|
Abstract
Objectives: To define the role of endoscopic evaluation of middle meatus in adult patients clinically diagnosed to have chronic rhino-sinusitis and its ability to predict intra-sinus mucosal involvement as compared to CT scan.
Methods: This prospective analytical study was conducted on consecutive patients with diagnosis of chronic rhino-sinusitis who were symptomatic and fulfilled the American Academy of Otolaryngology - Head and Neck Surgery Task Force criteria. The patients were enrolled prospectively and were subjected to rigid diagnostic nasal endoscopy and classified as defined by the revised Sinus Allergy Health Partnership Task Force criteria. The patients then underwent non contrast CT sinuses on the same day. Results were analyzed as a diagnostic test evaluation using CT as a gold standard.
Results: Among the 75 study patients with symptom based chronic rhino-sinusitis, nasal endoscopy was abnormal in 65 patients (87%). Of these patients, 60/65 (92%) showed positive findings on CT scan. Ten patients had normal endoscopy, of these 6/10 (60%) had abnormal CT scan. Sensitivity and specificity of diagnostic nasal endoscopy against CT scan were 91% (95% CI: 81-97) and 44% (95% CI: 14-79), respectively. The likelihood ratio for positive nasal endoscopy to diagnose chronic rhino-sinusitis was 1.6 and the likelihood ratio to rule out chronic rhino-sinusitis when endoscopy was negative was 0.2.
Conclusion: Nasal endoscopy is a valid and objective diagnostic tool in the work up of patients with symptomatic chronic rhino-sinusitis. When clinical suspicion is low (<50%) and endoscopy is negative, the probability of rhino-sinusitis is very low (<17%) and there is no need to perform a CT scan to reconfirm this finding routinely. Endoscopy alone is able to diagnose chronic rhino-sinusitis in >90% of patients when clinical suspicion is high (88%) as defined in this study by AAO-HNS Task Force criteria. Negative endoscopy, however, does not totally exclude the sinus disease in patients fulfilling task force criteria. CT scan may be needed on follow-up if there is clinical suspicion in 10% of these patients who are negative on endoscopy if symptoms persists. It is thus possible to reduce the number of CT scans if patients are carefully selected based on clinical criteria and endoscopy is done initially as part of their evaluation.
Keywords: Chronic; Sinusitis; Endoscopy; CT scan; Sensitivity; Specificity; Likelihood ratio.
Introduction
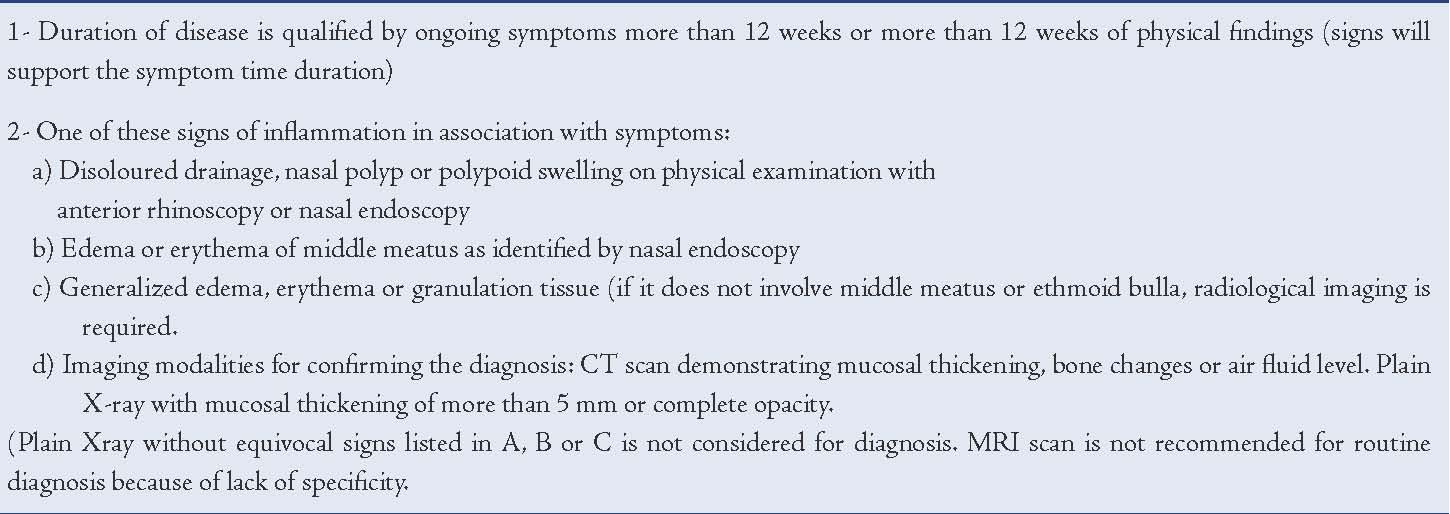
Chronic rhinosinsusitis (CRS) is one of the common diseases affecting people globally with significant negative impact on quality of life.1 The definition of CRS is currently based on subjective symptoms as defined by the American Academy of Otolaryngology- Head and Neck Surgery (AAO-HNS) Task Force criteria,2 detailed in Table 1, which was revised in 2002 by the Sinus Allergy Health Partnership (SAHP) Task Force (Table 2).3 The SAHP task-force stressed the need for objective criteria in confirming the diagnosis and initiating treatment. In the hospital setting, diagnostic nasal endoscopy and CT scan are routinely used to establish the diagnosis of CRS.
CT scan had been well accepted as a mandatory pre-requisite for endoscopic sinus surgery, in suspected complications of sinusitis and in neoplasms of the nose and paranasal sinuses. In the diagnosis of CRS, its association with the symptoms score have been evaluated by a number of studies.4-7 However, due to the lack of agreement, high cost of CT scan and exposure to ionizing radiation, many do not recommended CT scan to form part of routine work up for CRS.8-13
Nasal endoscopy plays a key role in identifying anatomical structural variations and mucosal changes of middle meatus and osteomeatal complex causing drainage block leading to CRS both in patients with normal CT and in patients with abnormal scans.10,14-16 It was also noted earlier that there was close association between endoscopy and CT scan in the diagnostic work up of CRS.14,17 However, both nasal endoscopy and CT scan are performed to establish diagnosis in routine practice since the relative values of each has not been well established.
Table 1: Clinical Categories of Adult Rhinosinusitis (1996 AA0-HNS Task Force).
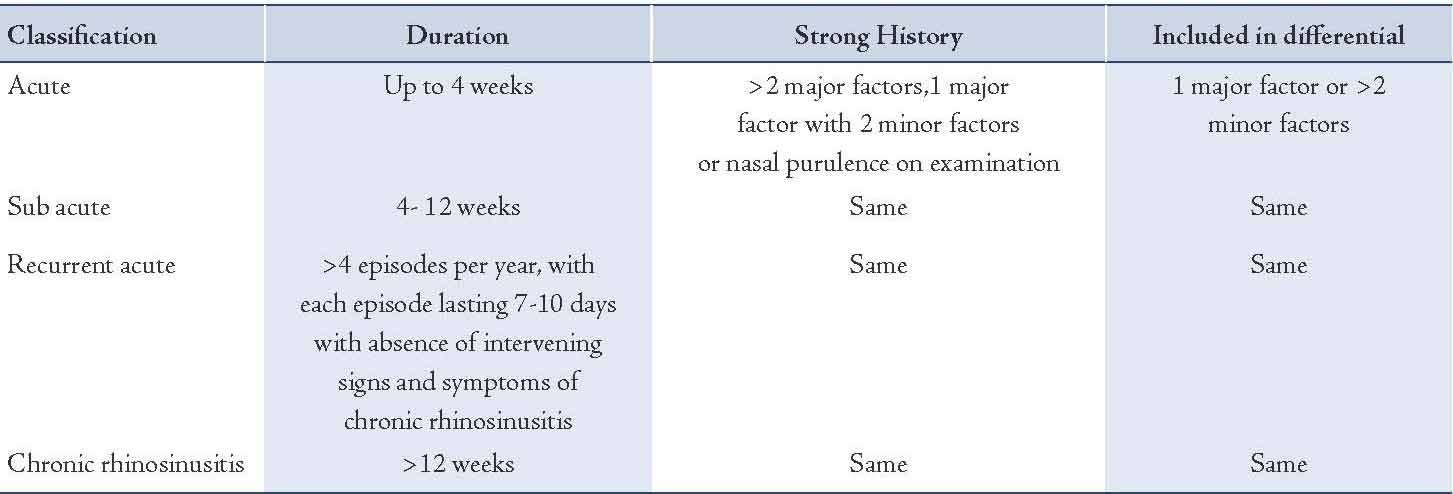
Table 2: Clinical diagnostic criteria of CRS Revision (2002 SAHP Task Force).
Nasal endoscopy is a mandatory clinical examination in ENT, more so in patients with sino-nasal symptoms. CT scan provides information on anatomical variations, sinus status and complications.18 To perform a CT scan merely to confirm CRS preoperatively poses the unacceptable risk of additional exposure to ionizing radiation, not to mention the additional cost of the procedure. There is need to evaluate whether nasal endoscopy can replace CT scan in the diagnostic algorithm of CRS, with CT being reserved for specific indications in this setting. Hence this study was undertaken.
Methods
This study was part of the original work conducted by the primary author over a period of three years in a tertiary teaching hospital in India. This prospective analytical study was cleared by the Institutional Ethical Committee and Review Board. Informed written consent was obtained from all the participating patients.
The sample size was calculated based on the assumption that when compared to CT scan as gold standard, nasal endoscopy will exhibit nearly 90% sensitivity and 75% specificity. In that scenario, if 75 patients are included in the study, it is possible to estimate with 95% confidence, the precision of sensitivity and specificity at 7% and 10%, respectively.
Consecutive patients who were symptomatic and fulfilled the AAO-HNS Task Force criteria,2 for diagnosis of CRS were enrolled into the study. Patients with acute rhino sinusitis, clinically proven allergy and extensive nasal polyposis, as well as previous history of facial trauma or sino-nasal surgeries, who were aged less than 15 years, were excluded. Rigid nasal endoscopy was performed on all subjects under local anesthesia with topical application of 2% Xylocaine (2% Lidocaine Hydrochloride, AstraZeneca, Sweden) and using 30º 4 mm diameter rigid nasal endoscope (Karl Stortz Sinuscope, KARL STORZ GmbH & Co. KG, Tuttlingen, Germany) in accordance with by SAHP Task Force criteria for defining adult CRS.3 The endoscopic examination of frontal recess, middle meatus and spheno-ethmoid recess were reviewed for the presence of polyps, mucosal edema, congestion, discharge, scarring or crusting. The endoscopic findings have been well established by Lund Kennedy Endoscopic Grading System and scored as: polyp (0 - absent, 1- within middle meatus, 2 - beyond the middle meatus), discharge (0 - absent, 1 - thin clear, 2 - thick purulent), edema (0 - absent, 1 - mild, 2 - severe), and scarring (0 - absent, 1 - mild, 2 - severe).19 Endoscopy was categorized as ‘negative’ (Endo-) if Lund Kennedy score was 0. Patients who obtained any other score were categorized as abnormal and ‘positive’ (Endo+).
All patients were then subjected to coronal CT scanning (Siemens somatom DRH and GE Pace - single slice helical CT scanner, Germany) within 24-48 hrs. The radiological imaging has also been accepted by the well recognized Lund MacKay System with each sided sinuses and osteomeatal complexes considered separately and scored: the status of maxillary, anterior ethmoids, posterior ethmoids, sphenoid and frontal sinuses as 0 - no abnormality, 1- partial opacity, 2- Complete opacification; and osteomeatal complex as 0 - no obstruction, 2 - obstructed.20 Zero score for sinuses and osteomeatal complex was considered ‘negative’ (CT-) and scores above 0 were classified as ‘positive’ (CT+). All the assessments of CT and endoscopy were performed independently and assessors were blinded to each other’s scores.
The data was tabulated and analyzed using the software program ‘Statistical Product and Service Solutions’ (SPSS) version 12. Sensitivity, specificity and likelihood ratios (LR) were estimated for endoscopic diagnosis of CRS using CT scan as gold standard.
Results
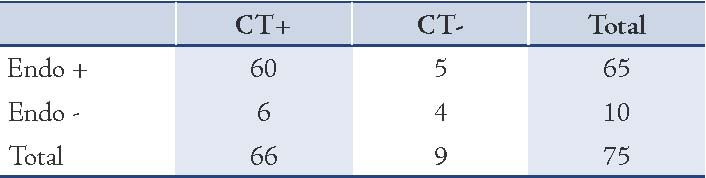
Among the 75 studied patients, 42 were males and 33 were females. The results are displayed in Table 3. Overall, 87% of patients had abnormal endoscopic examination, with 92% showing positive CT scan. In the remaining 13% of patients who showed normal endoscopy, 60% had abnormal CT. The sensitivity of endoscopy was 91% (95% CI: 81% to 97%) and the specificity was 44% (95% CI: 14% to 79%). The Likelihood ratio (LR) for a positive endoscopy to diagnose CRS is 1.6 and the Likelihood ratio for a negative test to rule out CRS was 0.21. This means that one can effectively rule out CRS (post test probability of less than 17%) if the pretest probability is less than 50% and if endoscopy is not suggestive of the diagnosis. The post test probability of positive and negative endoscopy results with pretest probability of 90%, 50% and 30% are 96% and 65%; 62% and 17%; 41% and 8% respectively.
Table 3: Results of study population (n = 75).
Discussion
The current definition of CRS as defined by the 1996 AAO-HNS task force is based only on subjective data. The accuracy and validity of such a definition has been questioned in light of recent studies (Table 1).2 A later revision of the SAHP task force (sinus allergy health partnership) in 2002 emphasized the need to reconfirm CRS by adopting physical evidence of mucosal changes and asserted that such concrete signs such as purulent drainage, polyps, polypoid changes, localized mucosal edema, erythema and granulations are needed to reach a definitive diagnosis. Nasal endoscopy and imaging were therefore recommended for confirmation.3 (Table 2)
Bhattacharya et al. in 1997,5 and Bradley and Kountakis in 2005,21 compared sino-nasal symptoms (Sino-Nasal Outcome Test: SNOT-20) and CT scan findings (latter with respect to severity of mucosal thickening) and found no significant agreement between the two. The frequently quoted prospective study by Stankiewicz and Chow et al.17 on 78 patients who fulfilled the symptomatic criteria for CRS revealed normal CT scans in more than half of the patients (52%) and only 29% of patients had findings on nasal endoscopy.
In the current study, 22% showed positive endoscopy and CT findings while 35% were negative on both endoscopy and CT. Though the authors concluded that positive endoscopy correlated well with CT, it did not specify whether endoscopy could replace CT scan in the majority of patients clinically diagnosed to have CRS. Hwang et al. conducted a review of literature and pointed out the lack of association between imaging and CRS symptomatology.22 The role of CT scan in the work up of CRS is thus debatable and there are obvious problems associated with the routine use of this diagnostic procedure for management of CRS. Although, Nass et al. suggested that a combination of CT and endoscopy is more effective in diagnosing CRS than either modality alone, this hypothesis has not been supported by appropriate data and analysis.23
From the literature, it appears that nasal endoscopy provides more important objective evidence of CRS and corroborate CT findings in the majority of patients.17,24,25 In addition, nasal endoscopy allows targeted culturing, quantification of microbial levels and harvesting of inflammatory mediators or esoinophils.3 Indeed, endoscopy sometimes provides information which CT would not demonstrate such as muco-ciliary loops.12 However, our study raises the concern of whether it is justifiable to use CT scan as a routine diagnostic tool for CRS. In the present study, the pretest probability was 88% (66/75) after screening patients and selecting those with symptoms. This means that in a diagnostic algorithm which uses symptoms screening followed by endoscopy, the post test probability reaches 94% and CT scan cannot add much to this diagnostic probability. Nevertheless, when the pretest probability is less than 50% and endoscopy is negative, the post-test probability is as low as 17%. Thus, CT scan may not be indicated in this situation. It could probably be considered when the symptoms persist in spite of medical therapy or when a surgical intervention is needed.
The National Radiation Protection Board (NRPB) has suggested that CT has become one of the major contributors towards the increased collective population dose from medical radiology. The over utilization of resources and cost are other two limiting factors.12 Hence, this study was conducted to determine whether nasal endoscopy may be used as an alternative by any means. Our study differs from other similar studies, in that all other previous studies were based on symptom based diagnostic criteria and investigated its diagnostic accuracy based on CT and endoscopic parallels. In the current study, diagnostic endoscopy was incorporated as true objective diagnostic standard for CRS and its role as a diagnostic test was evaluated along with CT scan which is the gold standard. This observation has not been elucidated in the literature to the best of our knowledge.
Our study suggests that a combination of CT and diagnostic endoscopy even though complimentary to each other, does not need to be performed together routinely. The presence of nasal purulence, mucosal changes or polyps seen on endoscopy in CRS is a good indicator and highly sensitive in predicting sinus involvement, and therefore does not require routine imaging, which can be avoided. However, it is important to note that negative endoscopy does not exclude sinus disease, and thus CT may be indicated in symptomatic patients with negative endoscopic findings. It could be stated that CT scan may only need to be considered in patients exhibiting a high index of clinical suspicion with negative endoscopy findings. The findings in the study suggest that this would be limited to a small minority of patients with CRS.
Lloyd et al.10 and Havas et al.11 have pointed out a high incidence of asymptomatic sinus disease in an otherwise normal population. The role of endoscopy in this subgroup of patients could not be addressed in the current study and it is therefore a limiting factor of the study.
Conclusion
Nasal endoscopy is a valid and objective diagnostic tool in the work up of patients with symptomatic CRS. The presence of mucosal disease, purulence, and polyps, alone or in combination on endoscopic examinations has a strong positive association with CT and is a good predictor of sinus disease as our study reveals. Endoscopy alone is able to diagnose CRS with very high levels of confidence and CT scan does not add much to this diagnosis in most cases who fulfill the clinical criteria for diagnosis. Hence, it is not necessary to perform CT scan routinely to reconfirm the findings of endoscopy. However, negative endoscopy does not totally exclude sinus disease in symptomatic patients. Hence, CT scan can be reserved as second level investigation for the subgroup of patients with negative endoscopy who remain symptomatic on follow up.
Acknowledgements
The authors reported no conflicts of interest and no funding was received for this work.
References
1. Kalogiera L, Baudoin T. Evidence based treatment of chronic rhinosinusitis. Acta Clin Croat 2005;44(1):53-58.
2. Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg 1997 Sep;117(3 Pt 2):S1-S7.
3. Benninger MS, Ferguson BJ, Hadley JA, Hamilos DL, Jacobs M, Kennedy DW, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg 2003 Sep;129(3)(Suppl):S1-S32.
4. Kenny TJ, Duncavage J, Bracikowski J, Yildirim A, Murray JJ, Tanner SB. Prospective analysis of sinus symptoms and correlation with paranasal computed tomography scan. Otolaryngol Head Neck Surg 2001 Jul;125(1):40-43.
5. Bhattacharyya T, Piccirillo J, Wippold FJ II. Relationship between patient-based descriptions of sinusitis and paranasal sinus computed tomographic findings. Arch Otolaryngol Head Neck Surg 1997 Nov;123(11):1189-1192.
6. Calhoun KH, Waggenspack GA, Simpson CB, Hokanson JA, Bailey BJ. CT evaluation of the paranasal sinuses in symptomatic and asymptomatic populations. Otolaryngol Head Neck Surg 1991 Apr;104(4):480-483.
7. Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 1991 Jan;101(1 Pt 1):56-64.
8. Bhattacharyya N, Fried MP. The accuracy of computed tomography in the diagnosis of chronic rhinosinusitis. Laryngoscope 2003 Jan;113(1):125-129.
9. Bhattacharyya N. A comparison of symptom scores and radiographic staging systems in chronic rhinosinusitis. Am J Rhinol 2005 Mar-Apr;19(2):175-179.
10. Lloyd GA. CT of the paranasal sinuses: study of a control series in relation to endoscopic sinus surgery. J Laryngol Otol 1990 Jun;104(6):477-481.
11. Havas TE, Motbey JA, Gullane PJ. Prevalence of incidental abnormalities on computed tomographic scans of the paranasal sinuses. Arch Otolaryngol Head Neck Surg 1988 Aug;114(8):856-859.
12. Roberts DN, Hampal S, East CA, Lloyd GA. The diagnosis of inflammatory sinonasal disease. J Laryngol Otol 1995 Jan;109(1):27-30.
13. Jones NS. CT of the paranasal sinuses: a review of the correlation with clinical, surgical and histopathological findings. Clin Otolaryngol Allied Sci 2002 Feb;27(1):11-17.
14. Vining EM, Yanagisawa K, Yanagisawa E. The importance of preoperative nasal endoscopy in patients with sinonasal disease. Laryngoscope 1993 May;103(5):512-519.
15. Kennedy DW. Functional endoscopic sinus surgery. Technique. Arch Otolaryngol 1985 Oct;111(10):643-649.
16. Kennedy DW, Zinreich SJ, Rosenbaum AE, Johns ME. Functional endoscopic sinus surgery. Theory and diagnostic evaluation. Arch Otolaryngol 1985 Sep;111(9):576-582.
17. Stankiewicz JA, Chow JM. Nasal endoscopy and the definition and diagnosis of chronic rhinosinusitis. Otolaryngol Head Neck Surg 2002 Jun;126(6):623-627.
18. Mujaini A, Wali U, Al-Khabori M. Functional Endoscopic Sinus Surgery: Indications and Complications in Ophthalmic Field. OMJ 2009;24:70-79.
19. Lund VJ, Kennedy DW. Quantification for staging sinusitis. International conference on sinus Disease: Terminology, staging, therapy. Ann Otol Rhinol Laryngol 1995;104(Suppl 167):17-21.
20. Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg 1997 Sep;117(3 Pt 2):S35-S40.
21. Bradley DT, Kountakis SE. Correlation between computed tomography scores and symptomatic improvement after endoscopic sinus surgery. Laryngoscope 2005 Mar;115(3):466-469.
22. Hwang PH, Irwin SB, Griest SE, Caro JE, Nesbit GM. Radiologic correlates of symptom-based diagnostic criteria for chronic rhinosinusitis. Otolaryngol Head Neck Surg 2003 Apr;128(4):489-496.
23. Nass RL, Holliday RA, Reede DL. Diagnosis of surgical sinusitis using nasal endoscopy and computerized tomography. Laryngoscope 1989 Nov;99(11):1158-1160.
24. Senior BA, Kennedy DW, Tanabodee J, Kroger H, Hassab M, Lanza D. Long-term results of functional endoscopic sinus surgery. Laryngoscope 1998 Feb;108(2):151-157.
25. Rosbe KW, Jones KR. Usefulness of patient symptoms and nasal endoscopy in the diagnosis of chronic sinusitis. Am J Rhinol 1998 May-Jun;12(3):167-171.
|