|
A 15 year old male patient presented with complaints of chronic intermittent abdominal pain and occasional vomiting. On examination, the patient was anemic and dark brown pigmented cutaneous lesions were seen in the region of the lower lip. The vital parameters were pulse rate (100/min) and BP (120/80 mmHg). No abdominal tenderness was noted. Family history was negative for any gastrointestinal disturbances. The patient underwent barium enteroclysis and Computed Tomography (CT) investigations.
Barium enteroclysis images (Figs. 1 and 2) showed multiple sessile polypoidal lesions (arrows) of varying sizes seen in jejunal loops. No evidence of bowel obstruction was seen. Axial CT image with patient positioned in right lateral decubitus position and with oral contrast (Fig. 3) showed multiple polyps seen as hypodense intraluminal lesions (arrows) outlined by oral contrast. Endoscopic examination showed multiple sessile jejunal polyps.
Question
What is the most likely diagnosis?
1. Polypoid carcinoma
2. Small bowel lymphoma
3. Peutz-Jeghers syndrome
4. Gastrointestinal Stromal Tumor
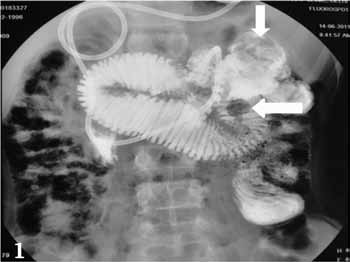
Figure 1: Barium enteroclysis image shows sessile polypoidal lesions (arrows) in proximal jejunal loops.
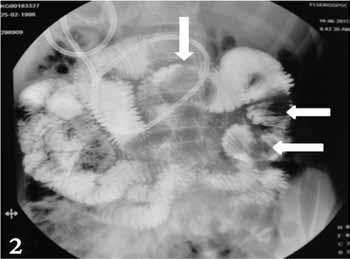
Figure 2: Barium enteroclysis image shows multiple sessile polypoidal lesions (arrows) of varying sizes seen in proximal and distal jejunal loops.

Figure 3: Axial CT image with patient positioned in right lateral decubitus position and with oral contrast shows multiple polyps seen as intraluminal soft tissue lesions (arrows) outlined by oral contrast.
Answer
Peutz-Jeghers Syndrome
Endoscopic examination showed multiple sessile jejunal polyps, which on histologic examination showed features of hamartoma suggestive of Peutz-Jeghers Syndrome.
Discussion
Peutz-Jeghers Syndrome (PJS) is a rare familial autosomal dominant disorder characterized by mucocutaneous pigmentation and gastrointestinal polyps. The penetrance of the disease is often incomplete and sporadic mutations can result in PJS. Hence a negative family history does not exclude PJS as seen in our case. There is no documented racial or sex predilection seen in PJS. Mucocutaneous manifestations include pigmented flat lesions distributed mainly on the lower lip, buccal mucosa and periorbital areas. The gastrointestinal polyps in PJS are hamartomatous polyps and the characteristic histologic finding is a smooth muscle core arising from muscularis mucosae which branches into the substance of polyp.1 The most common locations for polyps are the jejunal and ileal segments of the small bowel, although multiple polyps in the stomach, colon and rectum have been described. Patients are usually diagnosed in the second or third decade of life and they generally present with recurrent abdominal pain, anemia secondary to bleeding and intestinal obstruction due to intussusception.
Radiographic examinations like barium studies can detect the polyps as an intraluminal filling defect which may be pedunculated or sessile. The polyps may vary in size and they commonly occur in clusters. The surface may be smooth or lobulated. When there is associated intussusception, the barium column is seen as a coiled spring appearance due to the outlining of mucosal folds of intussusceptum by barium. Computed Tomography (CT) may be useful for detection of large polyps and for diagnosing extra-intestinal abnormalities. Magnetic Resonance (MR) enteroclysis is an established modality to delineate the polyps and poses no risk of radiation.
The major life-threatening complications to individuals with PJS are malignancies and small bowel obstruction. Patients with PJS are more prone to develop extra-intestinal malignancies like carcinoma of the pancreas, breast, lung and ovary.2 In patients presenting with bowel obstruction or intussceptions, surgical intervention is required. In case of abdominal pain or gastrointestinal bleeding, endoscopic examination is necessary to localize the bleeding polyp so that they can be resected.3,4
References
1. Buck JL, Harned RK, Lichtenstein JE, Sobin LH. Peutz-Jeghers syndrome. Radiographics 1992 Mar;12(2):365-378.
2. Bhattacharya S, Mahapatra SR, Nangalia R, Palit A, Morrissey JR, Ruban E, et al. Melaena with Peutz-Jeghers syndrome: a case report. J Med Case Rep 2010;4:44.
3. Akimaru K, Katoh S, Ishiguro S, Miyake K, Shimanuki K, Tajiri T. Resection of over 290 polyps during emergency surgery for four intussusceptions with Peutz-Jeghers syndrome: Report of a case. Surg Today 2006;36(11):997-1002.
4. Gokhale U, Pillai GR. Large Brunner’s Gland Hamartoma: A Case Report. Oman Med J 2009 Jan;24(1):41-43.
|