|
Abstract
Objective: To identify patients’ attitudes, preferences and comfort levels regarding the presence and involvement of medical students during consultations and examinations.
Methods: A cross-sectional descriptive study was conducted from September 2011 to December 2011 at King Abdulaziz University Hospital in Jeddah, Saudi Arabia. Participants were randomly selected from the outpatient and inpatient clinics at the Department of Obstetrics and Gynecology and the Emergency Department, provided they were admitted for obstetric or gynecology-related conditions. Data were collected using a structured questionnaire, and data analysis was performed using the Statistical Package for Social Sciences.
Results: Of the 327 patients who were recruited, 272 (83%) were elective patients who were seen at the outpatient and inpatient clinics of the Department of Obstetrics and Gynecology (group I). The other 55 (16.8%) were seen at the Emergency Department or the Labor and Delivery Ward (group II). One hundred seventy-nine participants (160 [58.8%] in group I and 19 [34.5%] in group II) reported positive attitudes about the presence of female medical students during consultations. Fewer participants (115 [42.3%] were in group I and 17 [30.9%] in group II) reported positive attitudes regarding the presence of male medical students during consultations (p=0.095). The gender of the medical student was the primary factor that influenced patients’ decision to accept or decline medical student involvement. No significant associations were observed between patients’ attitudes and perceptions toward medical students and the patients' age, educational level, nationality or the gender of the consultant.
Conclusion: Obstetrics and Gynecology patients are typically accepting of female medical student involvement during examinations. Student gender is the primary factor that influences patient attitudes regarding student involvement during physical examinations.
Keywords: Medical student; OB-GYN patients; Saudi Arabia.
Introduction
Contact with patients is an important component for students in medical education. In addition to promoting contextual and clinical learning, contact with patients improves communication and professional skills.1,2 However, gaining experience with patients requires that patients to be willing to participate in the education and training of medical students. In the modern era, patient’s rights and informed consent have gained greater visibility, and patients now have the right to choose whether to have medical students present during consultations, a fact that can make it difficult to train students when patients decline to participate.
Studies of patients’ attitudes towards the presence of medical students in Obstetrics and Gynecology clinics have shown that patients are generally accepting of medical student involvement, with acceptance rates ranging between 79% and 89.1%.3-6 It has also been reported that patients with greater experience with medical students are more willing to favor medical student involvement than those with less previous contact.4,7,8
Male students have been reported to be more likely to experience gender bias from patients in Obstetrics and Gynecology clinics.9 In contexts in which most patients are Muslim, this type of bias is more likely to be serious. One report from the United Arab Emirates found that women generally refuse to be examined by male students for abdominal and gynecological problems.10 In Saudi Arabia, an Islamic theocratic monarchy whose official religion is Islam, cultural and religious issues might also affect the attitudes of patients in Obstetrics and Gynecology clinics toward male medical students. In addition, as women increasingly populate the field of Obstetrics and Gynecology, the need for obstetrics and gynecology faculty members to prevent gender differences in the quality of training during obstetrics and gynecology clerkships will likely increase.
Patients attending Obstetrics and Gynecology clinics are vulnerable, as they are frequently required to reveal personal information, including their sexual history. In addition, it might be stressful for some patients to have genital examinations in the presence of a medical student. Patients at Obstetrics and Gynecology clinics were surveyed to ascertain their attitudes towards the role of medical students, their preferences regarding medical student involvement and their comfort level with the presence of medical students during consultations and examinations.
Methods
A cross-sectional descriptive study was conducted from September 2011 to December 2011 at King Abdulaziz University Hospital in Jeddah, Saudi Arabia. Participants were selected from the outpatient and inpatient clinics in the Department of Obstetrics and Gynecology and the Emergency Department, provided that they were admitted for obstetric or gynecology-related conditions. The research team selected the patients by systematic random sample of every third patient. The third number was chosen randomly. The working days for hospital admission were Sunday and Thursday. Patients who refused or were unable to communicate because of language barriers and those in critical conditions were excluded from the study.
Patients were informed that their participation would not affect the quality of care provided and that they had the right to decline to participate in the interview. The interviewers also informed them that the information that was obtained from the structured questionnaires would be kept confidential. All participants were given the opportunity to ask additional questions. Consent was obtained from all participants prior to their inclusion in the study, which was approved by the Biomedical Ethics Research Committee of King Abdulaziz University.
The questionnaire, which was prepared in English, consisted of short, clear, open-ended questions. The validity of its content was confirmed through an extensive literature review and by experts with specializations in gynecology, community medicine and medical education (the basic survey that was used was done by Hartz et al).4 Interviewers were house officers who were rotating in the Department of Obstetrics and Gynecology. The interviewers were available to answer any query raised by a participant based on their ability to find the necessary information.
The sample size was calculated to require a minimum of 10 participants per question. To the authors’ knowledge, this is the first study done in Saudi Arabia, making the estimation of sample size difficult. However, the research team aimed to include more than 300 patients. Items were designed to collect basic demographic data, prior experiences with medical students, patient attitudes towards medical students and any other important factors that could potentially influence their decision to allow or refuse medical student participation in their care. To ensure content validity, the questionnaire was discussed in a focus group of five Obstetric and Gynecology consultants. Some questions were modified. To ensure face validity, a pilot study was done among 20 patients. The results of the analysis were not included in the study. The reliability was calculated using Cronbach’s alpha which was equal to 0.74. A positive attitude was defined by allowing students to attend consultation, as in the community where there are lots of social and culture limitations.
The study population was divided into two groups. Group I consisted of patients from the outpatient clinic or inpatient ward of the Department of Obstetrics and Gynecology, and group II consisted of patients who were admitted to the Emergency Department or the Labor and Delivery Ward. The data were entered and analyzed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA), version 17.0. Descriptive analyses were conducted by calculating the means and proportions for continuous and discrete data, respectively, and associations were tested using Chi squared tests to compare outcome variables between the two groups.
Results
Out of the 400 patients who were approached to participate in the survey, 327 were interviewed. The overall survey response rate was 81.8%; 272 of the respondents (83.2%) were in group I, and the other 55 (16.9%) participants were in group II. The mean age of the participants was 32.6 years (range: 17-83 years) and 284 (86%) were married. Regarding the education status of the study participants, 27 (8.2%) were illiterate, 90 (27.4%) completed high school and 63 (19%) had postgraduate degrees.
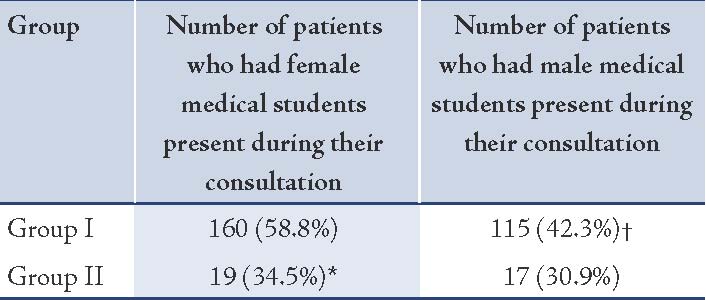
One hundred seventy-nine participants (54.7%) reported a positive attitude regarding the presence of female medical students during consultations. Of these, 160 (58.8%) were in group I and 19 (34.5%) were in group II (p=0.0025). Fewer participants (n=132; 40.3%) reported positive attitudes regarding the presence of male medical students during consultations. Of these, 115 (42.3%) were in group I and 17 (30.9%) were in group II (p=0.095). (Table 1)
Table 1: Participants with a history of positive experiences with medical students.
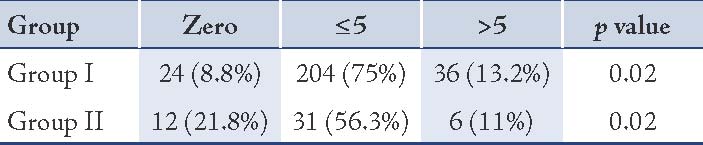
A total of 36 participants (11.0%) declined to have a medical student present during their consultation, and 204 participants (75%) in group I and 31 (56%) in group II indicated that they would only permit the presence of fewer than five medical students during their consultation (Table 2). Less than half of the participants in group I (n=128; 47%) and more than half of the participants in group II (n=28; 50.9%) responded that they would not mind having female medical students present during consultations.
Table 2: Number of medical students with which patients would feel comfortable during a consultation.*
Forty-eight participants (17.6%) in group I and 15 (27%) in-group II felt that it was either unnecessary or extremely unnecessary to have female medical students present during consultations (p=0.03). However, 88 participants (32.3%) in group I and 22 (40.0%) in group II indicated that they did not mind having male students present during consultation. However, no significant differences were observed between the two groups regarding the necessity of male medical students being present during consultations, (p=0.194). (Table 3)
Table 3: Participants’ attitudes toward the presence of female and male medical students during their consultations.*
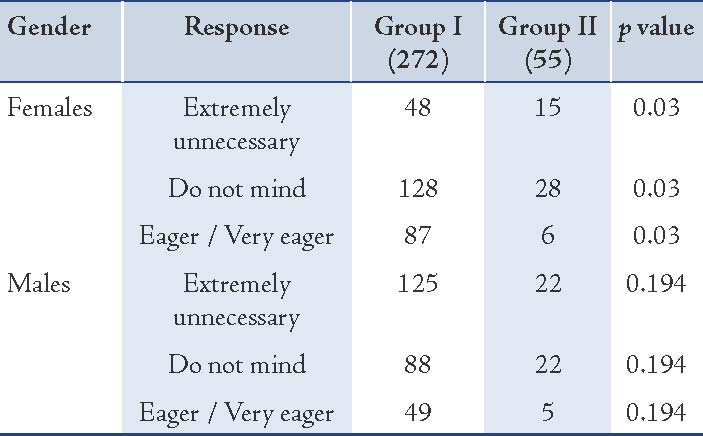
Table 4: Reasons for accepting or declining the involvement of medical students during examinations.*
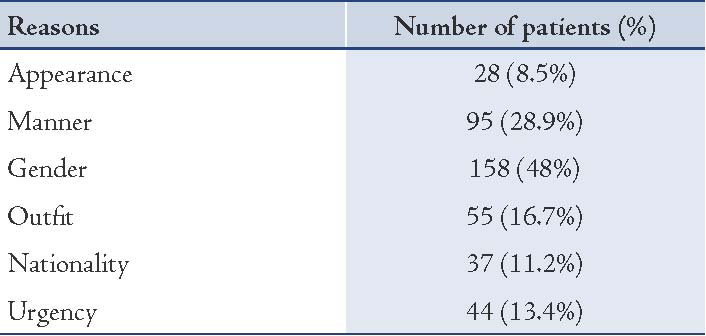
Religious beliefs were cited as the most common primary reason that influenced patients’ opinions regarding the presence of medical students during consultations (n=138; 42.2%). The personality (n=120; 36.7%) and cultural beliefs (n=84; 25.6%) of the participant were also important factors. Most participants (n=158; 48%) reported that medical student gender was the main reason for their decision regarding medical student involvement. The nationality and appearance of medical students were the deciding factors for 28 (8.5%) and 37 participants (11%), respectively. (Table 4)
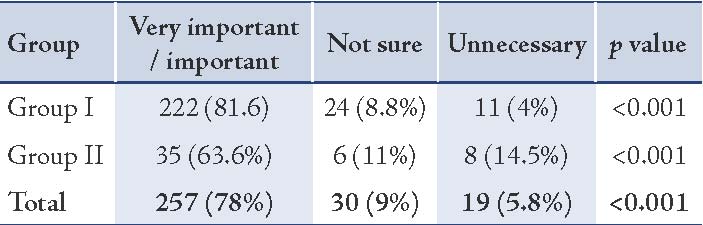
Most participants (n=227; 83.4%) in group I responded that it was very important to have medical students present during consultations; only 11 participants (3.5%) thought it was unnecessary in emergency situations (p=0.21). Similarly, 257 participants (78.5%) recognized the importance of hands-on patient contact for medical students to learn physical examination skills; whereas, only 19 (5.8%) felt that hands-on patient contact was unnecessary (Table 5). Multivariate analysis revealed no significant associations between patients’ attitudes towards medical students and patient age, educational levels, nationality or the consultant’s gender.
Table 5: Participants’ perceptions of the importance of hands-on training for medical students.
Discussion
This study demonstrated that most patients are accepting of having medical students present during consultations in obstetrical and gynecological settings. This finding is consistent with previous studies.3,4,11 In particular, one study from Riyadh, Saudi Arabia concluded that most women would accept the participation of medical students in their care.12 Similar to several other reports,8,13 no associations between the age of patients and their acceptance of medical student involvement were noted in this study. In contrast, Shan et al. reported that younger women with no children were less likely to permit a student of either gender to take their history or observe their examination.14
Finding of an association between patients’ previous contact with medical students and the willingness of patients to allow medical student involvement is consistent with previous reports that patients with more previous visits involving medical student participation were more willing to accept medical student involvement and would feel more comfortable with the presence of a medical student during clinical situations.4,7,8
In the present study, a negative association between patient acceptance and the extent of involvement of medical students in the physical examination, particularly during pelvic exams was identified. In general, the gender of medical students was the most important factor cited by participants in this survey, and female medical students were preferred over male medical students. Other authors have reported similar findings.9,15
Contrary to the findings of Abdulghani et al.12 who reported that most patients (81%) indicated that the general appearance and manner of students influenced their cooperation, only 16.7% of the participants in this study reported that the appearance of medical students had an effect on their attitudes. Regardless of patients’ perceptions of medical students, the participants believed that hands-on patient contact and observations of physician-patient interactions were crucial for the training of medical students.
The members of Obstetrics and Gynecology Departments need to be sensitive to subtle forms of gender bias and should ensure equal training for medical students. This study reveals a need to have alternative methods of teaching Obstetrics and Gynecology in the community, especially for male medical students.
Conclusion
Women who attend the Obstetrics and Gynecology Service of King Abdulaziz University Hospital are generally accepting of the presence of medical students during consultations. However, the student’s gender is the primary factor that was cited as the reason for accepting or refusing to allow medical student participation during physical examinations.
Acknowledgments
The authors would like to express their sincere thanks to Scientific Chair of Professor Abdullah Hussain Basalamah of Gynecological Cancer. The authors would also like to express their great appreciation to all of the participants (OB-GYN patients) in this study. The authors report no conflicts of interest.
References
1. Spencer J, Blackmore D, Heard S, McCrorie P, McHaffie D, Scherpbier A, et al. Patient-oriented learning: a review of the role of the patient in the education of medical students. Med Educ 2000 Oct;34(10):851-857.
2. British Medical Association, Medical Education Subcommittee. Role of the patient in medical education. British Medical Association 2008.
3. Ching SL, Gates EA, Robertson PA. Factors influencing obstetric and gynecologic patients’ decisions toward medical student involvement in the outpatient setting. Am J Obstet Gynecol 2000 Jun;182(6):1429-1432.
4. Hartz MB, Beal JR. Patients’ attitudes and comfort levels regarding medical students’ involvement in obstetrics-gynecology outpatient clinics. Acad Med 2000 Oct;75(10):1010-1014.
5. Rizk DE, Al-Shebah A, El-Zubeir MA, Thomas LB, Hassan MY, Ezimokhai M. Women’s perceptions of and experiences with medical student involvement in outpatient obstetric and gynecologic care in the United Arab Emirates. Am J Obstet Gynecol 2002 Oct;187(4):1091-1100.
6. Berry RE Jr, O’dell K, Meyer BA, Purwono U. Obtaining patient permission for student participation in obstetric-gynecologic outpatient visits: a randomized controlled trial. Am J Obstet Gynecol 2003 Sep;189(3):634-638.
7. Magrane D, Gannon J, Miller CT. Obstetric patients who select and those who refuse medical students’ participation in their care. Acad Med 1994 Dec;69(12):1004-1006.
8. Adams DS, Adams LJ, Anderson RJ. The effect of patients’ race on their attitudes toward medical students’ participation in ambulatory care visits. Acad Med 1999 Dec;74(12):1323-1326.
9. Chang JC, Odrobina MR, McIntyre-Seltman K. The effect of student gender on the obstetrics and gynecology clerkship experience. J Womens Health (Larchmt) 2010 Jan;19(1):87-92.
10. McLean M, Al Ahbabi S, Al Ameri M, Al Mansoori M, Al Yahyaei F, Bernsen R. Muslim women and medical students in the clinical encounter. Med Educ 2010 Mar;44(3):306-315.
11. Choudhury TR, Moosa AA, Cushing A, Bestwick J. Patients’ attitudes towards the presence of medical students during consultations. Med Teach 2006 Nov;28(7):e198-e203.
12. Abdulghani HM, Al-Rukban MO, Ahmad SS. Patient attitudes towards medical students in Riyadh, Saudi Arabia. Educ Health (Abingdon) 2008 Jul;21(2):69.
13. Witte FM, Stratton TD, Nora LM. Stories from the field: students’ descriptions of gender discrimination and sexual harassment during medical school. Acad Med 2006 Jul;81(7):648-654.
14. Shann S, Wilson JD. Patients’ attitudes to the presence of medical students in a genitourinary medicine clinic: a cross sectional survey. Sex Transm Infect 2006 Feb;82(1):52-54.
15. Stratton TD, McLaughlin MA, Witte FM, Fosson SE, Nora LM. Does students’ exposure to gender discrimination and sexual harassment in medical school affect specialty choice and residency program selection? Acad Med 2005 Apr;80(4):400-408.
|