Diabetes mellitus is one of the fastest growing non-communicable diseases globally. The Middle East is one of the regions with the highest diabetes indices.1 Of the top 20 countries with highest prevalence of diabetes, seven are from the Middle East and North Africa region. The prevalence of type II diabetes in patients aged 20–79 years in the UAE is estimated to be 17.3%.1 The mean healthcare expenditure per person with diabetes per year in the UAE is more than $5000 USD.1 Moreover, the economic burden of diabetes is expected to increase with development of diabetes complications. Data from the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) demonstrated that the incidence of diabetic complications is directly related to glycemic control. Furthermore, preliminary WESDR health outcomes data suggest that higher levels of glycemia are related to a decreasing quality of life.2
Previous studies have provided evidence of the power of good glycemic control to restrict the microvascular and macrovascular complications of diabetes.3,4 The results of the Diabetes Control and Complications Trial showed that intensive insulin therapy and improved glycemic control reduced diabetic complications in people with type I diabetes.5 Results of the U.K. Prospective Diabetes Study and the Kumamoto trial also support the relationship between glycemic control and diabetic complications in individuals with type II diabetes.6,7 Despite that, between 40% and 60% of patients worldwide still have poorly controlled diabetes.8–11
Attaining the benchmark of the American Diabetes Association (HbA1c < 7%) has always been a global challenge.9,12,13 Given the propagated cost of treating diabetes and its complications, very few countries have managed to report a positive trend in diabetes control.9,12,13
Despite the high prevalence of diabetes in the UAE, very few studies have evaluated diabetes control patterns over the last few years.14–18 In the UAE, all national citizens and expatriates (the majority of whom have health insurance) receive free medical treatment; a fact that raises the expectations of having a high percentage of patients with controlled diabetes status.
This study was conducted in Dubai Health Authority (DHA), the main governmental health sector in the emirate of Dubai in the UAE. DHA has 13 primary care centers that manage patients with diabetes, in addition there are three hospitals with specialized tertiary diabetes care departments.
Our primary aim was to assess the level of glycemic control across DHA points of care over the past five years (2012–2016). Additionally, we aimed to compare the differences in glycemic control between primary and tertiary centers, between nationalities, and different types of diabetes.
Methods
We conducted a retrospective analysis of the electronic medical records of all patients who attended the DHA primary and tertiary care centers from 2012 to 2016.
We analyzed all patients with an International Classification of Diseases (ICD) coding of type I and II diabetes, with or without complications. Since the data was retrospectively collected, we randomly selected any glycated hemoglobin (HbA1c) available during the fourth quarter in each year, which may arguably reflect the glycemic control of that particular year.
Patients were categorized based on their HbA1c into three groups: controlled (< 7%), uncontrolled (7–9%), and poorly controlled (> 9%) diabetes. Different levels of glycemic control were compared between the primary and tertiary services, UAE nationals versus expatriates, and type I versus type II diabetes. Moreover, those who were coded to have advanced cardiovascular or renal complications were categorized (as per American Diabetes Association recommendations) into less tight HbA1c cutoffs (7–7.5, 7.5–8, and > 8%). The different HbA1c categories were then compared between primary and tertiary care centers, and UAE nationals and expatriates.
Data was statistically described as mean and standard deviation, median and range, or frequencies (number of cases), and percentages as appropriate. Comparison of numerical variables between the study groups was made using Student t-test for independent samples in comparing two groups and one-way analysis of variance (ANOVA) test with post-hoc multiple two-group comparisons for comparing more than two groups. Within-group comparison between the different years was made using the repeated measures ANOVA test. For comparing categorical data, the Chi-square test was performed.
Table 1: Demographic distribution of the study population.
|
Males |
12 765 |
48.3 |
|
Females |
13 682 |
51.7 |
|
UAE nationals |
19 508 |
73.8 |
|
Expatriates |
6939 |
26.2 |
|
T1DM |
2625 |
9.9 |
|
T2DM |
23 822 |
90.1 |
|
Tertiary care |
10 967 |
41.5 |
UAE: United Arab Emirates; T1DM: type I diabetes mellitus; T2DM: type II diabetes mellitus.
Results
We reviewed 26 447 patients 73.8% (n = 19 508) were UAE nationals while the other nationalities accounted for 26.2% (n = 6939). The population was not equally distributed in gender with 51.7% females (n = 13 682) and 48.3% males (n = 12 765) [Table 1]. The overall mean HbA1c (across the DHA clinics) from 2012 to 2016 was 7.76%. Mean HbA1c among males was 7.68%, while in females, it was 7.78% (p = 0.046). Patients attending primary care clinics had a mean HbA1c of 7.64% compared to 7.68% for the tertiary care cohort. In our population, 37.7% achieved HbA1c < 7%, while the majority (42.0%) had HbA1c of 7–9%, and 20.3% had HbA1c > 9% [Figure 1].
Table 2: Mean HbA1c levels across the study duration and the percentages of HbA1c according to health care center type.
|
Overall |
7.653 |
7.803 |
7.723 |
7.769 |
7.899 |
|
Primary care |
7.639 |
7.780 |
7.714 |
7.609 |
7.775 |
|
Tertiary care |
7.671 |
7.831 |
7.732 |
7.968 |
8.093 |
|
p-value |
0.370 |
0.170 |
0.660 |
< 0.001 |
< 0.001 |
|
Total |
7.76 |
37.7 |
42.0 |
20.3 |
|
|
Tertiary care |
7.68 |
34.9 |
44.4 |
20.8 |
|
HbA1c: glycated hemoglobin.
Upon comparing primary versus tertiary care patients with HbA1c levels < 7, there were 40.8% and 34.9%, respectively [Table 2]. More than one-third of primary care patients (39.7%) had a mean HbA1c of 7–9%, compared to 44.4% in tertiary care. Interestingly, both primary and tertiary care patients had a comparable percentage of HbA1c > 9% which was 19.5% and 20.8%, respectively [Table 2].
UAE nationals had significantly higher mean HbA1c levels (7.84) compared to expatriates (7.65). Of the UAE nationals only 38.8% had HbA1c < 7% compared to 37.3% of expatriates [Figure 2].
Patients with type II diabetes had better glycemic control (HbA1c < 7%) than patients with type I diabetes; 16.0 and 40.7%, respectively [Figure 3]. Moreover, about 40.0% of patients aged 20–40 years and > 65 years achieved HbA1c < 7% in both groups [Figure 4].
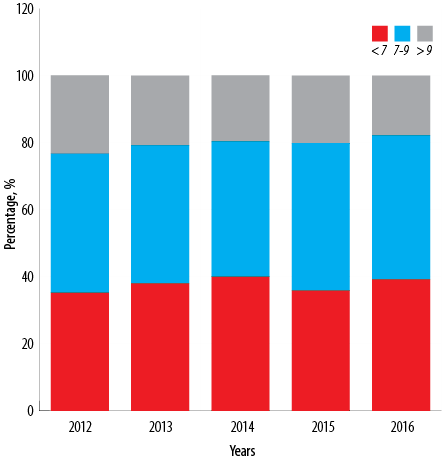
Figure 1: Proportions of glycated hemoglobin (HbA1c) levels from 2012 to 2016.
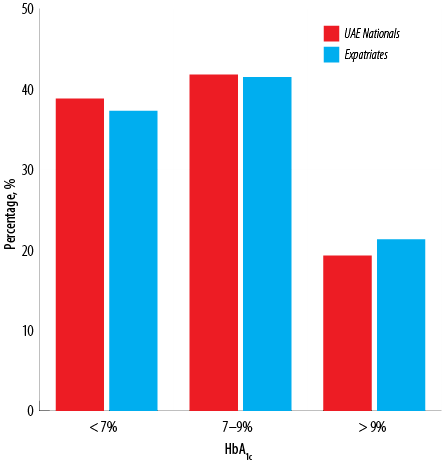
Figure 2: Mean glycated hemoglobin (HbA1c) levels between UAE nationals and expatriates.
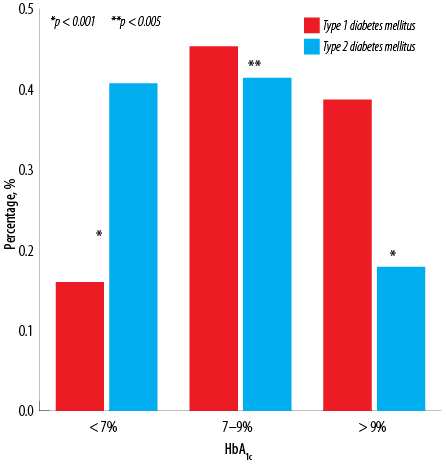
Figure 3: Comparison of glycated hemoglobin (HbA1c) levels between patients with type I and type II diabetes.
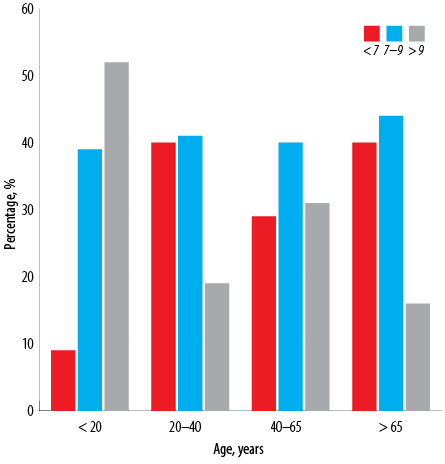
Figure 4: Categories of glycated hemoglobin (HbA1c) levels according to age.
Discussion
Achievement of glycemic control targets is the mainstay of diabetes management. This has been supported by numerous studies looking at the advantages of improved glycemic control in reducing complications related to diabetes.2–7
International guidelines such as the American Diabetes Association Standards of Medical Care19 and the European Association for the Study of Diabetes joint care statement20 have devised evidence-based recommendations on target diabetes glycemic control variables, allowing physicians across general practice and specialist centers to benchmark their practice. This was shown to be successful in improving overall critical quality indicators including HbA1c levels, blood pressure, and low-density lipoprotein at the primary care level in the OPTIMISE randomized, controlled trial.21
Globally, however, it is very difficult to achieve the appropriate level of HbA1c (< 7%) as per international guidelines. A recent meta-analysis that included 24 studies reporting on over 350 000 patients with diabetes from 20 countries, reported a pooled HbA1c target achievement rate of 42.8% (95% confidence interval CI: 38.1–47.5%) with a higher proportion of patients achieving the target in Europe and North America compared to the rest of the world.22 Our study shows that we are slightly below the average achievement internationally, with our percentage of patients on target at 37.7% on average over five years with an improving trend. The achievement of target HbA1c in patients with type II diabetes alone is 40.7%. However, we have the highest percentage of patients achieving target levels in the Middle East region, compared to Saudi Arabia (24.2%), Palestine (29.1%), Kuwait (19.2%), and Qatar (22.3%) although the number of patients included in these cross-sectional studies was significantly smaller, ranging from 305 to 652 patients.23–26 We are also the first to describe the trend in glycemic control over five consecutive years, with an overall trend towards improvement in the percentage of patients achieving target HbA1c from 35.2% in 2012 to 39.2% in 2016 (p < 0.001). This improvement could be attributed to improved physician awareness, standardization of services, and the availability of new therapies (such as the sodium glucose cotransporter inhibitor class of diabetes therapy), and improved glucometers including flash glucose monitoring. Most of these advances have occurred in tertiary care centers, which have also shown a more substantial trend towards improvement of glycemic control in patients over the years.
It is interesting to note that a larger percentage of patients attending primary care for follow-up of diabetes had achieved the target HbA1c value of < 7% compared to their counterparts attending tertiary care centers, with a total of 40.8% of the former group at target, compared to 34.9% of the latter. A possible explanation for this observation is that primary care centers tend to look after patients in the early phase of diabetes and those who are well controlled, while patients with type I diabetes and those with more complicated type II diabetes cases would be referred to specialist centers whereby an overall poorer glycemic profile could be expected at baseline. This is evident with the larger percentage of patients with an HbA1c of 7–9% at tertiary referral centers (44.4%), compared to 39.7% with a similar HbA1c level in primary care. A smaller, retrospective study done in the UAE at a tertiary referral center in Al Ain, reported a similar achievement rate of < 7% HbA1c with 38% of patients on target.14 Another study reported achievement of target HbA1c in only 23% of surveyed patients at a Dubai Hospital.18
A significant discrepancy was noted in the level of glycemic control achieved by patients aged 40–65 years, with only 29.0% being on target compared to those aged 20–40 and > 65 years with the number on target in both these groups being 40.0%. Of note, adolescents (< 20 years) generally had poor glycemic control with only 9% achieving target levels. It is worth mentioning that only 16% of patients with type 1 diabetes achieved the HbA1c target. There was no difference between the UAE nationals and expatriates in terms of the HbA1c control.
The retrospective nature of this study gives rise to some limitations. Reliance on the ICD coding alone may have veiled patients with diabetes who were coded under other diseases (missed cases). On the other hand, those who were identified on the basis of the ICD code are confirmed cases of diabetes, thus strengthening the validity of the study. As this was a large group inclusive of type I and type II patients of all ages and with any possible complications, the overall percentage of patients described achieving glycemic targets is affected by various variables, which may not reflect any one specific group. However, the breakdown of patients by age, nationality and diabetes type helps alleviate some of those issues.
Conclusions
To date, this is the largest study in the region evaluating the glycemic control of patients with diabetes. The optimum glycemic target was achieved by < 40% of patients. Glycemic control is still below the desired levels. However, there has been a trend of improvement in the last few years and we are achieving the international average target. Prompt and sustainable educational activities are needed to improve these goals. Further collaborative actions from clinical, educational, and strategic sectors are needed.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. International Diabetes Federation Diabetes Atlas. 8th ed; 2017.
- 2. Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. X. Four-year incidence and progression of diabetic retinopathy when age at diagnosis is 30 years or more. Arch Ophthalmol 1989 Feb;107(2):244-249.
- 3. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998 Sep;352(9131):837-853.
- 4. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000 Aug;321(7258):405-412.
- 5. Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, et al; Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993 Sep;329(14):977-986.
- 6. King P, Peacock I, Donnelly R. The UK prospective diabetes study (UKPDS): clinical and therapeutic implications for type 2 diabetes. Br J Clin Pharmacol 1999 Nov;48(5):643-648.
- 7. Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract 1995 May;28(2):103-117.
- 8. Bi Y, Zhu D, Cheng J, Zhu Y, Xu N, Cui S, et al. The status of glycemic control: A cross-sectional study of outpatients with type 2 diabetes mellitus across primary, secondary, and tertiary hospitals in the Jiangsu province of China. Clin Ther 2010 May;32(5):973-983.
- 9. Ong KL, Cheung BM, Wong LY, Wat NM, Tan KC, Lam KS. Prevalence, treatment, and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999-2004. Ann Epidemiol 2008 Mar;18(3):222-229.
- 10. Ezenwaka CE, Offiah NV. Differences in cardiovascular disease risk factors in elderly and younger patients with type 2 diabetes in the West Indies. Singapore Med J 2002 Oct;43(10):497-503.
- 11. Mastura IC, Chew BH, Lee PY, Cheong AT, Sazlina SG, Jamaiyah H, et al. Control and treatment profiles of 70,889 adult type 2 diabetes mellitus patients in Malaysia - a cross sectional survey in 2009. International Journal of Collaborative Research on Internal Medicine & Public Health 2011;3(1):98-113.
- 12. Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004 Jan;291(3):335-342.
- 13. Harris SB, Ekoé JM, Zdanowicz Y, Webster-Bogaert S. Glycemic control and morbidity in the Canadian primary care setting (results of the diabetes in Canada evaluation study). Diabetes Res Clin Pract 2005 Oct;70(1):90-97.
- 14. Afandi B, Malik A, Alkaabi J, El Houni A, Aziz F. Clinical diabetes care of patients with type 2 diabetes at a major tertiary care hospital in the United Arab Emirates 2015. Journal of Diabetes. Metabolic Disorders and Control 2015;2(1):7-12.
- 15. Afandi B, Ahmad S, Saadi H, Elkhumaidi S, Karkoukli MA, Kelly B, et al. Audit of a diabetes clinic at Tawam hospital, United Arab Emirates, 2004-2005. Ann N Y Acad Sci 2006 Nov;1084:319-324.
- 16. Reed RL, Revel AO, Carter A, Saadi HF, Dunn EV. A clinical trial of chronic care diabetic clinics in general practice in the United Arab Emirates: a preliminary analysis. Arch Physiol Biochem 2001 Jul;109(3):272-280.
- 17. Shehab A, Elnour A, Abdulle A. A clinical audit on diabetes care in patients with type 2 diabetes in Al-ain, United arab emirates. Open Cardiovasc Med J 2012;6:126-132.
- 18. Osenenko KM, Szabo SM, Qatami L, Korenblat Donato BM, Al Madani AA, Al Awadi FF, et al. Patterns of care and treatment target success among persons with type 2 diabetes mellitus in Dubai: a retrospective cohort study. Value Health Reg Issues 2015 Sep;7:87-93.
- 19. Targets G; American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes-2018. Diabetes Care 2018 Jan;41(Suppl 1):S55-S64.
- 20. Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycaemia in type 2 diabetes, 2015: a patient-centred approach. Update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 2015 Mar;58(3):429-442.
- 21. Hermans MP, Elisaf M, Michel G, Muls E, Nobels F, Vandenberghe H, et al; OPTIMISE International Steering Committee. Benchmarking is associated with improved quality of care in type 2 diabetes: the OPTIMISE randomized, controlled trial. Diabetes Care 2013 Nov;36(11):3388-3395.
- 22. Khunti K, Ceriello A, Cos X, De Block C. Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: A meta-analysis. Diabetes Res Clin Pract 2018 Mar;137:137-148.
- 23. Al Harbi TJ, Tourkmani AM, Al-Khashan HI, Mishriky AM, Al Qahtani H, Bakhiet A. Adherence to the American Diabetes Association standards of care among patients with type 2 diabetes in primary care in Saudi Arabia. Saudi Med J 2015 Feb;36(2):221-227.
- 24. Ali D, Abduelkarem AR, Shahwan M. Evaluation of factors associated with inadequate glycemic control and some other health care indicators among patients with type 2 diabetes in Ramallah, Palestine; 2013. p. 445-451.
- 25. Al-Taweel DM, Awad AI, Johnson BJ. Evaluation of adherence to international guidelines for treating patients with type 2 diabetes mellitus in Kuwait. Int J Clin Pharm 2013 Apr;35(2):244-250.
- 26. Issam Diab M, Julienne Johnson B, Hudson S. Adherence to clinical guidelines in management of diabetes and prevention of cardiovascular disease in Qatar. Int J Clin Pharm 2013 Feb;35(1):101-112.