Dissecting aneurysms (DAs) are uncommon arterial vascular lesions most commonly associated with the aorta.1 The occurrence of DA in the internal carotid artery (ICA) is exceedingly rare with an average incidence of 2.5–3 per 100 000.2–4 The pathogenesis of DA involves an arterial wall tear that leads to subintimal hematoma resulting in luminal narrowing, occlusion, aneurysmal dilatation, or vascular rupture.2,3 DA of the ICA may occur as a consequence of cervicocranial trauma, head and neck surgery, and other multifactorial etiology.2–5 In this report, we present a rare case of DA of the ICA occurring as a complication of facial bones trauma.
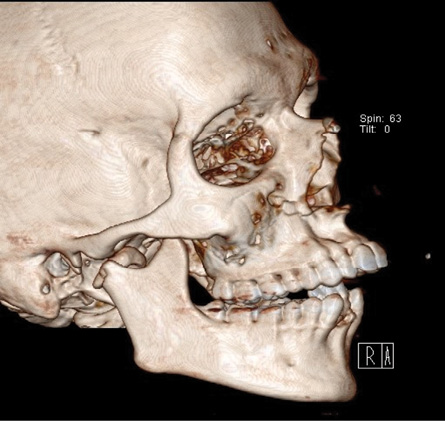
Figure 1: Three-dimensional facial bone computed tomography imaging showing Le Fort I maxillary fracture, medially displaced and fractured right condyle, and dentoalveolar fracture involving the lower anterior segment.

Figure 2: Selective angiogram of the right internal carotid artery (ICA) showing focal dissecting aneurysm of the extracranial part of the right
ICA (arrows).
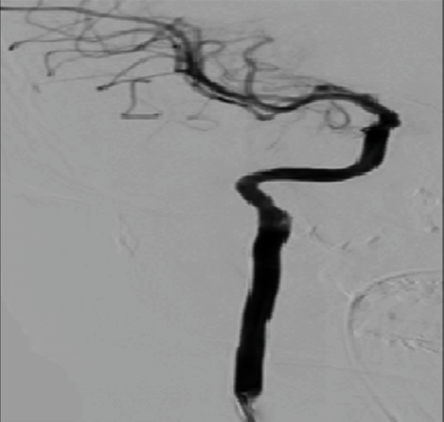
Figure 3: Intraoperative surgical exposure demonstrating dissecting aneurysm of the right internal carotid artery (arrow). Note the close anatomical relation of the lesion to the base
of skull.
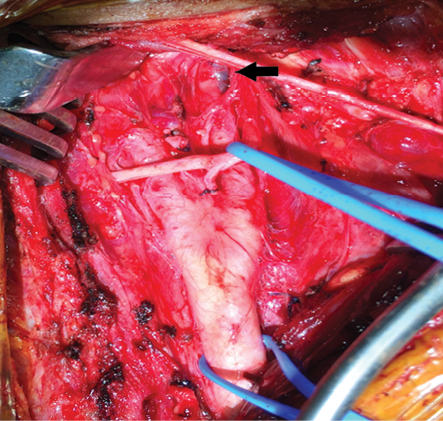
Figure 4: Post-right internal carotid artery stenting angiogram showing resolution of a dissecting aneurysm.
Case report
A 22-year-old male was intubated and admitted to the intensive care unit of Sultan Qaboos University Hospital, Oman, in March 2014 after being involved in a motor vehicle accident with multiple injuries, which included his lower limb, ribs, and maxillofacial fractures. Facial bone computed tomography (CT) showed lower anterior dentoalveolar fracture with lingual displacement, bilateral Le Fort I fractures of the maxillae, and medially displaced and fractured right condylar neck [Figure 1].
As emergency management, the patient underwent closed reduction of the dentoalveolar fracture and open reduction and internal fixation (ORIF) of the bilateral maxillary fractures under general anesthesia along with orthopedic surgical repair. Three days later, the patient underwent ORIF of the right condylar fracture. Following the completion of the ORIF, severe intraoperative bleeding was encountered from the posterior medial aspect of the condyle. All local measures of packing failed to arrest the bleeding, and the patient underwent emergency angiography to identify and treat the possible source of bleeding, which was anticipated to be from the right internal maxillary artery. However, the angiogram did not show any major source of bleeding in relation to the internal maxillary artery, but identified a large DA of the extracranial part of the right ICA [Figure 2]. The vascular surgeon attempted surgical repair of the identified DA. However, due to the additional intracranial extension of the lesion this was difficult [Figure 3]. At this time, no active bleeding was found from the surgical site of the right mandibular condyle. Accordingly, a decision was taken to arrange for repair using an endovascular arterial stent, thus avoiding ligation of the ICA. The wound was thus closed in layers.
Six days later, through the femoral approach, the patient underwent endovascular insertion of a 50 × 6 mm self-expandable covered arterial stent with no distal carotid embolic protection, which resulted in complete resolution of the vascular lesion with no complications [Figure 4]. At nine months follow-up, the patient showed satisfactory dental occlusion and mandibular movements with no vascular or cranial abnormalities.
Discussion
DAs are vascular pathologies defined by the existence of a hematoma in the arterial wall.1 In the head and neck region, there are reposts of involvement of the vertebral, cerebral, common carotid artery, and the ICA in DAs. Although involvement of the ICA in DAs is rare, the unilateral form is more common. However, bilateral presentations have also been reported.2,4,6,7
DAs of the ICA can occur spontaneously or in association with various etiological factors including craniomaxillofacial trauma, head and neck surgeries, hyperextension or hyperflexion of the neck, fibromuscular dysplasia, and connective tissue disorders such as Ehlers-Danlos and Marfan syndromes.5,8–10
Craniomaxillofacial fractures such as mandibular and/or maxillary fractures have been reported to be associated with the development of traumatic injuries of the ICA.9,11–13 Mundinger et al,11 looked at facial fracture patterns in association with ICA injuries. In their study, Le Fort I and subcondylar fractures were the only patterns showing an increased risk of injury to the ICA without specifying the nature of the involved vascular injury.11 In our case, the etiological factor leading to the development of DA of the ICA was facial trauma presenting as mandibular condyle and Le Fort I maxillary fractures, which is in line with published literature.11–13
The pathogenesis of DA starts with vascular injury resulting in blood penetration into the vessel wall causing interstitial hemorrhage and dissection. Accumulated blood between the tunica intima and the media results in arterial luminal narrowing. A dissection between the media and adventitia creates aneurysmal dilatation.2–4,9
The clinical presentation of DA involving the ICA can be mild and nonspecific. The literature reports that this form of DA formation following craniomaxillofacial fractures is often difficult to distinguish and lead to underdiagnosis.9,14 The clinical presentation can be immediate or occurring within the first 24 hours and includes ipsilateral facial pain, cervical and retinal ischemia, Horner’s syndrome, paralysis, or stroke.2,3,9
Many diagnostic modalities exist for the diagnosis of DA including ultrasonography, CT, magnetic resonance imaging, and conventional angiography, which is the gold standard in diagnosing arterial dissections.12 Angiography of a DA classically demonstrates irregular narrowing of the vessel lumen or aneurysmal dilatation.14 In this case, the conventional angiography revealed narrowing of the extracranial part of the ICA, thus confirming the diagnosis of DA.
Multiple screening guidelines are present to illustrate cerebrovascular injuries. These are used to screen for vertebral and carotid artery dissection and/or injury after blunt head and neck trauma. Biffl et al,15 described a grading scale for blunt carotid artery injuries in 1999. They found a 0.38% incidence of blunt carotid injuries with facial fractures being the most associated cause of injury to the carotid artery and present in 61% of cases.15
The management of ICA dissection is debatable but can be broadly divided into medical, surgical, and endovascular interventions.5,16 Medical management includes using anticoagulant and antiplatelet therapies to prevent cerebral embolization of the dissecting vessel and permanent occlusion of the tight stenosis.16 Surgical management involves vascular bypass, ligation, and resection and grafting of the damaged vessel.14,16 Endovascular stenting is a less invasive modality, which allows immediate recanalization and is associated with less complications.5,7,16 As the surgical repair failed in our case due to the unfavorable anatomical position of the lesion being close to the skull base, we were not in favor of ICA ligation due to the increased morbidity in this young patient and alternatively used an endovascular stent that resulted in complete resolution of the DA and a good outcome for the patient.
Conclusion
Craniomaxillofacial fractures may contribute to the development of DAs of the ICA, which may rupture, leading to a life-threating hemorrhage and an increase in morbidity and mortality. Utilization of conventional angiography helps to establish the diagnosis and provides a safe therapeutic option. All surgeons need to be cognizant of the rare possibility of a DA of the internal carotid as a complication of craniomaxillofacial injury.
Disclosure
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to thank Dr. Rajeev Kariyattil from Sultan Qaboos University Hospital for his kind input during the management of the reported case.
references
- 1. Tong J, Cheng Y, Holzapfel GA. Mechanical assessment of arterial dissection in health and disease: Advancements and challenges. J Biomech 2016 Aug;49(12):2366-2373.
- 2. Zetterling M, Carlström C, Konrad P. Internal carotid artery dissection. Acta Neurol Scand 2000 Jan;101(1):1-7.
- 3. Guillon B, Lévy C, Bousser MG. Internal carotid artery dissection: an update. J Neurol Sci 1998 Jan;153(2):146-158.
- 4. Scovell SD, Masaryk T. Carotid artery dissection. Semin Vasc Surg 2002 Jun;15(2):137-144.
- 5. Singh RR, Barry MC, Ireland A, Bouchier Hayes D. Current diagnosis and management of blunt internal carotid artery injury. Eur J Vasc Endovasc Surg 2004 Jun;27(6):577-584.
- 6. Kutlu NO, Saraç K, Yakinci C. Dissection of bilateral internal carotid arteries and occlusion of both vertebral arteries in a child patient. Comput Med Imaging Graph 2002 May-Jun;26(3):205-209.
- 7. Agarwala MK, Asad A, Gummadi N, Chidambaram S, Venkateswaralu J. Bilateral spontaneous internal carotid artery dissection managed with endovascular stenting - A case report. Indian Heart J 2016 Sep;68(Suppl 2):S69-S71.
- 8. Lleva P, Ahluwalia BS, Marks S, Sahni R, Tenner M, Risucci DA, et al. Traumatic and spontaneous carotid and vertebral artery dissection in a level 1 trauma center. J Clin Neurosci 2012 Aug;19(8):1112-1114.
- 9. Lo YL, Yang TC, Liao CC, Yang ST. Diagnosis of traumatic internal carotid artery injury: the role of craniofacial fracture. J Craniofac Surg 2007 Mar;18(2):361-368.
- 10. Carvalho KS, Edwards-Brown M, Golomb MR. Carotid dissection and stroke after tonsillectomy and adenoidectomy. Pediatr Neurol 2007 Aug;37(2):127-129.
- 11. Mundinger GS, Dorafshar AH, Gilson MM, Mithani SK, Manson PN, Rodriguez ED. Blunt-mechanism facial fracture patterns associated with internal carotid artery injuries: recommendations for additional screening criteria based on analysis of 4,398 patients. J Oral Maxillofac Surg 2013 Dec;71(12):2092-2100.
- 12. Kelts G, Maturo S, Couch ME, Schmalbach CE. Blunt cerebrovascular injury following craniomaxillofacial fractures: A systematic review. Laryngoscope 2017 Jan;127(1):79-86.
- 13. Vranis NM, Mundinger GS, Bellamy JL, Schultz BD, Banda A, Yang R, et al. Extracapsular mandibular condyle fractures are associated with severe blunt internal carotid artery injury: analysis of 605 patients. Plast Reconstr Surg 2015 Oct;136(4):811-821.
- 14. Yang WG, Chen CT, de Villa GH, Lai JP, Chen YR. Blunt internal carotid artery injury associated with facial fractures. Plast Reconstr Surg 2003 Feb;111(2):789-796.
- 15. Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: implications of a new grading scale. J Trauma 1999 Nov;47(5):845-853.
- 16. Martinelli O, Venosi S, BenHamida J, Malaj A, Belli C, Irace FG, et al. Therapeutical options in the management of carotid dissection. Ann Vasc Surg 2017 May;41:69-76.