A tenosynovial giant cell tumor (TGCT) is a rare benign soft-tissue lesion first described by Chassaignac in 1852. Jaffe and his co-workers further defined the lesion to include synovial tissue, tendon sheath, bursa, and joint structure.1 TGCT usually affects patients in their third to fifth decades of life with roughly equal sex distribution.2,3 TGCT has been reported to mainly involve the finger joints and tendon sheaths of the foot, ankle, and knee. The occurrence of TGCT in the head and neck region is exceedingly rare and relatively uncommon in the temporomandibular joint (TMJ) and skull base.1–5 The TGCT lesion is broadly classified into localized and diffuse type, with literature reporting the localized form accounting for over 75%.3–6 Recently, published work reported that the prevalence per 100 000 persons for localized TGCT was 44.3 and 11.5 for the diffuse form.4 The pathogenesis of TGCT is unknown, but studies have proposed that the neoplasm could be related to bleeding following trauma and lipid metabolism diseases.2,4
Several treatment modalities have been proposed to manage TGCT. While total surgical excision remains the main form of treatment, adjunctive therapies including radiotherapy and/or chemotherapy are advocated in cases of incomplete excision and recurrence.3–5
This short report describes an unusual and unique presentation of a craniofacial TGCT in a 27-year-old male. It highlights the clinical presentation, investigations performed, and the surgical management that have led to a successful outcome with an 18-month follow-up.
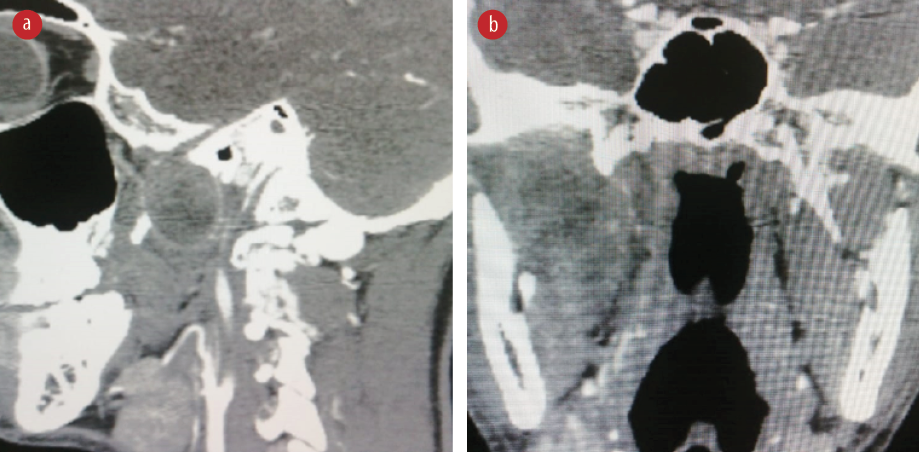
Figure 1: Non-contrast CT. (a) Sagittal and (b) coronal views of the patient showing a round soft tissue lesion with no extensions to the surrounding bones.
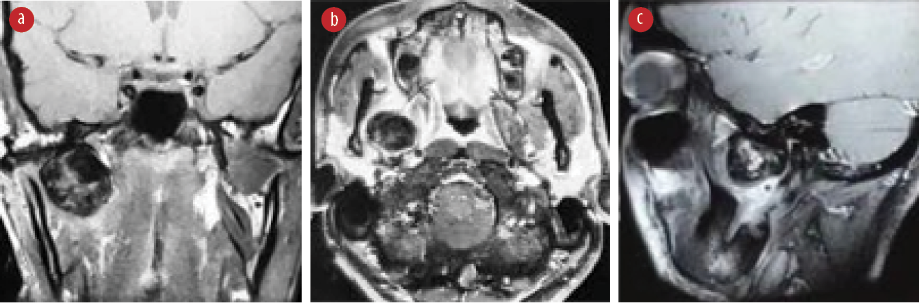
Figure 2: MRI of the patient. (a) Coronal T1-weighted view, (b) axial T1-weighted view, and (c) sagittal T1-weighted view showing a round soft tissue lesion with no bony involvement of the skull base and temporomandibular joint (TMJ). Minimal extension into the soft tissue component of the TMJ.

Figure 3: Surgical procedure stages; (a) marking of the skin incision, (b) marking of the mandibular osteotomy, (c) osteosynthesis fixation with two bone plates, (d) lateral mandibulotomy facilitating direct access to the infratemporal fossa, and (e) endoscopic view of the lesion.
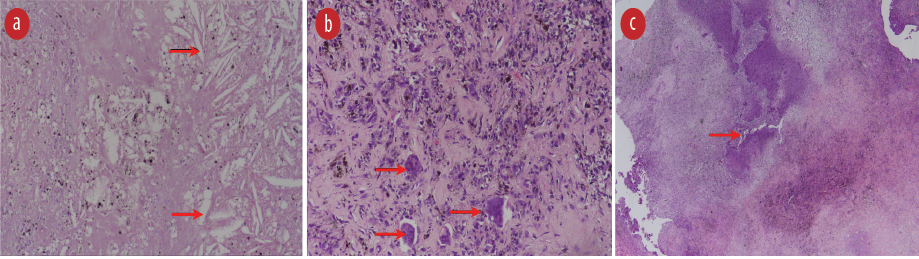
Figure 4: Histopathology images of the tenosynovial giant cell lesion in hemataxylin and eosin stain (a) showing cholesterol clefts (red arrows) and hemosiderin (magnification = 200 ×), (b) multinucleated giant cells (red arrows) in a background of fibrocollagenous tissue with chondroid islands, hemosiderophages and foamy macrophages (magnification = 200 ×), and (c) areas of tissue necrosis (red arrow; magnification = 100 ×).
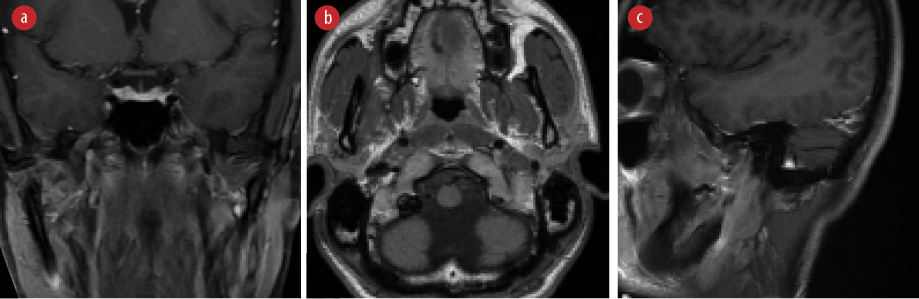
Figure 5: Post-operative magnetic resonance imaging of the patient at 18-months. (a) Coronal T1-weighted view, (b) axial T1-weighted view, and (c) sagittal T1-weighted view showing no recurrence or residual soft tissue mass.
Case report
A 27-year-old male was referred to our department in September 2017 with a chief complaint of a six-month progressive trismus and jaw pain. His medical history was unremarkable, and there was no report of recent trauma or infection. Clinical assessment showed limited mouth opening of 25 mm and pain affecting the right side of the TMJ area. There was no associated clicking or deviation on mouth opening.
An orthopantomograph did not reveal any significant abnormality of the jaw, and non-contrast computed tomography (CT) showed a well-defined round mass in the right infratemporal fossa with no cranial or TMJ bony extensions [Figure 1]. Magnetic resonance imaging (MRI) revealed a defined round soft tissue mass measuring 3.2 × 3.1 × 2.8 cm, medial to right TMJ head with minimal extension into the soft tissue component of the TMJ [Figure 2]. Both CT and MRI excluded the cranial extension and vascular nature of the lesion but highlighted close proximity to the internal carotid and internal maxillary arteries.
Based on the clinical findings and imaging modalities, a differential diagnosis of neurofibroma, trigeminal schwannoma, and giant cell tumor was proposed. As the lesion was located at a relatively inaccessible position and being close to critical anatomical structures, the preoperative diagnostic biopsy was neither feasible nor advisable. Therefore, the patient underwent total surgical excision of the lesion under general anesthesia via trans-oral anterior lateral mandibulotomy approach for direct access to the infratemporal fossa. The approach involved a midline lip split that was extended to the submandibular neck crease. The mandibular symphysis was then exposed, marked, and fixed with two mini bone plates before osteotomy. Subsequently, the mandible was laterally rotated, the lingual and inferior alveolar nerves were identified and protected, and the lateral pterygoid muscle was excised to closely approach the lesion, which was then visualized via endoscope and freed from all attachments ensuring total and complete excision. The maxillary artery branches were circulating the mass, and identified and clipped endoscopically [Figure 3].
The histopathology result showed fibrohistiocytic cells with hemosiderophages, foamy macrophages and osteoclast-type multinucleated giant cells on a background of fibrocollagenous tissue with chondroid islands and osteoid formation. The cells appeared to form a lining giving a partly cystic appearance. There were large areas of coagulated necrosis, cholesterol clefts, hemorrhage, and scattered dystrophic calcifications [Figure 4]. The histopathological features were consistent with chondroid TGCT, a rare subset of localized TGCT that was completely excised.
At 18-months post-operative review, the patient showed remarkable recovery with improvement in mouth opening to 35 mm and resolution of the associated jaw pain. In addition, the 18-month post-operative MRI showed no evidence of recurrence [Figure 5].
Discussion
TGCT is a benign soft-tissue neoplasm that can be seen in the head and neck region.2,3 The neoplasm can be broadly classified according to the clinical appearance and biological conduct into localized or diffused form. The localized form, also referred to as a giant cell tumor of tendon sheath, appears as isolated nodule of tendon sheath. The diffuse, commonly referred as pigmented villonodular synovitis, is an aggressive form that classically infiltrate into the joint, often recur, and may exhibit features of malignant transformation.2,3,6 Scientific literature states that both forms are rare with most reported case studies focusing on the diffused form.2,5–8 Our case falls under the category of localized TGCT and was diagnosed relatively early compared to published cases.5,6,8
The clinical presentation of TGCT over the TMJ and skull base region is considered a rare phenomenon, with only a few cases reported in the literature.5,6,9,10 A recently published population-based study covering a period of 16 years in Denmark failed to show any evidence of TGCT involving the face; thus, highlighting the relatively rare occurrence of TGCT in the facial region.4 The age of the population affected ranges from 25–60 years and with some reports showing a slight female predominance, especially in the localized form of TGCT.4,5,8–10 The average age at presentation was reported as 33.7 years with a roughly 1:1 male to female ratio.3,10 Our case falls into this age range and in line with published reports.2–6,8–12
Clinically, most of the patients with TGCT present with general and non-specific symptoms, including vague jaw pain and gradually progressive trismus with or without an associated facial swelling.5,6 Such incipient presentation of symptoms may lead to delayed diagnosis and significant expansion of the lesion with the risk of involvement of the surrounding vital anatomical structures.10,11,13 One study highlighted that the time to diagnosis of TGCT involving the TMJ and the surrounding tissues was ranged from two months to 15 years with an average duration of symptoms of 30 months.12 Performing imaging, preferably both a CT and an MRI, earlier during the course of the disease as in our case would result in a timely diagnosis
and management.
Total surgical resection of TGCT is the widely recommended treatment modality.3,5–10 The surgical approach depends mainly on the lesion’s location; hence, it may include different surgical approaches.14,15 We utilized the trans-oral lateral mandibulotomy approach combined with endoscopic assistance. This resulted in providing us with wide surgical access and minimal morbidity to the patient.
The literature reports an overall TGCT recurrence rate of 7–32.3% post-surgical excision.2–8 Published work has highlighted that many factors could influence the potential risk of recurrence, and these include; the destructive biological behavior of the tumor, the degree of surgical resection (total or subtotal), and post-resection adjunctive radiotherapy usage.3,5,16 Published meta-analysis research highlighted that gross total resection of the localized TGCT is an optimal and effective treatment modality. Furthermore, they have observed that in cases of subtotal resection, the use of adjunct radiotherapy has significantly reduced the rate of recurrence from 70% to 14.3%, and accordingly, suggested that when sub-total resection is performed, adjunct radiotherapy is highly recommended as an effective treatment for controlling the disease.3 Due to the potential risk of recurrence, patients with TGCT are recommended to be placed on long-term follow-up.3,6 At 18-months follow-up, our patient showed an overall satisfactory recovery with no evidence of recurrence, and he remains under annual long-term review.
Conclusion
TGCT is a benign soft-tissue tumor, which is rarely observed in the craniofacial region. TGCT should be included in the armamentarium of clinical diagnosis for any lesions arising within or in close proximity to the TMJ. Total resection of the lesion offers good treatment outcome and low recurrence rate.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol (Chic) 1941;31:731-765.
- 2. Qin JR, Jin L, Li LK, Zhang SS, Kong J, Yang HY. Diffuse-type giant cell tumor of tendon sheath in the temporal region incidentally diagnosed due to temporal tumor: a report of two cases and review of the literature. Oncol Lett 2015;10(2):1179-1183.
- 3. Freeman JL, Oushy S, Schowinsky J, Sillau S, Youssef AS. Invasive giant cell tumor of the lateral skull base: a systematic review, meta-analysis, and case illustration. World Neurosurg 2016 Dec;96:47-57.
- 4. Ehrenstein V, Andersen SL, Qazi I, Sankar N, Pedersen AB, Sikorski R, et al. Tenosynovial giant cell tumor: incidence, prevalence, patient characteristics, and recurrence. A registry-based cohort study in Denmark. J Rheumatol 2017 Oct;44(10):1476-1483.
- 5. Biyani P, Khurram SA, Thomas M, Nusrath M. Chondroid tenosynovial giant cell tumour: a rarity in the temporomandibular joint. Br J Oral Maxillofac Surg 2019 Apr;57(3):282-284.
- 6. Bredell M, Schucknecht B, Bode-Lesniewska B. Tenosynovial, diffuse type giant cell tumor of the temporomandibular joint, diagnosis and management of a rare tumor. J Clin Med Res 2015 Apr;7(4):262-266.
- 7. van der Heijden L, Gibbons CL, Dijkstra PD, Kroep JR, van Rijswijk CS, Nout RA, et al. The management of diffuse-type giant cell tumour (pigmented villonodular synovitis) and giant cell tumour of tendon sheath (nodular tenosynovitis). J Bone Joint Surg Br 2012 Jul;94(7):882-888.
- 8. Gong ZC, Lin ZQ, Moming A, Ling B, Liu H, Hu M, et al. Extra-articular diffuse tenosynovial giant cell tumour of the infratemporal fossa: report of a case and literature review. Int J Oral Maxillofac Surg 2010 Aug;39(8):820-824.
- 9. Omura S, Mizuki N, Bukawa H, Fujita K. Diffuse variant tenosynovial giant cell tumor of the temporomandibular joint: report of a case. J Oral Maxillofac Surg 1998 Aug;56(8):991-996.
- 10. Tel A, Spinzia A, Boggio M. Diffuse tenosynovial giant cell tumour of the temporomandibular joint. Int J Oral Maxillofac Surg 2012 Mar;41(3):321-323.
- 11. Sasagawa Y, Tachibana O, Shiraga S, Takata H, Kinoshita E, Nojima T, et al. Secondary malignant giant cell tumor of the clivus: case report. Clin Neurol Neurosurg 2012 Jul;114(6):786-788.
- 12. Zhang C, Zhu L, Lizhen Wang L, Hu Y, Li J, Tian Z. Diffuse tenosynovial giant cell tumor in the temporomandibular joint area in a Chinese population: a clinicopathological analysis of 32 cases. Int J Clin Exp Pathol 2016;9(2):1105-1115.
- 13. Stojadinovic S, Reinert S, Wildförster U, Jundt G. Destruction of the glenoid joint fossa by a tenosynovial giant-cell tumour of the skull base: a case report. Int J Oral Maxillofac Surg 1999 Apr;28(2):132-134.
- 14. Nair S, Sridhar KR, Shah A, Kumar B, Nayak K, Shetty P. Maxillectomy through mandibulotomy – a retrospective clinical review. J Oral Maxillofac Surg 2011;69(7):2040-2047.
- 15. Mehanna P, Devine J, McMahon J. Lip split and mandibulotomy modifications. Br J Oral Maxillofac Surg 2010 Jun;48(4):314-315.
- 16. Yan H, Wang F, Xiang L, Zhu W, Liang C. Diffuse giant cell tumors of the tendon sheath in temporomandibular joint: two case reports and review of the literature. Medicine (Baltimore) 2018 Jun;97(25):e11101.