Torsion of Appendix Epiploica: A Rare Cause of Acute Right Iliac Fossa Pain
Ganapathy Iyer, 1 Vuthaluru Seenu,1 Akhil Bhat,1 MC Sharma,2 Rebecca Mathew,2 GPN Verma2
Iyer G, et al. OMJ. 25 (2010); doi:10.5001/omj.2010.18
ABSTRACT
Acute appendicitis is the most common cause of right iliac fossa pain. However, if the appendix is normal at surgery, the surgeon has to search for other causes of acute abdominal pain including rare etiologies. Awareness of all causes of acute right iliac fossa pain and a high index of suspicion is essential for diagnosis of rare causes like torsion of appendix epiploica In addition, in some patients, two pathologies causing acute pain may coexist. It is to the authors’ knowledge that the simultaneous occurrence of torsion of appendix epiploica and acute appendicitis in a patient has not been previously reported, and is therefore discussed in this report.
From the 1Department of Surgery, Oman Medical College, Sultanate of Oman. 2Department of Surgery & Pathology, Sohar Hospital, Sultanate of Oman.
Received: 14 Oct 2009
Accepted: 01 Dec 2009
Address correspondence and reprint request to: Dr. Vuthaluru Seenu, Department of Surgery, Oman Medical College, Sultanate of Oman. Email: varnaseenu@hotmail.com
INTRODUCTION
Acute appendicitis is the most common cause of right iliac fossa pain. Other common causes of acute right iliac fossa pain include Meckel’s diverticulitis, pelvic inflammatory disease, twisted ovarian cysts, regional ileitis and ureteric calculous. Very rarely, it can also be caused by torsion of appendices epiploaecae.1-5 The simultaneous occurrence of torsion of appendix epiploica and acute appendicitis in a patient, as far as the authors are aware has not been previously reported. Preoperative diagnosis of torsion of appendix epiploica is extremely difficult and needs a very high index of suspicion. This is a report of torsion of appendix epiploica detected at operation in a patient who was also subsequently diagnosed to have acute appendicitis at histopathology.
CASE REPORT
A 21- year- old Omani male presented to the Accident and Emergency Department of Sohar Hospital, with a history of right iliac fossa pain of one day duration associated with nausea with no other gastrointestinal or urinary tract symptoms. The pain was of sudden onset, and was also severe, gripping, continuous and localized. The patient was nauseated but had no history of vomiting. He had no other gastrointestinal or urinary tract symptoms. On examination, the patient was comfortable, well built and his general condition was fair. His vitals were normal (Pulse: 99 beats/min, BP: 141/87mmHg, Temp: 37 c and RR: 20/min). Abdominal examination revealed tenderness in the right iliac fossa with rebound and guarding. The rest of the abdomen was soft with normal bowel sounds. Per rectal examination was normal. Examination of other systems was also normal. Laboratory investigations revealed normal haemoglobin and elevated leukocyte counts of 11.6 K/uL, polymorphonuclear leucocytosis were also observed. Ultrasonography of the abdomen showed no free fluid, and although the appendix was not visualised, the rest of abdominal organs were normal.
A diagnosis of acute appendicitis was made and the patient was taken up for emergency appendicectomy under general anaesthesia after obtaining informed consent. On opening the abdomen, one appendix epiploica over the ascending colon, close to the caecum was found to be twisted, infarcted and gangrenous. (Fig. 1)
The appendix was retrocaecal in location, kinked by adhesions but not found to be inflamed on gross examination. The diseased appendix epiploica was excised. As the operation was being performed through a McBurney’s incision and the appendix was kinked by adhesions, an appendicectomy was also performed. Both specimens were sent for histopathologic examination.
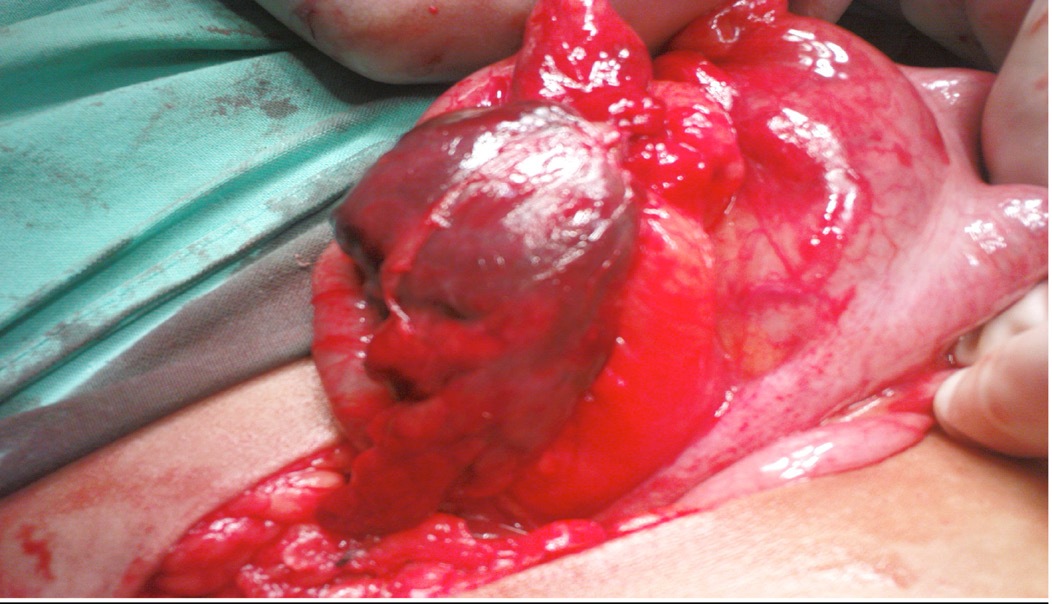
Figure 1: Operative photograph showing twisted and infarcted appendix epiploica. Arrrow pointing to taenia coli.
Post operative recovery was uneventful and the patient was discharged after four days. Histopathologic examination of the appendix epiploica revealed infarction of adipose tissue, congested blood vessels, areas of fresh haemorrhage and infiltration by foamy macrophages, (Fig. 2).
Sections from the appendix showed edema of the muscle coat and acute and chronic inflammatory cells infiltrate in the sub mucosa and muscle coat, (Fig. 3). There was no fibrinous exudate on the surface. A final diagnosis of acute appendicitis and infarction of the appendix epiploica was made.
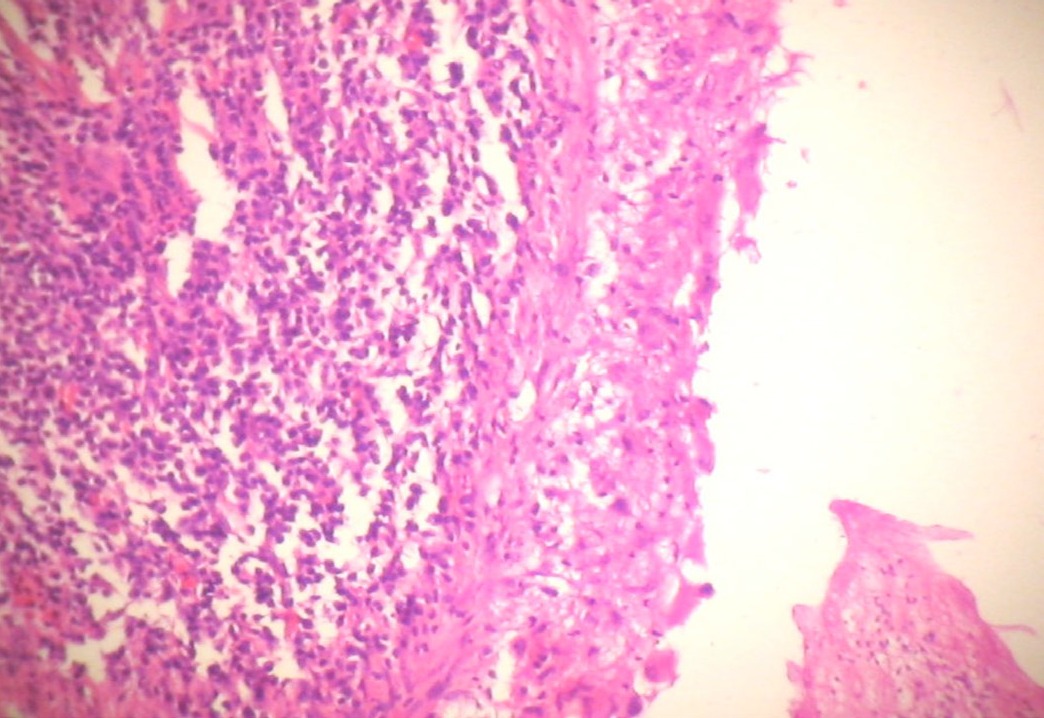
Figure 2: Photograph showing fresh haemorrhage and inflammatory exudates in adipose tissue suggestive of infarction.
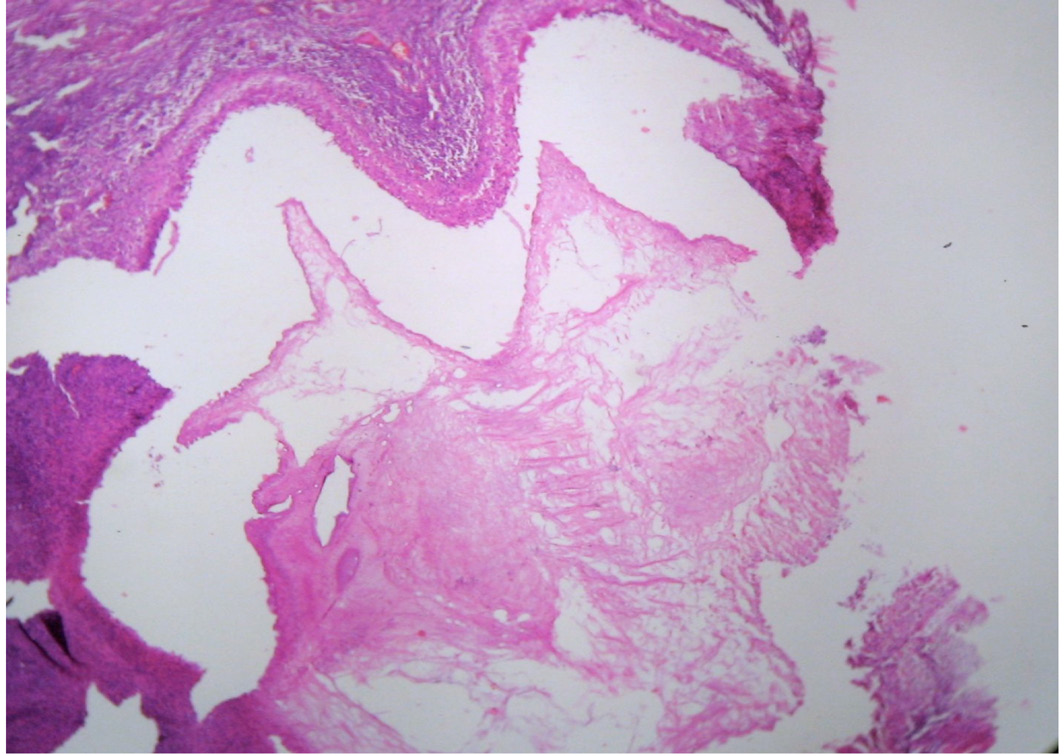
Figure 3: Photomicrograph showing acute and chronic inflammatory exudate in muscle coat reaching upto the serosa suggestive of acute appendicitis
Discussion
Epiploic appendages are small out-pouches filled with fat and small vessels (1 or 2 arterioles and venules) that are aligned along the serosal surface of the colon from the cecum to the recto-sigmoid junction.2 The distribution of the epiploicae is moderate on the ascending and descending colons and the greatest number usually appear on the transverse colon and sigmoid flexure.1 Their length varies from 0.5 to 5 cm. There are between 50-100 appendages lying in two rows parallel to the external surface of the three longitudinal muscle bands of the large intestine known as taenia coli.1,3 The exact function of appendices epiploicae is unknown. It has been suggested that they may have bacteriostatic properties, may serve as a protective cushion for blood vessels or may have a role in the absorptive actions of the large bowel.4
An appendix epiploica can undergo torsion (the most common complication) resulting in thrombosis, infarction, gangrene and abscess. The exact cause of torsion is unknown. It may develop as a consequence of sudden rotation of the body, or it may be due to a long pedicle, or the vein may be longer and may be more likely to twist around its accompanying artery, or it may be caused by excess fat in the pedicles.4 It can also cause intestinal obstruction by forming a band on the abdominal wall or an adjacent loop of bowel and thus kink the bowel; or a loop of small bowel may be caught under the adherent band, another possibility is that it may initiate an intussusceptions.4
There is no classical clinical picture of torsion of an appendix epiploica. It can occur at any age and there is no sex predilection. Pain is the most common complaint and may be acute or intermittent/ prolonged where the torsion untwists spontaneously and recurs again. The pain occurs in either the lower quadrant of the abdomen, but more frequently in the right iliac fossa, although the most common site of the lesion itself is the sigmoid colon.4 This could be explained by the fact that the sigmoid colon may be redundant and the top of the loop may be lying in the right iliac fossa. Clinical examination of the patient revealed localized tenderness with rebound and guarding. A palpable mass is rarely found. The white cell count is usually either normal or only mildly elevated.2.
Ultrasound findings include hyperechoic non-compressible pericolonic mass, frequently surrounded by a hypoechoic border.6,7 CT scan may show a hyper-attenuated ring with adjacent fat stranding or a lobulated fatty mass (due to two or more contiguous infarcted epiploic appendages lying in close proximity).7 However, preoperative diagnosis of torsion of appendix epiploica is extremely difficult and needs a very high index of suspicion.
The treatment of torsion of appendices epiploicae is surgical excision. This can be done laparoscopically,8-11 or through open approach.1-5 It may be prudent to perform appendicectomy, especially if a patient is operated through a McBurney or Lanz incision. Additionally, rarely can a patient have acute appendicitis in addition to torsion of appendix epiploica. Sometimes it may not be possible to diagnose acute appendicitis on gross examination in situ as in the studied case. In the patient under discussion, the occurrence of two pathologies can be attributed to the presence of adhesions around both sDiscussion
In conclusion, torsion of appendix epiploica is very rare and a preoperative diagnosis of torsion of appendix epiploica cannot be made with certainty. One must be aware of the entity so that it will not be missed at a laparotomy. A patient with torsion of the appendix epiploica can also have acute appendicitis. Hence, the appendix should always be examined at surgery. If a patient is operated through a right iliac fossa incision, it may be prudent to perform an appendicectomy, so as to avoid the confusion in future when the same patient presents with right iliac fossa pain at a later date.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Hunt VC, Torsion of appendices epiploicae. Ann Surg. 1919; 69:31-46.
2. Li A, Lau S, Loke TKL, Chan JCS. Primary epiploic appendagitis, HK Coll Radiol 2004; 7:81-83.
3. Sand M, Gelos M, Bechara FG, Sand D, Weiss TH, Steinstraesser L, et al. Epiploic appendagitis clinical characteristics of an uncommon surgical diagnosis, BMC SURG, 2007; 7:11.
4. Violago FC, Thorlakson RH. Torsion of the appendices epiploicae, Canad. Med. Ass. J, 1969, 100:274-82.
5. Hurreiz H, Madavo C. Torsion of an epiploic appendix mimicking acute appendicitis. The Internet J Surg. 2005; 6:2.
6. Danse EM, Van Beers BE, Baudrez V, Pauls C, Baudrez Y, Kartheus A, et al. Epiploic appendagitis: Color Doppler sonographic findings. Eur Radiol 2001; 11:183-186.
7. Barbier C, Denny P, Pradoura JM, Bui P, Rieger A, Bazin A, etal. Primary Epiploic Appendagitis: US, CT and MR Findings. J Radiol 1998; 79:1479-1485.
8. Chowbey P, Singh G, Sharma A, Khullar R, Soni V, Baijal M. Torsion of appendices epiploicae presenting as acute abdomen: laparoscopic diagnosis and therapy. Ind J Gastroenterol 2003; 22:68-69.
9. Bandyopadhyay SK, Jain M, Khanna S, Sen B, Tantia O. Torsion of the epiploic appendix: An unusual cause of acute abdomen. J Min Access Surg 2003; 3:70-72.
10. Dubose J, Jenkins D, Quayle C, Dress A, Cotlar A. Laparoscopic resection of infarcted appendices epiploicae of colon. Curr Surg 2005; 62:362-364.
11. Vazquez-Frias JA, Castaneda P, Valencia S, Cueto J. laparoscopic diagnosis and treatment of acute epiploic appendagitis with torsion and necrosis causing an acute abdomen. JSLS 2000; 4:247-250.