Stroke is a major complication after cardiac surgical procedures with a reported incidence of 1–5%.1 A variety of cardiac surgical procedures nowadays including coronary artery bypass grafting or valvular surgery are performed in elderly patients who are prone, in particular, to stroke and other complications. Patients with associated comorbidities like hypertension, heart rhythm abnormalities, and arteriosclerotic disease of the aorta also have a higher risk of developing stroke.2
Numerous methods have emerged as possible strategies for revascularization including intra-arterial thrombolysis and mechanical thrombectomy using different devices. These have variable success rates.3 The principal advantage of intra-arterial thrombolysis is the direct delivery of a highly concentrated thrombolytic drug in the vicinity of the thrombus with a lesser systemic distribution of the drug, while mechanical thrombectomy has the advantage of quick restoration of cerebral blood flow by clot extraction or clot fragmentation. Procedural related brain hemorrhage with variable incidence rates is a drawback for such neurointerventions.4
Our case depicts the valued importance of early recanalization using mechanical thrombectomy for ischemic stroke after cardiac surgery.
Case Report
A 52-year-old female was referred to the cardiology clinic at the Queen Alia Heart Institute, Jordan, with significant shortness of breath (New York Heart Association Class III-IV symptoms). Her coronary angiogram was normal, and the transthoracic echocardiogram (TTE) demonstrated severe rheumatic mitral valve stenosis, with moderate tricuspid valve regurgitation. The aortic valve was normal, and the left ventricular ejection fraction was preserved. The patient had a normal sinus rhythm and no history of atrial fibrillation. Transesophageal echocardiogram (TEE) confirmed these findings and did not demonstrate any clot in the heart chambers. Surgery was performed via median sternotomy and total cardiopulmonary bypass with bicaval snaring. Via a right atriotomy and transseptal approach, the rheumatic stenotic mitral valve leaflets were excised and a 29 mechanical bileaflet ST Jude valve (St. Jude Medical Inc., St. Paul, Minnesota, US) was inserted and fixed using 2/0 pledgeted Ethibond suture. Tricuspid valve repair with an annuloplasty ring was also performed. The patient underwent bypass smoothly and was in normal sinus rhythm. Assessment of the left atrial appendage for possible ligation or excision was performed. However, it was rudimentary and very small, and no apparent clot was there. Immediate echocardiographic assessment in the intensive care unit demonstrated functioning mitral valve prosthesis, with minimal gradient across the valve, preserved left ventricular function, excellent tricuspid valve repair, and absence of any clot in the heart chambers.

Figure 1: Computed tomography of the brain showed no hemorrhage or detectable ischemia at the (a) basal, (b) middle, or (c) cranial brain level.
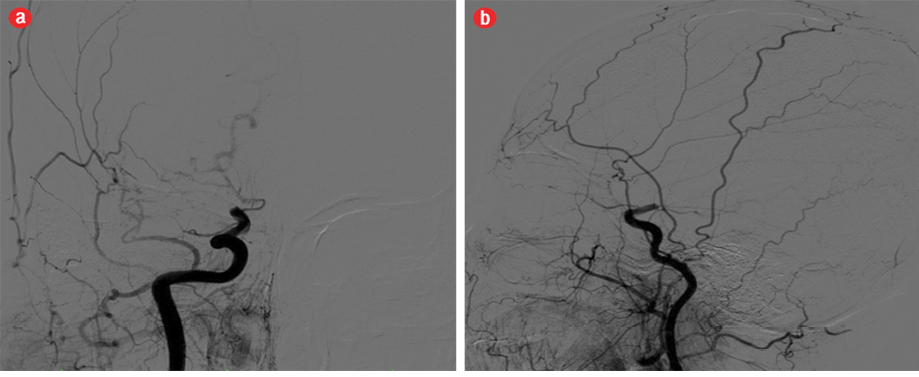
Figure 2: Cerebral angiography demonstrating (a) complete occlusion of the right middle cerebral artery territory. (b) There was no obvious dye leakage in the right middle cerebral artery territory.
The patient had a smooth recovery period, and a therapeutic international normalized ratio (INR) value less than 2.2. She was planned for possible discharge in the coming few days. The patient had a sudden deterioration in her level of consciousness and left-sided weakness. An immediate brain computed tomography (CT) scan was performed [Figure 1]. Cerebral CT angiography demonstrated complete occlusion of the right middle cerebral artery territory [Figure 2a and 2b]. She was rushed to the catheterization laboratory and, via the right femoral artery approach, selective angiography of the vertebral and carotid arteries was performed. We confirmed the presence of an occluded right middle cerebral artery. A small microcatheter (size 018-FR) was advanced with a guidewire to the site of occlusion, and by using the Solitaire Flow Restoration (FR) device (Covidien/ev3, Dublin, Ireland), the clot was pushed against the arterial wall to maintain structural integrity. It was then grasped with multiple struts and dragged gradually. Blush of the middle cerebral artery was confirmed without iatrogenic evidence of arterial wall damage related to device insertion as shown in Figure 3. An immediate clinical improvement was noticed, and the patient recovered completely over three days and was discharged from the hospital in good general status. Follow-up brain CT scan was obtained [Figure 4]. The clot was not sent to the laboratory for examination. On gross assessment, it appeared to be a fresh clot, which may have originated from a cardiac source at the site of the new mechanical valve prosthesis.

Figure 3: Cerebral angiography demonstrating (a) blush in the right middle cerebral artery territory. (b) No iatrogenic evidence of arterial wall damage related to device insertion in the right middle cerebral artery territory was seen.

Figure 4: Computed tomography of the brain showed no hemorrhage or detectable ischemia at the (a) basal, (b) middle, or (c) cranial brain level.
Discussion
Early stroke after cardiac surgery is an important cause of mortality and morbidity. The optimal use of neurointervention technology in managing early ischemic stroke is highly encouraged to shorten the recovery period and save the patient’s life. Different authors have adopted various methods as a way for recanalization for occluded cerebral arteries with variable success rates.3
Nguyen and colleagues5 reported an interest in intra-arterial thrombolysis early in acute ischemic strokes and considered a three hour period as a viable time frame to interfere. However, with the recent advances in neurointervention techniques, and the introduction of mechanical thrombectomy, the time frame had been extended up to eight hours, with a recanalization rate of 60%.6 Better results were demonstrated in the SWIFT trial using a Solitaire stent device for retrieval of fresh clots in large vessels such as the internal carotid artery, middle cerebral artery parts (M1 and M2), and the basilar artery. Recanalization rates approached 83%, and recanalization without symptomatic intracranial hemorrhage approached 61%.4
A possible explanation for the greater success achieved using the Solitaire flow restoration device, is that it pushes the clot against the vascular wall and traps it with multiple struts. It also maintains enough structural integrity while dragging the clot.
The encouraging results shown by the authors4 led us to choose mechanical thrombectomy as a first-line therapy rather than intra-arterial thrombolysis in our patient’s clinical scenario.
In our case, the younger age of the patient and the presence of good collateral circulation had a positive impact on the success of the treatment. Our case demonstrates the successful outcome achieved by mechanical thrombectomy as a method of endovascular reperfusion in managing early ischemic stroke after cardiac surgery.
Conclusion
We aimed to shorten the recanalization time in patients who experienced ischemic stroke following cardiac surgery. A team approach which includes neurologists and neuro-interventionists is crucial in the management of such cases. Using mechanical thrombectomy as a first-line option, instead of intra-arterial thrombolysis, could be of benefit.
Disclosure
The authors declared no conflicts of interest.
references
- Filsoufi F, Rahmanian PB, Castillo JG, Bronster D, Adams DH. Incidence, imaging analysis, and early and late outcomes of stroke after cardiac valve operation. Am J Cardiol 2008 May;101(10):1472-1478.
- McKhann GM, Grega MA, Borowicz LM Jr, Selnes OA, Baumgartner WA, Royall RM. Encephalopathy and Stroke After Coronary Artery Bypass Grafting. Curr Treat Options Cardiovasc Med 2004 Jun;6(3):171-178.
- Jongsathapongpan A, Raumthanthong A, Muengtaweepongsa S. Successful recanalization with multimodality endovascular interventional therapy in acute ischemic stroke. World J Clin Cases 2014 Mar 16;2(3):78-85.
- Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al; SWIFT Trialists. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet 2012 Oct;380(9849):1241-1249.
- Nguyen TN, Babikian VL, Romero R, Pikula A, Kase CS, Jovin TG, et al. Intra-arterial treatment methods in acute stroke therapy. Front Neurol 2011 Mar 8;2:9.
- Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al; Multi MERCI Investigators. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke 2008 Apr;39(4):1205-1212.