A 32-year-old female presented to the emergency department with severe, unrelenting pain in her abdomen for two days accompanied by vomiting and gross abdominal distension. She had no history suggestive of gastric outlet obstruction, and signs of peritoneal irritation were absent. On examination, the patient was hemodynamically unstable. On palpation, the abdomen had a diffuse tympanitic note, and the Pouch of Douglas was distended, but tenderness was absent. An intravenous line was started immediately and after resuscitation investigations showed an arterial pH of 7.32, K+ = 2.7 mEq/L, and Na+ = 123 mEq/L with a leukocyte count of 16 500. A nasogastric tube was inserted, and about 100 cm3 of greyish semisolid fluid returned. A supine abdominal X-ray was done [Figure 1]. The patient soon developed massive hematemesis and rapidly progressed to shock from which she could not be revived.
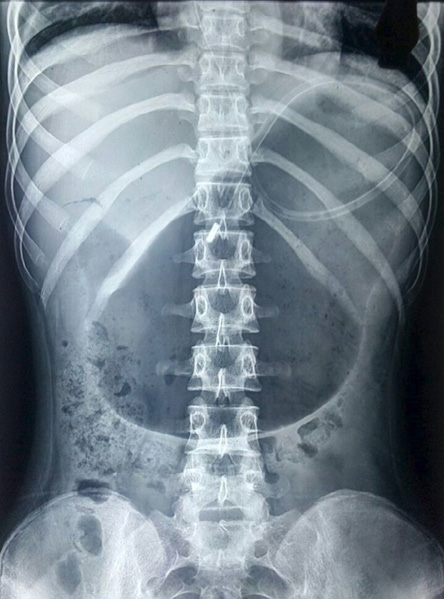
Figure 1: Supine abdominal X-ray of a 32-year-old female.
Question
- What is the diagnosis?
a. Acute pancreatitis.
b. Acute gastric dilatation.
c. Toxic megacolon.
d. Portal hypertensive gastropathy.
Answer
b. Acute gastric dilatation.
Discussion
Duplay first described acute gastric dilatation (AGD) in 1833.1 Generally, AGD occurs as a postoperative complication, but can also be seen in anorexia nervosa and bulimia, psychogenic polyphagia, trauma, electrolyte disturbances, and gastric volvulus.2 The pathogenesis of AGD is controversial; however, aerophagia due to the relaxation of the upper esophageal sphincter as a sequel to anesthesia and debilitation has been suggested.2 Emesis is the commonest symptom at presentation in more than 90% cases. The inability to vomit, diffuse abdominal distension, and pain are other common findings.3 On physical examination, the abdomen is found to be diffusely tympanitic with succussion splash, and a distended Pouch of Douglas on rectal examination. Plain abdominal radiographs can show a largely distended stomach with a gas fluid level. The most useful diagnostic investigation is an abdominal computed tomography scan.4 Often an endoscopy is required to determine the condition of the gastric mucosa and rule out mechanical obstruction. The rich vascular network of the stomach generally protects it from ischemia and necrosis.5 Thus if the diagnosis can be made early with prompt gastric decompression, normal endoscopy, and no signs of peritonitis, surgical intervention may be avoided.4 In cases of failure of conservative management or if gastric infarction with or without perforation is suspected, immediate laparotomy is mandatory followed by surgical decompression, and partial or total gastric resection depending on the findings. Delayed treatment and failure to recognize gastric necrosis or perforation in a case of AGD can have a high mortality rate of 80%.6
references
- Todd SR, Marshall GT, Tyroch AH. Acute gastric dilatation revisited. Am Surg 2000 Aug;66(8):709-710.
- 2. Byrne JJ, Cahill JM. Acute gastric dilation. Am J Surg 1961 Mar;101(3):301-309.
- 3. Chaun H. Massive gastric dilatation of uncertain etiology. Can Med Assoc J 1969 Feb;100(7):346-348.
- 4. Adson DE, Mitchell JE, Trenkner SW. The superior mesenteric artery syndrome and acute gastric dilatation in eating disorders: a report of two cases and a review of the literature. Int J Eat Disord 1997 Mar;21(2):103-114.
- 5. Jefferiss CD. Spontaneous rupture of the stomach in an adult. Br J Surg 1972 Jan;59(1):79-80.
- 6. Cogbill TH, Bintz M, Johnson JA, Strutt PJ. Acute gastric dilatation after trauma. J Trauma 1987 Oct;27(10):1113-1117.