Kidney disease (KD) can be acute or chronic. Chronic kidney disease (CKD) is diagnosed using internationally accepted criteria when there is an estimated glomerular filtration rate (GFR) < 60 mL/min/1.73 m2 and/or persistent albuminuria.1 KD has five defined stages, and CKD includes stages three to five, where it can be deduced that approximately 50% of kidney function has been lost. This significantly increases the risk of morbidity and premature death.2 End-stage renal disease (ESRD), also known as kidney failure, is the most severe form of CKD because, at this stage, death is inevitable without renal-replacement therapy, which can be done either with dialysis or a kidney transplant.3
CKD has been estimated to affect as much as 10–15% of the population worldwide, which has increased the disease burden of morbidity and mortality.4,5 For instance, the median prevalence of CKD was 7.2% in persons aged 30 years or older from a systematic review of 26 studies in different populations including 10 studies from America, eight studies from Europe, and eight studies from Asia and Australia;6 the overall prevalence of CKD varied from 23.4% to 35.8%.7 However, the increasing burden of CKD prevalence is not just limited to western countries, but also in sub-Saharan Africa where both infectious and non-communicable diseases contribute risk to poor health outcomes. For instance, the estimated prevalence of CKD is 13.9% in sub-Saharan Africa, which is similar to global prevalence estimates of 13.4%.5,8,9 The incidence rate of CKD is projected to increase disproportionately. Countries in sub-Saharan Africa face numerous problems where health transitions are characterized by rapid urbanization, low life expectancy, structural difficulties, unemployment, gender imbalances in access to social well-being, and poverty. Thus, poor health infrastructures and the absence of health screening and prevention programs are systemic factors that further accentuate the risk of KD.
Community studies in Nigeria have reported the prevalence of CKD to be 11.4–18.8%.2,7 For instance, in one study, the enormity of CKD in Nigeria (with the situation in tertiary healthcare in Southeast of Nigeria as a reference) revealed that ESRD cases accounted for 8% of all medical admissions and 42% of renal admissions.10 However, there is a dearth of community-based data on the epidemiology of CKD in Nigeria. The prevalence of CKD in Nigeria ranges from 8–45%, and the reported prevalence largely depends on the population studied (urban/rural or general/at-risk population) and methodology.2,11,12 Similarly, proteinuria, a well-accepted marker of CKD, is common in the general population ranging from 4.7% in South-south Nigeria13 to 23.9%14 in Southwest Nigeria. Thus, the prevalence is likely to increase as KD risk factors are projected to increase in the coming years, especially in countries with emerging economies.8,15
In Nigeria, and as well as in many other African countries, biomedical risk factors such as hypertension, diabetes, and chronic glomerulonephritis are common in the general population. Thus, poor knowledge of the health implications of these biomedical risk factors often underscore the need for screening and early detection of the disease.2,10,16 Other causes, which include genetic (hereditary) and modifiable causes (socioeconomic, lifestyle, and culture), have also been identified as risk factors. In Nigeria, there is low knowledge and awareness of KD risk factors in certain populations.10 In some instances, the causes may be unclear because of the advanced nature of the disease, and could be associated with unknown causes from in and around the environment. Also, the scarcity of kidney replacement therapy facilities is significantly associated with economic and public health burden where few severe KD patients can afford to pay for renal-replacement therapy.10
In Nigeria, the peak prevalence of CKD is between the third and fifth decade of life, which contributes to manpower shortages and economic waste.16,17 The burden of the disease has increased significantly and the lack of a national renal registry and coordinated national health policies have affected the equitable allocation of resources and restricted the efforts towards effective planning and control measures.18 The initial stages of KD can be asymptomatic, and early detection is problematic for many patients. Besides, undiagnosed and untreated KD sufferers may gradually advance to ESRD, and costly renal therapy treatment becomes essential to sustain the patients’ life.10
The major challenge of individuals with KD is the late presentation in an advanced stage which is stemmed from poor knowledge of the disease and its risk factors as cited by many studies.2,19 To a great extent, knowledge is central to social behavior and the level of knowledge on any issue/phenomenon will have implication for man’s disposition towards it. Knowledge affects the ability to make informed decisions. Thus, medical knowledge of any health condition will inform an individual’s actions towards the health condition and health-seeking behavior.20 Specifically, knowledge of KD will make people take actions to avoid kidney problems and get knowledge on how to manage one if it exists.
Epidemiological studies have shown a low knowledge of KD risk factors in developed countries. For instance, in the US, the awareness of CKD among individuals with a GFR of 15–60 mL/min was 24.3%,21 while in Australia only 2.8% and 8.6% of the population studied were able to cite hypertension and diabetes, respectively, as CKD risk factors.22 In a study among African Americans, only 23.7% knew at least one laboratory test for KD, and < 3.0% agreed that CKD is an important health condition.23 However, awareness of CKD was higher among people with the advanced stage of the disease.24 However, studies on knowledge and awareness of KD in Nigeria is scanty, as most were hospital-based.
Improving the public’s knowledge of KD and its risk factors is an important strategy for CKD prevention. Therefore, this study sought to estimate the level of knowledge of KD and its main sociodemographic determinants in order to strategize on preventive modalities using the information gathered from Nigerian population in Lagos State.
Methods
We conducted a cross-sectional study in six urban and two semi-urban local government areas of Lagos State, located in the Southwestern part of Nigeria. The six urban (Agege, Ajeromi-Ifelodun, Lagos Island, Lagos Mainland, Kosofe, and Somolu) and two semi-urban (Epe and Ikorodu) areas were randomly selected from sixteen urban and four semi-urban local government areas in Lagos State. Lagos State was selected for this study owing to the fact that it was featured prominently as one of the KD-prone states in 2015.25
An earlier hospital-based study highlighted the enormity of CKD in Nigeria reporting a prevalence that ranged from 8% to 42%,10 while a previous community-based study reported a prevalence of 27.2%.26 The sample size of this study was extrapolated from that value with 95% confidence interval (CI) and 5% error margin using the appropriate formula for study population > 10 00027 giving us 1071 participants. Participants had to be ≥ 15 years to be included in the study. This number was increased to 1757 to make allowance for 10% possible non-responders and increase the scope of the study. Respondents who were ≥ 15 years, non-Nigerian by nationality, and those who did not give informed consent were excluded from the study.
A multi-stage systematic sampling technique was used. According to the National Population Commission (NPC) of Nigeria census of 2006, the estimated population of the six urban and two semi-urban areas selected for this study, projected to 2016, was 2 741 396. The projection formular was adopted from similar studies.2,28 There are 246 wards in Lagos State and 24 wards were randomly selected by balloting, and these served as sampling units for this study. One hundred and thirteen enumeration areas (EAs) (representing 30%) of the total EAs were selected randomly. The population aged 15 years and above in the selected EAs was estimated using the NPC figures giving 421 757. Dividing this estimated population (421 757) by the sample size (1757) gave the sampling interval for the systematic selection of participants, which was approximately 1:10. Hence, one in every ten respondents was enrolled for the study. Selected houses where every 10th respondent was residing were given unique numbers for identification. The Kish conversion sheet was used to select the participants in each household.29,30 In situations where selected EAs were not adjoined, the first house in the next EA was regarded as a continuation of the previous EA and the selection procedure continued.
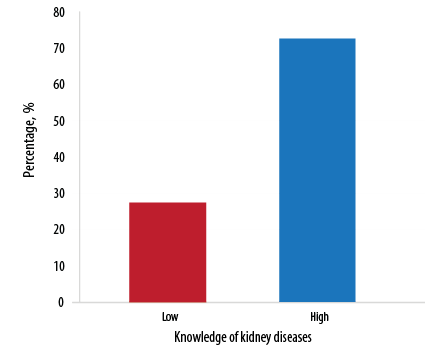
Figure 1: Percentage of respondents with low and high levels of knowledge of kidney diseases.
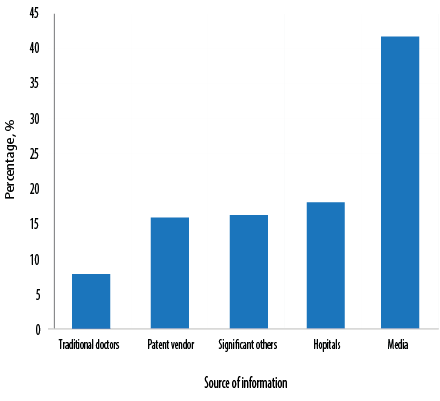
Figure 2: Respondents’ sources of information on kidney diseases.
The questionnaire used in this study was developed based on the KD knowledge evaluation questionnaire originated from the National Kidney Disease Education Program. Also, several previous KD knowledge surveys2 were used for this purpose. Its validity was confirmed by a panel of experts, including five medical sociologist professors, health demographers, and public health professionals. The questionnaire was pretested in a pilot study comprised of 200 respondents to ensure its clarity and relevance. The pilot study results were reviewed critically and further minor modifications were made to improve the clarity and comprehensibility of the questions. The estimated time for completing the questionnaire was approximately 15 minutes.
The results of the pre-test were not included in the final analysis. In addition, the questionnaire had two parts. The first part concerned demographics and comprised of questions concerning educational status, age, occupation, religion, ethnicity, employment status, and household income. The second part was composed of 30 multiple-choice questions to determine knowledge of KDs, which was the outcome of interest in this study. With a score range of 0–59, a binary variable was created with a mean score of 28.37, where knowledge score of 0–28 were coded ‘0’ (low knowledge) and score of 29–59 were coded ‘1’ (high knowledge). The predictor variables/sociodemographic factors (age, sex, educational status, marital status, religion, ethnic group, employment status, and monthly income) were used to explain the outcome variable. Other explanatory variables were the risk-inducing lifestyles (including both modifiable and biomedical risk factors) to give a composite lifestyle pattern of Nigerians residing in Lagos State.
The study was approved by the University of Ibadan Social Sciences and Humanities Research Ethics Committee (SSHEC), Nigeria (UI/SSHEC/14/0003).
The data were analyzed using the SPSS Statistics (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) The data were presented as mean±standard deviation for continuous variables and proportions for categorical variables. The chi-square test was used to explain the associations of the predictor variables on the outcome variable. Binary logistics regression was used to estimate the influence of the independent variables (sociodemographic factors) as a predictor of the outcome variable (knowledge levels).
Results
A total of 1171 respondents completed the study; 586 respondents who took part in the study did not complete either questionnaire or did not have any knowledge of KD and were excluded from the analysis. Table 1 shows the sociodemographic characteristics of the respondents. The mean age of respondents was 33.5±11.1 years with a male to female ratio of 1:0.9 completed the study. Two hundred and sixty (30.1%) respondents and 139 (45.3%) respondents in urban and semi-urban areas, respectively, were aged 30–39 years old. Over half had tertiary education (59.3%) in the urban areas and over three-quarters (77.9%) in semi-urban areas. A greater proportion of the respondents were employed (74.7%) and had a high socioeconomic status (50.7% in urban areas and 48.2% in semi-urban areas) [Table 1].
Figure 1 shows respondents with low and high levels of knowledge of KD. The results revealed that the majority of respondents in this study had high knowledge levels (72.4%).
Majorly, respondents reported media as one of their sources of information on KD [Figure 2]. Table 2 shows the proportion of respondents with low and high knowledge in relation to different sociodemographic variables. Place of residence (p = 0.048), age (p = 0.044), educational level (p < 0.001), and marital status (p < 0.001) were all found to have a significant association with knowledge scores.
The predictors of risk-inducing lifestyles of KDs included significant consumption of herbal supplements (adjusted odds ratio (AOR) = 0.668, 95% CI: 0.51–0.88; p = 0.004), significant alcohol consumption (AOR = 0.751, 95% CI: 0.57–0.99; p = 0.044) and diabetes (AOR = 0.583, 95% CI: 0.44–0.77; p < 0.001) [Table 3].
Table 1: Respondents’ sociodemographic characteristics by location who have knowledge of kidney diseases (n = 1171).
|
Age, mean ± SD, years |
32.4 ± 10.9 |
36.5 ± 11.0 |
33.5 ± 11.1 |
|
|
Age, years |
|
|
|
|
|
< 20 |
139 (16.1) |
13 (4.2) |
152 (13.0) |
62.037* |
|
20–29 |
216 (25.0) |
80 (26.1) |
296 (25.3) |
|
30–39 |
260 (30.1) |
139 (45.3) |
399 (34.1) |
|
40–49 |
126 (14.6) |
61 (19.9) |
187 (16.0) |
|
50 + |
123 (14.2) |
14 (4.6) |
137 (11.7) |
|
Sex |
|
|
|
|
|
Male |
455 (52.7) |
172 (56.0) |
627 (53.0) |
1.031 |
|
Female |
409 (47.3) |
135 (44.0) |
544 (46.5) |
|
Educational level |
|
|
|
|
|
No schooling |
11 (1.3) |
0 (0.0) |
11 (0.9) |
39.021* |
|
Primary |
55 (6.4) |
4 (1.3) |
59 (5.0) |
|
Secondary |
286 (33.1) |
64 (20.8) |
350 (29.9) |
|
Tertiary |
512 (59.3) |
239 (77.9) |
751 (64.1) |
|
Ethnic group |
|
|
|
|
|
Yoruba |
483 (55.9) |
180 (58.6) |
663 (56.6) |
13.555* |
|
Igbo |
219 (25.3) |
96 (31.3) |
315 (26.9) |
|
Hausa |
45 (5.2) |
9 (2.9) |
54 (4.6) |
|
Others |
117 (13.5) |
22 (7.2) |
139 (11.9) |
|
Marital status |
|
|
|
|
|
Single |
537 (55.9) |
157 (51.1) |
694 (59.3) |
13.346* |
|
Married |
292 (33.8) |
139 (45.3) |
431 (36.8) |
|
Separated/divorced |
18 (2.1) |
7 (2.3) |
25 (2.1) |
|
Widowed |
17 (2.0) |
4 (1.3) |
21 (1.8) |
|
Religion |
|
|
|
|
|
Christianity |
669 (77.4) |
223 (72.6) |
892 (76.2) |
33.221* |
|
Islam |
184 (21.3) |
66 (21.5) |
250 (21.3) |
|
Traditionalist |
10 (1.2) |
5 (1.6) |
15 (1.3) |
|
Others |
1 (0.1) |
13 (4.2) |
14 (1.2) |
|
Employment status |
|
|
|
|
|
Working |
627 (72.6) |
248 (80.8) |
875 (74.7) |
8.088* |
|
Not working |
237 (27.4) |
59 (19.2) |
296 (25.3) |
|
Monthly income |
|
|
|
|
|
Low |
197 (22.8) |
119 (38.8) |
316 (27.0) |
|
Middle |
229 (26.5) |
40 (13.0) |
269 (23.0) |
*Significant at p < 0.050. SD: standard deviation.
Table 2: Knowledge scores of kidney diseases by sociodemographic variables (n = 1171).
|
Sex |
|
|
|
|
|
|
|
Male |
185 |
29.5 |
442 |
70.5 |
627 (100) |
0.114 |
|
Female |
138 |
25.4 |
406 |
74.6 |
544 (100) |
|
Age, years |
|
|
|
|
|
|
|
< 20 |
53 |
34.9 |
99 |
65.1 |
152 (100) |
0.044* |
|
20–29 |
53 |
31.4 |
203 |
68.6 |
296 (100) |
|
30–39 |
96 |
24.1 |
303 |
75.9 |
399 (100) |
|
40–49 |
46 |
24.6 |
141 |
75.4 |
187 (100) |
|
50 + |
35 |
25.5 |
102 |
74.5 |
137 (100) |
|
Educational level |
|
|
|
|
|
|
|
None |
5 |
45.5 |
6 |
54.5 |
11 (100) |
0.000* |
|
Primary |
30 |
50.8 |
29 |
49.2 |
59 (100) |
|
Secondary |
112 |
32.0 |
238 |
68.0 |
350 (100) |
|
Tertiary |
176 |
23.4 |
575 |
76.6 |
751 (100) |
|
Ethnic group |
|
|
|
|
|
|
|
Yoruba |
175 |
26.4 |
488 |
73.6 |
663 (100) |
0.072 |
|
Igbo |
80 |
25.4 |
235 |
74.6 |
315 (100) |
|
Hausa |
20 |
37.0 |
34 |
63.0 |
54 (100) |
|
Others |
48 |
34.5 |
91 |
65.5 |
139 (100) |
|
Marital status |
|
|
|
|
|
|
|
Single |
224 |
32.3 |
470 |
67.7 |
694 (100) |
0.000* |
|
Married |
94 |
21.8 |
337 |
78.2 |
431 (100) |
|
Separated/divorced |
1 |
4.0 |
24 |
96.0 |
25 (100) |
|
Widowed |
4 |
19.0 |
17 |
81.0 |
21 (100) |
|
Religion |
|
|
|
|
|
|
|
Christianity |
257 |
28.8 |
635 |
71.2 |
892 (100) |
0.181 |
|
Islam |
61 |
24.4 |
189 |
75.6 |
250 (100) |
|
Traditional |
4 |
26.7 |
11 |
73.3 |
15 (100) |
|
Others |
1 |
7.1 |
13 |
92.9 |
14 (100) |
|
Employment status |
|
|
|
|
|
|
|
Working |
234 |
26.7 |
641 |
73.3 |
875 (100) |
0.269 |
|
Not working |
89 |
30.1 |
207 |
69.9 |
296 (100) |
|
Socioeconomic status |
|
|
|
|
|
|
|
Low |
89 |
28.2 |
227 |
71.8 |
316 (100) |
0.223 |
|
Middle |
84 |
31.2 |
185 |
68.8 |
269 (100) |
|
High |
150 |
25.6 |
436 |
74.4 |
586 (100) |
|
Place of residence |
|
|
|
|
|
|
|
Urban |
225 |
26.0 |
639 |
74.0 |
864 (100) |
0.048* |
|
Semi-urban |
98 |
31.9 |
209 |
68.1 |
307 (100) |
*Significant at p < 0.050.
Table 3: Univariate analysis to determine the risk-inducing lifestyles for kidney disease among the study
respondents (n = 1171).
|
Habitual medicine intake without medical prescription |
|
|
|
|
|
|
|
Yes |
226 (71.3) |
91 (28.7) |
317 (100) |
0.841 |
0.63–1.12 |
0.238 |
|
No |
638 (74.7) |
216 (25.3) |
854 (100) |
|
Habitual analgesic intake |
|
|
|
|
|
|
|
Yes |
166 (82.2) |
36 (17.8) |
202 (100) |
0.864 |
0.54–1.88 |
0.358 |
|
No |
4 (100) |
0 (0.0%) |
4 (100) |
|
Habitual use of herbal supplements |
|
|
|
|
|
|
|
Yes |
230 (68.0) |
108 (32.0%) |
338 (100) |
0.668 |
0.51–0.88 |
0.004* |
|
No |
634 (76.1) |
199 (23.9) |
833 (100) |
|
Excessive use of herbal remedies (agbo) |
|
|
|
|
|
|
|
Yes |
370 (72.1) |
143 (27.9) |
513 (100) |
0.859 |
0.66–1.12 |
0.255 |
|
No |
494 (75.1) |
164 (24.9) |
658 (100) |
|
Significant alcohol consumption |
|
|
|
|
|
|
|
Yes |
240 (69.8) |
104 (30.2) |
344 (100) |
0.751 |
0.57–0.99 |
0.044* |
|
No |
624 (75.5) |
203 (24.5) |
827 (100) |
|
Excessive cigarette smoking |
|
|
|
|
|
|
|
Yes |
65 (72.2) |
25 (27.8) |
90 (100) |
0.918 |
0.57–1.48 |
0.726 |
|
No |
799 (73.9) |
282 (26.1) |
1081 (100) |
|
Lack of moderate/vigorous exercise |
|
|
|
|
|
|
|
Yes |
687 (74.3) |
238 (25.7) |
925 (100) |
1.125 |
0.82–1.54 |
0.462 |
|
No |
177 (72.0) |
69 (28.0) |
246 (100) |
|
Sedentary behaviors |
|
|
|
|
|
|
|
Yes |
250 (71.6) |
99 (28.4) |
349 (100) |
0.855 |
0.65–1.13 |
0.276 |
|
No |
614 (74.7) |
208 (25.3) |
822 (100) |
|
Biomedical risk factors |
|
|
|
|
|
|
|
Hypertension |
|
|
|
|
|
|
|
Yes |
425 (76.4) |
131 (23.6) |
536 (100) |
1.210 |
0.92–1.59 |
0.179 |
|
No |
362 (72.8) |
135 (27.2) |
497 (100) |
|
Diabetes |
|
|
|
|
|
|
|
Yes |
308 (70.6) |
128 (29.4) |
436 (100) |
0.583 |
0.44–0.77 |
0.000* |
|
No |
483 (80.5) |
117 (19.5) |
600 (100) |
|
Overweight |
|
|
|
|
|
|
|
Yes |
68 (78.2) |
19 (21.8) |
87 (100) |
1.351 |
0.80–2.29 |
0.261 |
|
No |
747 (72.6) |
282 (27.4) |
1029 (100) |
|
Obesity |
|
|
|
|
|
|
|
Yes |
41 (83.7) |
8 (16.3) |
49 (100) |
1.971 |
0.91–4.25 |
0.079 |
|
No |
762 (72.2) |
293 (27.8) |
1055 (100) |
|
Heart problems |
|
|
|
|
|
|
|
Yes |
15 (93.8) |
1 (6.3) |
16 (100) |
*Significant at p < 0.050. CI: confidence interval.
Table 4: Predictors of knowledge of kidney disease.
|
Sex |
|
|
|
|
|
|
Male |
- |
- |
- |
- |
- |
|
Female |
-0.208 |
0.132 |
0.812 |
0.114 |
0.63–1.05 |
|
Age, years |
|
|
|
|
|
|
< 20 |
- |
- |
- |
- |
- |
|
20–29 |
-0.445 |
0.260 |
0.385 |
0.087 |
0.39–1.07 |
|
30–39 |
-0.289 |
0.232 |
0.749 |
0.214 |
0.48–1.18 |
|
40–49 |
0.080 |
0.228 |
1.083 |
0.727 |
0.69–1.69 |
|
50 + |
0.050 |
0.259 |
1.052 |
0.846 |
0.63–1.75 |
|
Educational level |
|
|
|
|
|
|
None |
- |
- |
- |
- |
- |
|
Primary |
-1.002 |
0.612 |
0.367 |
0.102 |
0.11–1.22 |
|
Secondary |
-1.218 |
0.274 |
0.296 |
0.000* |
0.17–0.51 |
|
Tertiary |
-0.430 |
0.143 |
0.650 |
0.003* |
0.49–0.86 |
|
Marital status |
|
|
|
|
|
|
Single |
|
|
|
|
|
|
Married |
-0.706 |
0.562 |
0.494 |
0.209 |
0.16–1.48 |
|
Separated/divorced |
-0.170 |
0.568 |
0.844 |
0.764 |
0.28–2.57 |
|
Widowed |
1.447 |
1.162 |
5.250 |
0.136 |
0.58–5.08 |
|
Ethnic group |
|
|
|
|
|
|
Yoruba |
- |
- |
- |
- |
- |
|
Igbo |
0.386 |
0.199 |
1.471 |
0.047 |
0.99–2.17 |
|
Hausa |
0.438 |
0.220 |
1.549 |
0.074* |
1.14–2.39 |
|
Others |
-0.109 |
0.334 |
0.897 |
0.744 |
0.78–1.72 |
|
Religion |
|
|
|
|
|
|
Christianity |
- |
- |
- |
- |
- |
|
Islam |
-1.660 |
1.040 |
0.190 |
0.110 |
0.03–1.46 |
|
Traditional |
-1.434 |
1.048 |
0.238 |
0.171 |
0.03–1.86 |
|
Others |
-1.553 |
1.191 |
0.212 |
0.192 |
0.02–2.18 |
|
Employment status |
|
|
|
|
|
|
Working |
|
|
|
|
|
|
Not working |
0.164 |
0.148 |
1.178 |
0.269 |
0.88–1.57 |
|
Socioeconomic status |
|
|
|
|
|
|
Low |
- |
- |
- |
- |
- |
|
Middle |
-0.131 |
0.157 |
0.877 |
0.405 |
0.65–1.19 |
|
High |
-0.556 |
0.417 |
1.518 |
0.404 |
1.01–2.29 |
|
Place of residence |
|
|
|
|
|
|
Urban |
- |
- |
- |
- |
- |
*Significant at p < 0.050. CI: confidence interval.
Table 4 shows the binary logistic regression analysis of the adjusted independent predictors of knowledge scores of KD. The results revealed that respondents with primary (OR = 0.367, p = 0.102) or secondary (OR = 0.296, p < 0.001) education had significantly negative increased odds of KD knowledge compared with their counterparts with no education. While those with tertiary level education (OR = 0.650, p = 0.003) have lower negative odds KD knowledge compared to respondents with no education (not significant). Conversely, respondents from Hausa ethnic group (OR = 1.549, p = 0.074) have significant decreased odds of KD knowledge compared with those from the Yoruba ethnic groups. While respondents from Igbo (OR = 1.471, p = 0.047) and other ethnic groups (OR = 0.897, p = 0.744) have decreased odds of KD knowledge compared with those from Yoruba ethnic groups. In addition, respondents from semi-urban areas (OR = 1.332, p = 0.048) have decreased odds of KD knowledge compared with those from urban areas [Table 4].
Other variables such as socioeconomic status, age (20-29 and 30-39 years), sex (female), and marital status (married and separated/divorced) were negatively associated with decreased odds of KD knowledge among the respondents (not significant). While age (40-50+ years) were positively associated with decreased odds of KD knowledge among respondents (not significant) [Table 4].
Discussion
The results of this study showed a high level of knowledge of KD among Nigerian communities. The prevalence of high knowledge in our cohort was 72.4%. This is similar to reports of other studies.2,3,31 In this study, the prevalence of KD knowledge was higher than the 9.5% knowledge and 10.0% awareness level reported by Tamura et al.32 Similarly, Shah et al,33 reported a lower prevalence of KD knowledge and awareness (49.4% and 23.0%, respectively). A study in the Iranian community indicated a relative lower limited knowledge of KD.34 However, studies in developing countries revealed lack of KD knowledge among patients before they reported to a hospital with symptoms of CKD.2,35 In developed countries, such as America, only one-third of CKD diagnosed American patients were aware of CKD and its possible treatment modalities.36,37 Thus, educational programs should incorporate healthy practices towards prevention and early detection of KD and disseminating such information to the general population, as especially at the grassroots level.
We found that the main source of KD information was media (41.6%), and this may explain the relatively high level of knowledge. The use of technology-based platforms may be effective in implementing health-related kidney programs in Nigerian communities where mobile health (mhealth) technologies have been adopted and used successfully in public health efforts related to maternal-child health, tuberculosis, and HIV.38,39 Although the use of technology-based platforms for improving non-communicable diseases care in sub-Saharan African countries is not well established, our assessment of healthcare practices related to KD suggested that mobile phones would be a prospective and well-received means of facilitating such public health efforts. Emails may also be useful for health communication and education among certain populations in local urban settings where internet facilities can be found.40,41
In our study population, education and marital status had the strongest associations with the mean knowledge score for KD. In developed countries, the level of education is directly associated with better health outcomes in patients with KD, and education can moderate the effectiveness of interventions.42,43 Thus, health knowledge is a key in aiding in the understanding of basic health information so that the right healthcare decisions can be made leading to better health outcomes. In developed countries, targeting high-risk populations with low levels of health knowledge has been proven to be effective in improving KD care as well as in adopting preventive modalities to reduce its risk factors.44,45 In Nigerian rural communities, it is important to target high-risk individuals with low education and health literacy towards non-communicable diseases, including KD, which may allow for more efficient educational health programs and health interventions that may better account for disparities of health outcomes in urban and rural settings.
High level of education facilitates good discussion for preventive measures between health workers and persons that are most likely to be predisposed to kidney ailments.1,45 Older respondents living in urban/semi-urban settings were associated with high knowledge levels of KD. Age and setting were characterized by a strong interest in learning about KD, as respondents were concerned about their socioeconomic status, health, and the social impact of being diagnosed with KD. Public health efforts aimed at improving knowledge of KD and reducing these concerns have been effective in other low-resource settings outside of developing nations of Africa, and our findings suggest that such efforts would also be well-received and implemented in health policy programs in Nigeria.36,46,47
The findings of this study showed a strong association between KD and habitual use of herbal supplements. Various authors have cited the habitual intake of herbal supplements and as a contributing factor to the increasing prevalence of CKD in Nigerian communities.48,49 However, the association in this study may be explained by the likelihood of biomedical risk factors, which may act concurrently with herbal supplement abuse to cause nephrotoxicity from aristolochic acid resulting in adverse kidney effects and toxicity from contaminants within the extracts and has been implicated in the increasing prevalence of KD.49,50 Similar reasons may explain the significant positive association found between KD and alcohol consumption in this study. This is in agreement with the findings of a previous study that found a significant association with alcohol consumption and renal impairment in the general population of South Korea.51 On the contrary, some studies have reported no association between alcohol consumption and KD.16,52
Habitual analgesic and medicine intake (without a medical prescription) were not found to be a risk factor for KD in this study. This is in agreement with previous studies.53,54 Similarly, analgesic use was not associated with KD.55 In this study, excessive cigarette smoking was not associated with the development of KD, in contrast with findings that identified smoking as a major cardiovascular risk factor that promotes KD progression.2 Cigarette smoking is perceived in Nigerian communities as an antisocial habit with which the subjects possibly may not want to be identified. This may explain the non-significant association of cigarette smoking on the development of KD among our cohort.
In addition, lack of moderate/vigorous physical exercise and sedentary lifestyles did not have a significant association with kidney ailments in this study. This does not agree with the findings of many studies, in which simple exercise can help improve the health of individuals at risk of KD. Thus, sedentary behavior is an important risk factor for diabetes, hypertension, and obesity and are predisposing factors for kidney damage if left untreated or unmanaged.2,16,18,56 Unlike earlier studies from Nigeria that reported an association between KD and hypertension, overweight, obesity, and heart problems,2,16,18 no such association was found in this study. This may be due to a high negative self-reported response rate arising from the respondents having inadequate health information about biomedical risk factors for the development of KD. This study also demonstrated that urgent attention needs to be paid to risk factors for KD and to bring about behavioral health modification interventions to address the rising prevalence of KD risk factors and its slow consequence on the progression of kidney challenges. This need is driven by the inadequate knowledge by the general population of the negative outcome of risk factors on the kidney.
Participants showed poor recognition of the underlying modifiable and biomedical risk factors (risk-inducing lifestyles). Based on that, negative attitudes towards risk-inducing lifestyles were mostly based on the fact that most respondents showed ‘denial of medical reality’ and a misconception about the interconnected kidney risk factors that affect people’s health. Misconceptions and ‘denial of medical reality’ may influence individuals’ predisposition not to engage in healthy lifestyles, and even to seek medical attention if signs or symptoms are not noticed. This finding was applicable in many health diseases and medical conditions such as cardiovascular disease, breast cancer, and heart disease.2,16,57 Also, wrong assumptions about KD predisposing factors, signs and symptoms, disease stage, and related management plan may account for reasons why individuals with kidney challenges present late to medical facilities. Previous studies have shown positive development in health outcomes among populations who receive appropriate health knowledge.36,47 Health interventions aimed at changing misconceptions and improving perceived susceptibility will enhance adoption of healthy practices towards dealing with chronic illnesses, KD inclusive. Therefore, health education about kidney functions, KD-related risk factors, and the benefits of early screening should be encouraged.
Ethnic group (Hausa) and place of residence (semi-urban) were independently associated with decreased odds of KD knowledge. Similarly, female sex, age (20–29 and 30–39 years), marital status (married and separated/divorced), other ethnic groups, and socioeconomic status were associated with negative non-significant decreased odds of KD knowledge. While religion and education (primary) have negative non-significant increased odds of KD knowledge. Hence, those with secondary education have negative significant increased odds of KD knowledge and negative significant decreased odds of KD knowledge with those that have tertiary education. Hence, the findings on the demographic factors with negative odds showed the absence of KD knowledge, which implied that those demographic factors do not predict KD knowledge. But their association with other risk factors are likely to incline an individual to seek adequate KD knowledge. Emphasis should, therefore, be placed on community health intervention programs tailored towards improving Nigerian populations’ knowledge and awareness on the increased tendency to develop KD that are usually associated with risk-inducing lifestyles if left unmodified or unmanaged.
Our study was limited by its cross-sectional nature, where participants were visited only once to gather data. The knowledge of KD was self-reported, and so the concern of recall bias is of significance. Given the cross-sectional nature of our study, we suggest further prospective longitudinal studies about the association between the knowledge of KD and its sociodemographic determinants. We used a quantitative tool to assess knowledge and sociodemographic determinants in our survey. This approach may pose some methodological problems in obtaining the necessary information for this study. In addition, the study did not include a question as to whether or not the participating respondents with KD risk factors had routine medical care or not. This omission should be considered in future surveys.
The strength of our study, however, is the multi-stage systematic sampling method, and to a large extent a good coverage of the urban and semi-urban places of residence where the study was carried out. The sample of the respondents who participated in the survey is large, and allows robust analysis of the topic. Our community-based study found a relationship between knowledge of KD and its sociodemographic determinants. To the best of our knowledge, previous similar studies have been hospital-based. The study addressed a topical issue, considering its impact on the public health of Nigerian populations, and intended to attract the interest of not only investigators but also health policymakers.
Conclusion
The study achieved the aim of evaluating the Nigerian population’s knowledge of KD and its relation to social determinants. Although the results indicated that most participants have knowledge of KD, the majority were found to engage in risk-inducing lifestyles as a result of poor recognition of linking their lifestyles to KD development. At-risk individuals (i.e., individuals with biomedical risk factors) are not adequately informed regarding their increased risk for developing KD. A concerted effort should be made to improve the level of knowledge and awareness among the population with a view to a better understanding of the burden of KD and the solutions to reduce the burden of its related risk factors in their communities. KD should be discussed in public places with anyone with modifiable risk factors and health conditions of KD. Screening programs should incorporate more community awareness talks to raise people’s understanding of the benefits of kidney organ routine check-up, and modification of unhealthy behaviors that will lead to desirable health outcomes. Using this approach will minimize kidney health problems. Health demographers and public health practitioners should assist in planning and designing community health interventional programs that help educate people on health issues such as KD. An important implication for policy development of this study is engaging in multidisciplinary intervention programs, including medical doctors and other non-health professionals. Health demographers and public health practitioners take cognizance of the interplay of culture and the role individuals’ characteristics play, especially among high-risk individuals for KD. Another application for policy development is to provide financed improved health insurance services that will cover early detection and regular routine screening/check-ups for KD. This must be recognized as a priority area for Nigerian governments, given that an average Nigerian engages in self-management and treatment of health problems, acute or chronic (KD inclusive), with poverty standing as an obstacle for seeking medical attention.
Disclosure
The authors declared no conflicts of interest. Funding for this research was received from the URC Postdoctoral Fellowships, South Africa; the National Research Foundation, South Africa; the DST-NRF Centre of Excellence in Human Development, South Africa; the William and Flora Hewlett Foundation; and the National Institute for the Humanities and Social Sciences Funding for Research, Johannesburg, South Africa (Grant no. A0060498).
Acknowledgements
The authors gratefully acknowledge the support of the Wits Demography and Population Studies Programme, Schools of Public Health and Social Sciences, Faculties of Health Sciences and Humanities, University of the Witwatersrand, Johannesburg, South Africa.
references
- Kidney Disease Improving Global Outcomes (KDIGO). KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013 Jan;3:1-150.
- 2. Oluyombo R, Ayodele OE, Akinwusi PO, Okunola OO, Gbadegesin BA, Soje MO, et al. Awareness, knowledge and perception of chronic kidney disease in a rural community of South-West Nigeria. Niger J Clin Pract 2016 Mar-Apr;19(2):161-169.
- 3. Bello AK, Levin A, Tonelli M, Okpechi IG, Feehally J, Harris D, et al. Assessment of global kidney health care status. JAMA 2017 May;317(18):1864-1881.
- 4. Grams ME, Juraschek SP, Selvin E, Foster MC, Inker LA, Eckfeldt JH, et al. Trends in the prevalence of reduced GFR in the United States: a comparison of creatinine- and cystatin C-based estimates. Am J Kidney Dis 2013 Aug;62(2):253-260.
- 5. Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS One 2016 Jul;11(7):e0158765.
- 6. Zhang QL, Rothenbacher D. Prevalence of chronic kidney disease in population-based studies: systematic review. BMC Public Health 2008 Apr;8:117.
- 7. Ulasi IU, Ijoma CK, Onodugo OD, Arodiwe EB, Ifebunandu AN, Okoye JU. Towards prevention of chronic kidney disease in Nigeria: a community-based study in Southeast Nigeria. Kidney Int Suppl 2013;3(2):195-201.
- 8. Stanifer JW, Jing B, Tolan S, Helmke N, Mukerjee R, Naicker S, et al. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health 2014 Mar;2(3):e174-e181.
- 9. Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, et al. Chronic kidney disease: global dimension and perspectives. Lancet 2013 Jul;382(9888):260-272.
- 10. Ulasi II, Ijoma CK. The enormity of chronic kidney disease in Nigeria: the situation in a teaching hospital in South-East Nigeria. J Trop Med 2010;2010(Mar):501957.
- 11. Adetuyibi A, Akinsaya JB, Onadeko BO. Analysis of the causes of death on the medical wards of the UCH Ibadan over a 14yr period (1960-1973). Trans R Soc Trop Med Hyg 1976;70(5-6):466-473.
- 12. Alebiosu CO, Ayodele OE. The global burden of chronic kidney disease and the way forward. Ethn Dis 2005;15(3):418-423.
- 13. Oviasu E, Oviasu SV. Urinary abnormalities in asymptomatic adolescent Nigerians. West Afr J Med 1994 Jul-Sep;13(3):152-155.
- 14. Amira O, Sokunbi D, Sonibare A, Sokunbi A, Finnih O. Risk factors for chronic kidney disease: report of a preventive screening programme conducted in an unselected urban population in South west Nigeria. Trp J Nephron 2007 Dec;2(2):81-87.
- 15. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006 Nov;3(11):e442.
- 16. Afolabi MO, Abioye-Kuteyi AE, Arogundade FA, Bello IS. Prevalence of chronic kidney diseases in a Nigerian family practice population. S Afr Fam Pract 2009;51(2):132-137.
- 17. Ijoma C, Ulasi I, Ijoma U, Ifebunandu N. High prevalence of anemia in predialysis patients in Enugu, Nigeria. Nephrology Reviews 2010 Jul;2(2):e14.
- 18. Okwuonu CG, Chukwuonye II, Adejumo OA, Agaba EI, Ojogwu LI. Prevalence of chronic kidney disease and its risk factors among adults in a semi-urban community of South-East Nigeria. Niger Postgrad Med J 2017 Apr-Jun;24(2):81-87.
- 19. Obrador GT, García-García G, Villa AR, Rubilar X, Olvera N, Ferreira E, et al. Prevalence of chronic kidney disease in the Kidney Early Evaluation Program (KEEP) México and comparison with KEEP US. Kidney Int Suppl 2010 Mar;(116):S2-S8.
- 20. Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q 1984;11(1):1-47.
- 21. Coresh J, Byrd-Holt D, Astor BC, Briggs JP, Eggers PW, Lacher DA, et al. Chronic kidney disease awareness, prevalence, and trends among U.S. adults, 1999 to 2000. J Am Soc Nephrol 2005 Jan;16(1):180-188.
- 22. White SL, Polkinghorne KR, Cass A, Shaw J, Atkins RC, Chadban SJ. Limited knowledge of kidney disease in a survey of AusDiab study participants. Med J Aust 2008 Feb;188(4):204-208.
- 23. Waterman AD, Browne T, Waterman BM, Gladstone EH, Hostetter T. Attitudes and behaviors of African Americans regarding early detection of kidney disease. Am J Kidney Dis 2008 Apr;51(4):554-562.
- 24. Plantinga LC, Boulware LE, Coresh J, Stevens LA, Miller ER III, Saran R, et al. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med 2008 Nov;168(20):2268-2275.
- 25. Bamgboye EL. The looming epidemic of kidney failure in Nigeria. The magnitude of the problem. 2015 Alumni Session II. Consultant Transplant Nephrologist Clinical Director, St Nicholas Hospital Lagos. President, Transplant Association of Nigeria President, Nigerian Association of Nephrology Director-MetroHealth HMO. 2015 March; 1-34. [cited 2015 March]. Available from: https://docplayer.net/34731891-The-looming-epidemic-of-kidney-failure-in-nigeria.html.
- 26. Okoye OC, Oviasu E, Ojogwu L. Prevalence of chronic kidney diseases and its risk factors amongst adults in a rural population in Edo State, Nigeria. J US-China Med Sci 2011 Aug;8(8):471-481.
- 27. Binu VS, Mayya SS, Dhar M. Some basic aspects of statistical methods and sample size determination in health science research. Ayu 2014 Apr;35(2):119-123.
- 28. Lantta T, Kontio R, Daffern M, Adams CE, Välimäki M. Using the dynamic appraisal of situational aggression with mental health inpatients: a feasibility study. Patient Prefer Adherence 2016 Apr;10:691-701.
- 29. Gaziano C. Kish selection method. In: Lavrakas PJ. Encyclopedia of survey research methods. Sage Publications; 2011. p. 1-4.
- 30. Ghorbani B, Shahnazi H, Hassanzadeh A. Improving student’s self-efficacy and perceived susceptibility toward oral and dental health: a randomized controlled trial. Oman Med J 2018 Sep;33(5):423-428.
- 31. Arogundade FA, Sanusi AA, Hassan MO, Akinsola A. The pattern, clinical characteristics and outcome of ESRD in Ile-Ife, Nigeria: is there a change in trend? Afr Health Sci 2011 Dec;11(4):594-601.
- 32. Kurella Tamura M, Anand S, Li S, Chen SC, Whaley-Connell AT, Stevens LA, et al. Comparison of CKD awareness in a screening population using the Modification of Diet in Renal Disease (MDRD) study and CKD Epidemiology Collaboration (CKD-EPI) equations. Am J Kidney Dis 2011 Mar;57(3)(Suppl 2):S17-S23.
- 33. Shah A, Fried LF, Chen SC, Qiu Y, Li S, Cavanaugh KL, et al; KEEP Investigators. Associations between access to care and awareness of CKD. Am J Kidney Dis 2012 Mar;59(3)(Suppl 2):S16-S23.
- 34. Roomizadeh P, Taheri D, Abedini A, Mortazavi M, Larry M, Mehdikhani B, et al. Limited knowledge of chronic kidney disease and its main risk factors among Iranian community: an appeal for promoting national public health education programs. Int J Health Policy Manag 2014 Apr;2(4):161-166.
- 35. Khalil A, Abdalrahim M. Knowledge, attitudes, and practices towards prevention and early detection of chronic kidney disease. Int Nurs Rev 2014 Jun;61(2):237-245.
- 36. Plantinga LC, Tuot DS, Powe NR. Awareness of chronic kidney disease among patients and providers. Adv Chronic Kidney Dis 2010 May;17(3):225-236.
- 37. Fishbane S, Hazzan AD, Halinski C, Mathew AT. Challenges and opportunities in late-stage chronic kidney disease. Clin Kidney J 2015 Feb;8(1):54-60.
- 38. Davids MR, Eastwood JB, Selwood NH, Arogundade FA, Ashuntantang G, Benghanem Gharbi M, et al. A renal registry for Africa: first steps. Clin Kidney J 2016 Feb;9(1):162-167.
- 39. Osman MA, Okel J, Okpechi IG, Jindal K, Bello AK. Potential applications of telenephrology to enhance global kidney care. BMJ Glob Health 2017 May;2(2):e000292.
- 40. Bloomfield GS, Vedanthan R, Vasudevan L, Kithei A, Were M, Velazquez EJ. Mobile health for non-communicable diseases in Sub-Saharan Africa: a systematic review of the literature and strategic framework for research. Global Health 2014 Jun;10:49.
- 41. Scheffler E, Visagie S, Schneider M. The impact of health service variables on healthcare access in a low resourced urban setting in the Western Cape, South Africa. Afr J Prim Health Care Fam Med 2015 Jun;7(1):1-11.
- 42. Shaw BA, Spokane LS. Examining the association between education level and physical activity changes during early old age. J Aging Health 2008 Oct;20(7):767-787.
- 43. Green JA, Cavanaugh KL. Understanding the influence of educational attainment on kidney health and opportunities for improved care. Adv Chronic Kidney Dis 2015 Jan;22(1):24-30.
- 44. Cavanaugh KL, Wingard RL, Hakim RM, Eden S, Shintani A, Wallston KA, et al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 2010 Nov;21(11):1979-1985.
- 45. Stanifer JW, Turner EL, Egger JR, Thielman N, Karia F, Maro V, et al. Knowledge, attitudes, and practices associated with chronic kidney disease in Northern Tanzania: a community-based study. PLoS One 2016 Jun;11(6):e0156336.
- 46. Walker R, Marshall MR, Polashek N. Improving self-management in chronic kidney disease: a pilot study. Ren Soc Aust J 2013 Sep;9(3):116-125.
- 47. Jha V, Arici M, Collins AJ, Garcia-Garcia G, Hemmelgarn BR, Jafar TH, et al; Conference Participants. Understanding kidney care needs and implementation strategies in low- and middle-income countries: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int 2016 Dec;90(6):1164-1174.
- 48. Stengel B, Tarver-Carr ME, Powe NR, Eberhardt MS, Brancati FL. Lifestyle factors, obesity and the risk of chronic kidney disease. Epidemiology 2003 Jul;14(4):479-487.
- 49. Asif M. A brief study of toxic effects of some medicinal herbs on kidney. Adv Biomed Res 2012;1:44.
- 50. Ige SF, Salawu EO, Olaleye SB, Adeeyo OA, Badmus J, Adeleke AA. Onion (Allium cepa) extract prevents cadmium induced renal dysfunction. Indian J Nephrol 2009 Oct;19(4):140-144.
- 51. Kim HN, Kim SH, Song SW. Is alcohol drinking associated with renal impairment in the general population of South Korea? Kidney Blood Press Res 2014;39(1):40-49.
- 52. Menon V, Katz R, Mukamal K, Kestenbaum B, de Boer IH, Siscovick DS, et al. Alcohol consumption and kidney function decline in the elderly: alcohol and kidney disease. Nephrol Dial Transplant 2010 Oct;25(10):3301-3307.
- 53. Beyene KA, Sheridan J, Aspden T. Prescription medication sharing: a systematic review of the literature. Am J Public Health 2014 Apr;104(4):e15-e26.
- 54. Santos DB, Barreto ML, Coelho HL. Use of prescribed and non-prescribed medications among children living in poor areas in the city of Salvador, Bahia State, Brazil. Cad Saude Publica 2011 Oct;27(10):2032-2040.
- 55. Choueiri TK, Je Y, Cho E. Analgesic use and the risk of kidney cancer: a meta-analysis of epidemiologic studies. Int J Cancer 2014 Jan;134(2):384-396.
- 56. Ulasi II, Ijoma CK, Onwubere BJ, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in enugu, Nigeria. Int J Hypertens 2011 Jan;2011:869675.
- 57. Rauscher GH, Ferrans CE, Kaiser K, Campbell RT, Calhoun EE, Warnecke RB. Misconceptions about breast lumps and delayed medical presentation in urban breast cancer patients. Cancer Epidemiol Biomarkers Prev 2010 Mar;19(3):640-647.