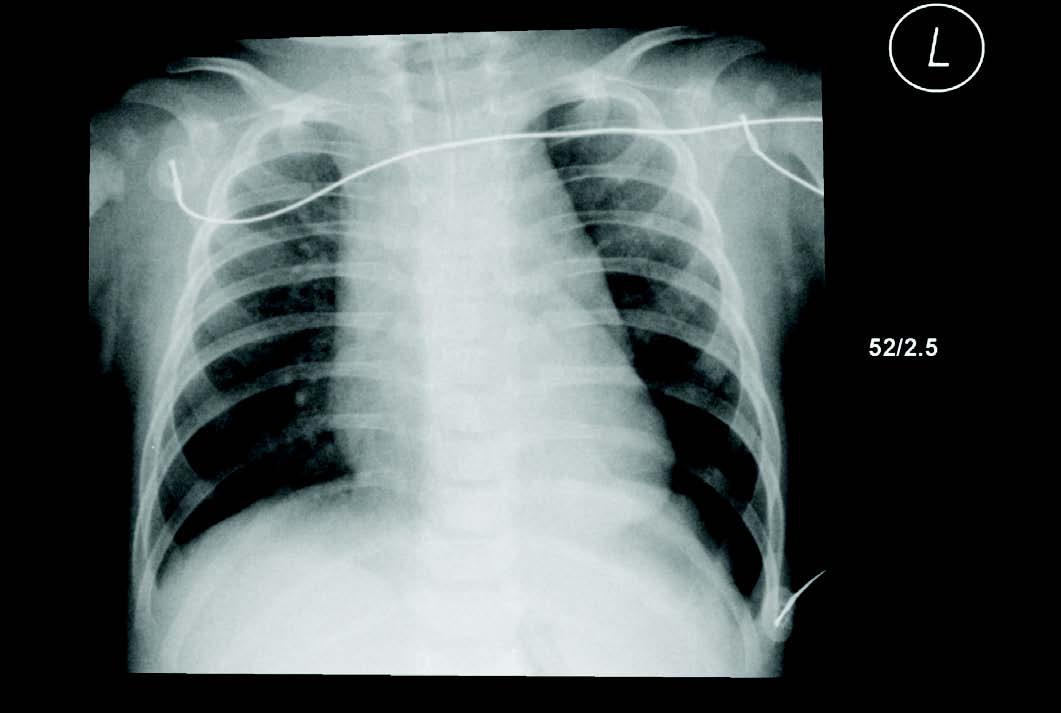
Figure 2: Resolution of gastrothorax with normal lung fields.
Discussion
The occurrence of late-presenting CDH was estimated to be 10% to 13% of all CDH cases.6,7 In 349 late-presenting CDH children recently reviewed, the male-to-female ratio was close to 2:1.4 Among late-presenting CDH cases, unilateral postero-lateral defects constituted more than 96%, with 79.4% and 20.6% left and right-sided hernias, respectively. Eighty percent of cases of delayed onset diaphragmatic hernia present with acute symptoms.4 As most of the cases presenting late do not have associated anomalies, the etio-pathology of diaphragmatic defect is less likely to be similar to the usual congenital diaphragmatic hernia.4,8 Another feature in these cases is the rarity of associated lung hypoplasia.6 Some of the cases presenting late may have acquired the defect secondary to Group B Streptococcus pneumoniae that causes diaphragmatic necrosis.9,10
The presentation of late onset diaphragmatic defect is often intriguing. It can be acute or chronic, the latter more commonly seen in right-sided pathology. It is presumed that the right-sided lesions present late as the solid organ-liver offers some resistance to displacement of abdominal contents into the thorax. Gastrointestinal symptoms predominate in right-sided lesions and in chronic herniation on either side, while acute herniation produces respiratory symptoms. Respiratory symptoms are also more common in younger patients. As none of the symptoms are specific for diaphragmatic hernia presenting late, this diagnosis should not be excluded from differential diagnosis in an affected child.4,8 A correct diagnosis should be arrived at expeditiously, as unnecessary thoracocentesis and other procedures have been done.3,11,12
In our patient, the initial presentation suggested a cardiac origin with irritability, tachycardia, tachypnea and muffled heart sounds, but the chest radiograph with the NGT coiled in the displaced stomach within the left chest clinched the diagnosis. The NGT was also very useful in decompressing the distended gastrothorax and is in fact the recommended intervention to relieve the respiratory distress. Other imaging modalities like ultrasound, CT scan, MRI chest and upper or lower GI contrast studies etc., have all been used in selected cases; it is necessary to have a high degree of suspicion to avoid unnecessary delays in diagnosis.13
Diaphragmatic hernia presenting at birth and those presenting in infancy or childhood have widely varying prognosis, with nearly all late presentation diaphragmatic hernia running a benign course.1,6 In a case series of ten neonates diagnosed radiologically with pneumothoraces, congenital diaphragmatic hernia was the primary etiology in 10% of them.14
Conclusion
This case highlights the importance of early diagnosis of the late presentation of congenital diaphragmatic hernia. It emphasizes the importance of sound physical examination, correct interpretation of imaging as surgical correction is lifesaving and curative. All pediatricians and pediatric surgeons should be aware of this condition in their routine practice.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work. They thank the patient and her family for their cooperation and for giving their consent for publishing this report. They also thank all health professionals involved in the care of this patient.
References
1. Elhalaby EA, Abo Sikeena MH. Delayed presentation of congenital diaphragmatic hernia. Pediatr Surg Int 2002 Sep;18(5-6):480-485.
2. Krikland J. congenital postero-lateral diaphragmatic hernia in the adult. Br J Surg 1957;47:16-22 .
3. Berman L, Stringer D, Ein SH, Shandling B. The late-presenting pediatric Bochdalek hernia: a 20-year review. J Pediatr Surg 1988 Aug;23(8):735-739.
4. Bagłaj M. Late-presenting congenital diaphragmatic hernia in children: a clinical spectrum. Pediatr Surg Int 2004 Sep;20(9):658-669.
5. Bagłaj M, Dorobisz U. Late-presenting congenital diaphragmatic hernia in children: a literature review. Pediatr Radiol 2005 May;35(5):478-488.
6. Butler MW, Stolar CJ, Altman RP. Contemporary management of congenital diaphragmatic hernia. World J Surg 1993 May-Jun;17(3):350-355.
7. Weinstein S, Stolar CJ. Newborn surgical emergencies. Congenital diaphragmatic hernia and extracorporeal membrane oxygenation. Pediatr Clin North Am 1993 Dec;40(6):1315-1333.
8. Tibboel D, Gaag AV. Etiologic and genetic factors in congenital diaphragmatic hernia. Clin Perinatol 1996 Dec;23(4):689-699. J.
9. Suresh BR, Rios A, Brion LP, Weinberg G, Kresch MJ. Delayed onset right-sided diaphragmatic hernia secondary to group B streptococcal infection. Pediatr Infect Dis J 1991 Feb;10(2):166-168.
10. Manzar S, Nair PM, Nayar M. Delayed presentation of congenital diaphragmatic hernia in association with group B streptococcus infection in a preterm Omani neonate. Saudi Med J 2000 May;21(5):487-489.
11. Fein JA, Loiselle J, Eberlein S, Wiley JF, Bell LM. Diaphragmatic hernia masquerading as pneumothorax in two toddlers. Ann Emerg Med 1993 Jul;22(7):1221-1224.
12. Coren ME, Rosenthal M, Bush A. Congenital diaphragmatic hernia misdiagnosed as tension pneumothorax. Pediatr Pulmonol 1997 Aug;24(2):119-121.
13. Oh KS, Newman B, Bender TM, Bowen A. Radiologic evaluation of the diaphragm. Radiol Clin North Am 1988 Mar;26(2):355-364.
14. Ali R, Ahmed S, Qadir M, Maheshwari P, Khan R. Pneumothoraces in a neonatal tertiary care unit: case series. Oman Med J 2013 Jan;28(1):67-69.
|