Extracorporeal shockwave lithotripsy (ESWL) was first introduced in 1980 by Chaussy et al.1 It has since become a preferred treatment modality for uncomplicated renal and ureteral stone < 20 mm in diameter, as it is safe and non-invasive.2–5 After the introduction of original first generation electrohydraulic lithotripter, numerous modifications have been made in subsequent models. These modifications made the procedure more comfortable and tolerable for patients without anesthesia, at the expense of less energy delivery and, therefore, lower success rates and higher retreatment rates.6–8 Studies have shown that the Storz Modulith SLX-F2 lithotripter is clinically effective in the management of solitary renal and ureteral stones.9,10
The success rate of ESWL has a wide variation ranging from 46% to 91%.11–18 The results of ESWL are measured depending on the stone fragmentation and clearance, which is influenced by some predicting factors, such as stone size, stone location, skin-to-stone distance (SSD), stone composition, severity of obstruction, urinary tract anatomy, obesity, and ESWL machine type.19–28 The chemical composition of urinary calculi in vivo has been found to be the main factor in determining the outcome of ESWL.29,30 These days, non-contrast computed tomography (NCCT) has become the diagnostic modality of choice to evaluate urolithiasis and its ability to detect density differences as low as 0.5, thus helping in determining the composition and fragility of urinary stones and the outcome of ESWL.24,31–33
Although ESWL is a non-invasive and safe procedure compared to other treatment modalities, it may also cause complications such as hemorrhage, steinstrasse, renal hematoma, infection, and flank pain.34–37 In cases where ESWL fails, the unnecessary exposure of renal parenchyma to shock waves may lead to complications and further alternative treatments leading to additional medical expenses.25,38 Therefore, it is important to investigate the predictors influencing ESWL outcome to decide the treatment strategy for preventing unnecessary complications and the cost and treatment time after the diagnosis of urinary stone.
Methods
We conducted a retrospective review for adult patients with renal or ureteric stones, treated with ESWL at Armed Forces Hospital (AFH), Oman, between January 2015 and December 2016. The inclusion criteria were radiopaque stone size > 4 mm, on the pretreatment plain abdominal X-ray of the kidney, ureter, and bladder (KUB). Pregnant women and patients with uncontrolled coagulopathy, ongoing urinary tract infection, stone secondary to anatomical obstruction, congenital anatomical abnormalities, any previous renal surgery or ESWL on the ipsilateral side, and gross obesity body mass index ≥ 35 kg/m2) were excluded from the study. The case summary, hematological, biochemical, radiological investigations, and follow-ups were charted. All the patients underwent X-ray KUB, ultrasonography, and NCCT KUB for initial diagnosis.
Of the 294 patients treated, 59 were not included in the study (29 patients due to non-availability of NCCT, 30 lost to follow-up, and the rest as per exclusion criteria). Therefore, the final analysis, results, and conclusions were based on 235 patients. NCCT was used to determine stone characteristics such as size, location, laterality, density, and SSD.24 In AFH, NCCT KUB was performed using Philips Brilliance 64 MSCT with slice thickness 3 mm from the diaphragm to pubic symphysis. The largest dimension of the stone with soft tissue window in coronal view represented the stone size. Hounsfield units (HUs) of stones were calculated by mean attenuation of three consistent (area 0.02 cm2), non-overlapping regions of interest chosen from stones in bone windows.39 Measurement of SSD on axial computed tomography view was done by calculating the mean value of three distances from the center of the stone to the skin surface (horizontally, perpendicular and at 45 degrees between the first two directions using radiographic calipers for renal and upper ureteric stones).17 SSD for lower ureteric stone was calculated by measuring the distance between the center of the stone to the skin surface of anterior abdominal wall, at right angle to the horizontal plane. A double J stent was inserted in patients with stones > 15 mm in size, high-grade hydronephrosis (grades 3 and 4 defined by The Society of Fetal Ultrasound), and impaired renal functions before ESWL.
The patients in the study were subjected to ESWL using Storz Modulith SLX-F2, third generation lithotripter with electromagnetic shockwave source after written and informed consent. ESWL was done under pethidine sedation. The procedure was performed under the supervision of the same urologist. Under intermittent fluoroscopic or ultrasonic guidance, the targeted stone was struck by a maximum of 4000 shocks per session at the rate of 60–90 shocks per minute with gradually increasing intensity to level 4 and 4.5 to 7 for renal stones and ureteric stones, respectively. Stone localization was achieved by fluoroscopy or a combination of ultrasound and fluoroscopy. Reassessment of stones was done after 2–3 weeks using X-ray KUB and ultrasonography to assess the fragmentation. Those patients with no or insignificant stone fragmentation (fragment > 4 mm) were given another session of ESWL. After the first ESWL session, patients were followed-up for three months for the outcome of stone clearance. At the end-point, patients were evaluated with X-ray KUB, ultrasonography, and/or NCCT KUB. Stone clearance, stone fragmentation, number of ESWL sessions, requirement of auxiliary procedure, and complications were documented. Treatment was defined as successful in cases of complete clearance of ureteric stones and stone-free (complete clearance or the presence of asymptomatic, non-infectious, and non-obstructive fragments ≤ 4 mm) for renal stones. Treatment failure was considered in case of no fragmentation or residual stone fragments > 4 mm after three sessions of ESWL or if the patient required another mode of treatment.
At end-point evaluation, patients were categorized into success and failure groups. Data were described using frequency, percent, and mean score. To test the statistical significance of the relationship between ESWL outcome and the factors affecting it, data were analyzed using chi-square test, independent samples t-test, and correlation. Thereafter, the significantly associated variables were tested with multivariate logistic regression analysis to identify the independent predictors of treatment failure. A two-tailed level of significance was set at 0.05. All statistical analysis was carried out using SPSS Statistics (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.).
Results
A total of 235 patients (188 males and 47 females) with renal or ureteric stones who received ESWL treatment from January 2015 to December 2016 were analyzed.
ESWL was successful in 79.1% (186/235) of patients and failed in 20.9% (49/235). The baseline demographic characteristics and predictors of all patients are presented in Table 1. In univariate analysis, as shown in Table 2, patient’s age and stone laterality were not significantly different in the two groups. However, differences in gender, stone size, stone site, stone density, SSD, number of ESWL sessions, number of shocks required, and patients with stents were statistically significant.
Table 1: Patients demographic characteristics and baseline parameters.
|
Patients, n |
235 |
|
Age, mean ± SD, years |
37.6 ± 10.8 |
|
Gender |
|
Male
Female |
188 (80.0)
47 (20.0) |
|
Stone laterality |
|
|
Right
Left |
106 (45.1)
129 (54.9) |
|
Stone size, mean ± SD, mm |
9.0 ± 2.5 |
|
< 10
> 10 |
179 (76.2)
56 (23.8) |
|
Stone location |
|
|
Upper calyx
Middle calyx
Lower calyx
Pelvis
Upper ureter
Lower ureter |
5 (2.1)
15 (6.4)
22 (9.4)
48 (20.4)
67 (28.5)
78 (33.2) |
|
Stone density, mean ± SD, HU |
859.0 ± 241.0 |
|
SSD, mean ± SD, mm |
106.0 ± 22.0 |
|
Stent |
|
|
Present
Absent |
48 (20.4)
187 (79.6) |
|
ESWL sessions, mean ± SD |
1.8 ± 0.9 |
SD: standard deviation; HU: hounsfield unit; SSD: skin-to-stone distance; ESWL: extracorporeal shockwave lithotripsy.
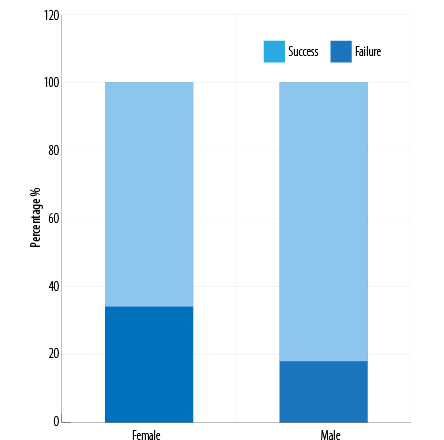
Figure 1: Extracorporeal shockwave lithotripsy outcome according to gender.
Table 2: Univariate analysis of the factors affecting outcome of extracorporeal shockwave lithotripsy.
|
Patients, n |
186 (79.1) |
49 (20.9) |
|
|
Age, mean ± SD, years |
37.3 ± 10.5 |
38.8 ± 11.6 |
0.385 |
|
Gender |
|
|
|
|
Male
Female |
155 (82.4)
31 (66.0) |
33 (17.6)
16 (34.0) |
0.017* |
|
Stone laterality |
|
|
|
|
Right
Left |
86 (81.1)
100 (77.5) |
20 (18.9)
29 (22.5) |
0.523 |
|
Stone size, mm |
|
|
|
|
< 10
> 10 |
150 (83.8)
36 (64.3) |
29 (16.2)
20 (35.7) |
0.004* |
|
Stone location |
|
|
0.040 |
|
Upper calyx |
5 (100.0) |
0 (0.0) |
|
|
Middle calyx |
12 (80.0) |
3 (20.0) |
|
|
Lower calyx |
17 (77.3) |
5 (22.7) |
|
|
Pelvis |
36 (75.0) |
12 (25.0) |
|
|
Upper ureter |
46 (68.7) |
21 (31.3) |
|
|
Lower ureter |
70 (89.7) |
8 (10.3) |
|
|
Stone density, mean ± SD, HU |
807.5 ± 213.8 |
1052.7 ± 242.6 |
< 0.001* |
|
SSD, mean ± SD, mm |
103.9 ± 21.3 |
111.6 ± 22.4 |
0.027* |
|
Stent, n (%) |
|
|
|
|
Present
Absent |
23 (47.9)
163 (87.2) |
25 (52.1)
24 (12.8) |
< 0.001* |
|
Number of ESWL sessions, mean ± SD |
1.6 ± 0.6 |
2.6 ± 1.3 |
< 0.001* |
*Statistically significant.
SD: standard deviation; HU: hounsfield unit; SSD: skin-to-stone distance.
The overall complication rate was 26.4% (62/235). Most complications were minor with the commonest being loin pain seen (18.7%; 44/235). However, in 6.0% (14/235) of patients, severe renal or ureteric colic was observed mandating a visit to the accident and emergency department, of which 3.4% (8/235) required inpatient care for pain control. Steinstrasse occurred in four patients, of which two were treated with ureteroscopy. The other two patients were treated conservatively with a further ESWL session leading to successful stone fragmentation. Patients with dysuria were 17.0% (40/235), of which symptomatic bacteriuria was diagnosed in three patients. There was gross hematuria observed in 11.9% (28/235) of patients, which improved spontaneously within two to three days. No major complications, such as hemorrhage (which could have necessitated transfusion), severe infection, or injury to other organs, occurred in any patients.
In the multivariate logistic regression analysis, only two variables were found to statistically significantly predict the failure of ESWL; sex and stent. Compared to males, females had three-times higher risk for ESWL failure (odds ratio (OR) = 3.213; 95% confidence interval (CI): 1.194–8.645; p = 0.021). Logistic regression analysis also showed a higher failure rate when stent was used (OR = 6.358; 95% CI: 2.228–18.143; p = 0.001).
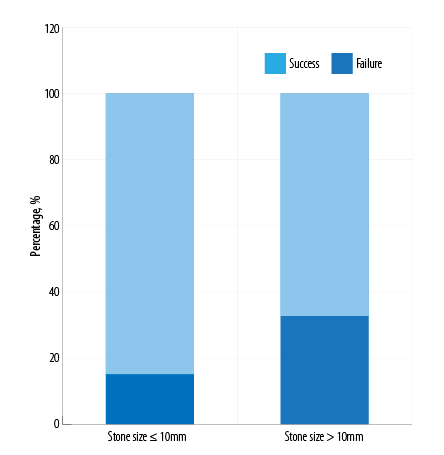
Figure 2: Extracorporeal shockwave lithotripsy outcome according to stone size.
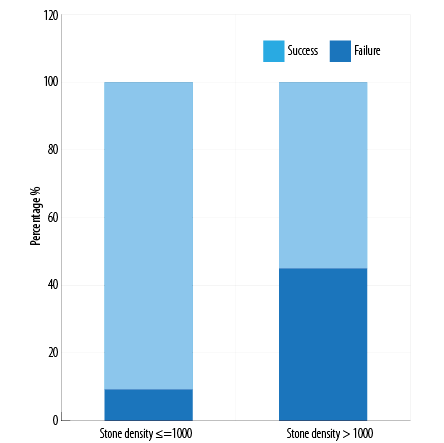
Figure 3: Extracorporeal shockwave lithotripsy outcome according to stone density.
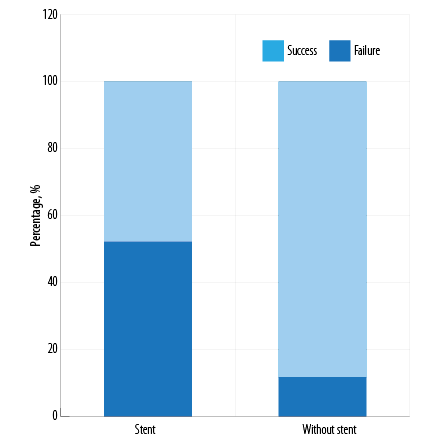
Figure 4: Extracorporeal shockwave lithotripsy outcome according to presence or absence of a double J stent.
The success rate of ESWL in males was 82.4% compared to 66.0% in females [Figure 1] and this result was statistically significant in both univariate and multivariate analysis.
Success rate of treatment in stones ≤ 10 mm was 83.8% compared to that of only 64.3% in stone > 10 mm [Figure 2] with p-value of 0.004.
A stone free rate of 56.2% was observed in patients with stones > 1000 HU density compared to 87.7% with a stone density ≤ 1000 HU [Figure 3].
Inferior ESWL outcome was observed in patients with stent. Only 47.9% of patients with stent showed good response to treatment, while 87.2% without stent had notable treatment benefit [Figure 4] with a p-value < 0.001.
Discussion
Since the introduction of ESWL in 1980, it has become an established and preferred treatment for uncomplicated renal and ureteral stone (< 20 mm in diameter) as it is safe as well as non-invasive.1–5
The success rate of ESWL varies from 46% to 91% and is measured in terms of stone fragmentation and clearance.11–18 Previous studies have demonstrated that predicting factors such as stone size, stone location, SSD, stone density, severity of obstruction, urinary tract anatomy, obesity, and type of ESWL machine can have an influence on the success rate of ESWL.21–28 We evaluated some of the factors affecting the outcome of ESWL as well as safety of treatment and observed a success rate of 79.1%.
Many studies have discussed factors affecting outcome of ESWL, but only few have considered age of any significance. One study of 3023 patients with renal and ureteric calculi treated with ESWL revealed that older patients had a significantly poorer stone-free rate.11 Another multivariate analysis of 2954 patients with renal stones treated with ESWL, revealed that patients aged > 40 years had significantly poorer stone-free rate.19 However, another study by same group on ureteric stones found that age did not affect ESWL outcome.40
In our study, age was not a significant factor affecting the outcome of ESWL. However, only 10 patients were above the age of 60. The reason for the possible poorer stone-free rate of renal calculi in elderly patients is unknown. However, age-related sclerotic kidney may affect the acoustic impedance and lower efficacy of ESWL. Further studies are needed to confirm age as a predictor of ESWL outcome.
Many studies have shown that gender is not a significant predictor of ESWL outcome. A retrospective study of 145 patients with renal stones treated with ESWL reported a success rate of 47.25% in males (43/91) and 50% (27/54) in females, which was not statistically significant.24 A study of 153 patients with ureteric stones treated with ESWL reported 83.33% (75/90) success in males compared to 82.54% (52/63) in females, which was also not statistically significant.21
In the present study, success rate of ESWL in males was 82.4% compared to 66.0% success in females and this result was statistically significant in both univariate and multivariate analysis.
Our study reports gender as a predicting factor of ESWL success, which is not in agreement with previous studies. We found the threshold for pain in females was lower compared to males. Many of our female patients could not tolerate higher energy shockwave during treatment and some presented to the emergency department with pain after their first session of ESWL, which eventually needed admission and another treatment modality. All these factors might have influenced lower success rate in females. Considering the limitations of this study, another prospective study is needed to confirm gender as predictor of failure of ESWL treatment.
Previous studies have shown that stone size is a significant predictor of ESWL treatment success. The larger the size of stone, the higher is the risk of ESWL failure. In a study of 2954 patients with renal stones, the authors observed a success rate of 89.7% for stones < 15 mm and of 78% for stones >15 mm (p < 0.001).19 In another study of 427 patients with renal stones, the success rate of ESWL for stones ≤ 10 mm was 90% and 70% for stones > 10 mm (p < 0.050).20
Stone size was also a significant predictor of ESWL outcome for ureteral stones. In a prospective study of 130 patients, the overall ESWL treatment success rate was 94.6%, while it was only 77.7% for stones > 15 mm. The authors also noted that the number of ESWL sessions increased with increasing stone size.41 Another retrospective study of 153 patients observed a success rate of 90.2% for stones ≤ 10 mm and 68.6% for stones > 10 mm.21 In the same study, multivariate analysis revealed that stone size was an independent predictor of failure of ESWL in each group (stone size ≤ 10 mm; OR = 50.005; 95% CI: 6.207–402.852; p = 0.013 and stone size > 10 mm; OR = 19.718; 95% CI: 1.600–243.005; p = 0.020).
Similarly, in our study stone size was one of the important factors determining ESWL success. Success rate of treatment in stones ≤ 10 mm was 83.8% (150/179) compared to that of only 64.3 (36/56) in stones > 10 mm (p = 0.004). A larger stone required a greater mean number of ESWL sessions for successful fragmentation. Stones ≤ 10 mm required 1.4 mean sessions while stones > 10 mm required 2.1 mean sessions. The mean number of shocks required for fragmentation of stones ≤ 10 mm were 5940.3 whereas 8301.5 shocks were required for stones > 10 mm. A positive correlation between the stone diameter (in mm) and the number of shock waves delivered was noted (r = 0.414; p = 0.000). Stone size was a significant predictor of ESWL success in univariate analysis; however, it was not found to be an independent predictor in multivariate analysis.
Calyceal stones have poor outcome with ESWL treatment compared to renal pelvic and ureteral stones, whereas lower pole renal calculi have poorer results with ESWL compared to middle and upper pole calculi.20
The role of ESWL treatment for lower calyceal stones has always been controversial. Various studies have observed a variable free rate for lower pole stones. One study showed that the success of ESWL treatment was only 47% in the lower calyceal stone compared to that of 79% for other site stones (chi-square = 6.3, df =1, p = 0.012).22 However, some studies favor ESWL treatment of lower calyceal stone, especially for low burden stones. A stone-free rate of 84% for lower calyceal stones between 5 to 15 mm with piezoelectric ESWL has been documented.42 A recent study revealed a stone-free rate of 75% for lower calyceal stone (size ranging from 10–20 mm) with ESWL treatment.43
We found stone site was a significant predictor of ESWL outcome. We compared the success rate of lower calyceal stones with stones at other sites. The success rate of ESWL for lower calyceal stones was 77.3% compared to 79.3% for stones at all other sites (p = 0.786). Patients with lower calyceal stones ≤ 10 mm in size had a success rate of 93.8% (15/16) compared to stones > 10 mm in size where the success rate was noted to be 33.3% (2/6). The clearance of the fragments was lower due to the unfavorable spatial anatomy of the lower pole collecting system.1 As ESWL is a non-invasive modality, it can still be offered for lower calyceal stones with low burden and favorable anatomy.
Recently, many studies have shown that the measurement of mean stone density by NCCT plays an important role in predicting ESWL success. In a prospective study of 120 patients, a stone density > 1000 HU was an independent predictor of ESWL failure (p = 0.020).44 Evidence from prospective study noted a stone-free rate for stones of < 970 HU was 96% versus 38% for stones of ≥ 970 HU (p = 0.001) and identified linear relationship between the stone density and ESWL success rate.25
Our study supports the above findings. We observed a stone-free rate of 56.2% in patients with stones > 1000 HU density compared to that of 87.7% with a stone density ≤ 1000 HU. Thus by calculating stone density with NCCT, one can predict the ESWL outcome and decrease the cost of management by reducing failure rate and number of ESWL sessions.
It has been noted in previous studies that the failure of ESWL is related to greater SSD. The mean SSD for ESWL success was 8.12±1.74 cm against 11.53±1.89 cm in the ESWL failure group (p < 0.010).39 In another study, the mean SSD in the stone free group was 83.3±21.9 mm compared to the residual stone group where the mean SSD was 107.7±28.9 mm (p < 0.050) and a multivariate regression analysis revealed that SSD was the only significant independent predictor of treatment outcome.27
In our study, the success group showed a mean SSD of 103.9±21.3 cm while the mean SSD in the failure group was 111.6±22.4 cm with a p-value of 0.027. Our study also demonstrated that SSD was a predictor of ESWL failure in univariate analysis, but the similar effect was not observed on multivariate analysis.
The use of a double J stent prior to ESWL treatment is rather controversial. Numerous studies have shown the use of double J stents is not much benefit prior to ESWL treatment. A prospective randomized study also revealed that the use of double J prior to ESWL did not improve treatment outcome.45 The authors reported a three-month stone-free rate of 88% in the stented group and 91% in the unstented group. Another study also concluded that the presence of ureteric stent resulted in a higher rate of ESWL failure.46 A comparative cross-sectional study noticed that pre-ESWL double J stenting for a 2 cm±2 mm renal stone reduces the risk of renal colic and obstruction, but does not reduce formation of steinstrasse or infective complications. The same study also noticed the cost of the treatment doubled in the stented group, which is an important factor in the authors’ country (Pakistan).47
Our study supports the findings of previous studies. Our study observed inferior ESWL outcome in patients with stent. Only 47.9% of patients with stent showed good response to treatment, while 87.2% without stent had notable treatment benefit (p < 0.001).
Stent was found to be independent predictor of ESWL failure in multivariate analysis. A higher failure of ESWL could be due to several difficulties such as difficulty in targeting, energy loss, and effect of the stent on peristalsis of ureter leading to reduced clearance of fragments. In our study, an indication for stenting was the presence of a stone > 15 mm in diameter. Considering the findings of previous studies and this study, routine stenting for stones < 20 mm should not be recommended as it does not prevent the formation of steinstrasse or the incidence of infective complications and might even lead to decreased stone clearance. However, it can be used in cases of sepsis and in patients with deteriorating renal function due to obstruction or with intolerable pain.2,46,47
A series of minor complications can occur after ESWL. A prospective study of 3241 patients treated with ESWL reported 4075 common complications, including renal colic (40%), gross hematuria (32%), steinstrasse (24.2%), symptomatic bacteriuria (9.7%), and perirenal hematoma or subclinical subcapsular haematoma (4.6%).48 All complications were managed conservatively or with minimal intervention. Another study noted an overall complication rate of 38.7%, which included all minor complications and were treated conservatively.34
The overall complication rate in this study was 26.4%. All complications were minor, including loin pain (18.7%), gross hematuria (11.9%), and steinstrasse (1.7%). Patients with dysuria were 17.0%, of which symptomatic bacteriuria was diagnosed in 1.3% of patients. No major complications occurred in any patient, such as hemorrhage (which could have necessitated transfusion), severe infection, or injury to other organs. ESWL is not completely free from major complications such as massive retroperitoneal hemorrhage, renal, or other organs injury. However, each of these complications can be prevented by respecting contraindications, recognition, and correction of concomitant diseases or infection, and using ESWL in the most efficient and safe way.34,48
Some of the limitations of the present study are mentioned herewith. We conducted a retrospective review and included a small number of patients. To reduce expected selection bias, a urologist was blinded to the results of ESWL, who assessed the predictors by NCCT. The measurement of the stone size was done in accordance with maximum diameter and not as per the surface area. Plain radiography and ultrasonography was used instead of NCCT for follow-up protocol to confirm treatment success. Stone composition has significant influence on outcome of ESWL, which was not evaluated. Chemical analysis of the retrieved stone fragment was not done. The patients with ureteral stents were not randomized prior to ESWL into stented and non-stented groups. However, the study provides strong evidence that patient’s gender, stone size, stone site, stone density, SSD, and use of double J stent affect the ESWL outcome, which can be very useful for patient selection to improve ESWL outcomes to save time and treatment costs.
Conclusion
This single institution experience, renal and ureteric stones treatment with ESWL showed good results. Any single potential predictive factor cannot determine likely outcome of ESWL treatment individually. Therefore, modern approach should consider all the predictors collectively. Failure of ESWL was observed to more in the case of females, stone size > 10 mm, stone density > 1000 HU, and patient with stents. Considering the limitations of this study, development of a nomogram on the basis of prospective randomized studies, may help to further improve patient selection and treatment outcome, thus decreasing the time and cost of treatment by reducing the failure rate.
Disclosure
The authors declared no conflict of interest. No funding was received for this study.
Acknowledgements
Special thanks to Dr Jyoti Shinde, Dr Upma Pathak, and Mr. Mahesh Ramamoorthy for their support during this article compilation and completion. Our patients who underwent extracorporeal lithotripsy deserve my unbounded gratitude.
references
- 1. Chaussy C, Brendel W, Schmiedt E. Extracorporeally induced destruction of kidney stones by shock waves. Lancet 1980 Dec;2(8207):1265-1268.
- 2. Bach C, Buchholz N. Shock wave lithotripsy for renal and ureteric stones. Eur Urol Suppl 2011;10:423-432.
- 3. Akal HR. The role of extracorporeal shock wave lithotripsy in the treatment of upper ureteral stone disease. Thi-Qar Medical Journal. 2011;5(3):16-27.
- 4. Labanaris AP, Kühn R, Schott GE, Zugor V. Perirenal hematomas induced by extracorporeal shock wave lithotripsy (ESWL). Therapeutic management. Scientific World Journal 2007 Sep;7:1563-1566.
- 5. Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck AC, Gallucci M, et al. American Urological Association Education and Research, inc. and European Association of Urology. Guideline for the management of ureteric calculi. Eur Urol 2007;52(6):1610-1631.
- 6. Rassweiler JJ, Tailly GG, Chaussy C. Progress in lithotriptor technology. EAU Update Series. 2005;3:17-36.
- 7. Egilmez T, Tekin MI, Gonen M, Kilinc F, Goren R, Ozkardes H. Efficacy and safety of a new-generation shockwave lithotripsy machine in the treatment of single renal or ureteral stones: Experience with 2670 patients. J Endourol 2007 Jan;21(1):23-27.
- 8. Köhrmann KU, Rassweiler JJ, Manning M, Mohr G, Henkel TO, Jünemann KP, et al. The clinical introduction of a third generation lithotriptor: Modulith SL 20. J Urol 1995 May;153(5):1379-1383.
- 9. Chandrapal J, Tang A, Navetta A, Trojan B, Haynes A, de Riese W, et al. Single-centre experience with the Dual-Focus Storz Modulith SLX-F2 lithotripter: a retrospective study. World Journal of Nephrology and Urology 2014;3(1):7-17.
- 10. Zehnder P, Roth B, Birkhäuser F, Schneider S, Schmutz R, Thalmann GN, et al. A prospective randomised trial comparing the modified HM3 with the MODULITH® SLX-F2 lithotripter. Eur Urol 2011 Apr;59(4):637-644.
- 11. Abe T, Akakura K, Kawaguchi M, Ueda T, Ichikawa T, Ito H, et al. Outcomes of shockwave lithotripsy for upper urinary-tract stones: a large-scale study at a single institution. J Endourol 2005 Sep;19(7):768-773.
- 12. Al- Dabbagh AA. Extracorporeal shock wave lithotripsy for the treatment of urolithiasis. Medical Journal of Babylon. 2009;6(2):263-267.
- 13. Albala DM, Assimos DG, Clayman RV, Denstedt JD, Grasso M, Gutierrez-Aceves J, et al. Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J Urol 2001 Dec;166(6):2072-2080.
- 14. Coz F, Orvieto M, Bustos M, Lyng R, Stein C, Hinrichs A, et al. Extracorporeal shockwave lithotripsy of 2000 urinary calculi with the modulith SL-20: success and failure according to size and location of stones. J Endourol 2000 Apr;14(3):239-246.
- 15. Pace KT, Ghiculete D, Harju M, Honey RJ; University of Toronto Lithotripsy Associates. Shock wave lithotripsy at 60 or 120 shocks per minute: a randomized, double-blind trial. J Urol 2005 Aug;174(2):595-599.
- 16. Park H, Park M, Park T. Two-year experience with ureteral stones: extracorporeal shockwave lithotripsy v ureteroscopic manipulation. J Endourol 1998 Dec;12(6):501-504.
- 17. Perks AE, Schuler TD, Lee J, Ghiculete D, Chung DG, D’A Honey RJ, et al. Stone attenuation and skin-to-stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. Urology 2008 Oct;72(4):765-769.
- 18. White W, Klein F. Five-year clinical experience with the Dornier Delta lithotriptor. Urology 2006 Jul;68(1):28-32.
- 19. Abdel-Khalek M, Sheir KZ, Mokhtar AA, Eraky I, Kenawy M, Bazeed M. Prediction of success rate after extracorporeal shock-wave lithotripsy of renal stones–a multivariate analysis model. Scand J Urol Nephrol 2004;38(2):161-167.
- 20. Al-Ansari A, As-Sadiq K, Al-Said S, Younis N, Jaleel OA, Shokeir AA. Prognostic factors of success of extracorporeal shock wave lithotripsy (ESWL) in the treatment of renal stones. Int Urol Nephrol 2006;38(1):63-67.
- 21. Choi JW, Song PH, Kim HT. Predictive factors of the outcome of extracorporeal shockwave lithotripsy for ureteral stones. Korean J Urol 2012 Jun;53(6):424-430.
- 22. Tarawneh E, Awad Z, Hani A, Haroun AA, Hadidy A, Mahafza W, et al. Factors affecting urinary calculi treatment by extracorporeal shock wave lithotripsy. Saudi J Kidney Dis Transpl 2010 Jul;21(4):660-665.
- 23. Takahara K, Ibuki N, Inamoto T, Nomi H, Ubai T, Azuma H. Predictors of success for stone fragmentation and stone-free rate after extracorporeal shockwave lithotripsy in the treatment of upper urinary tract stones. Urol J 2012;9(3):549-552.
- 24. Lee HY, Yang YH, Lee YL, Shen JT, Jang MY, Shih PM, et al. Noncontrast computed tomography factors that predict the renal stone outcome after shock wave lithotripsy. Clin Imaging 2015 Sep-Oct;39(5):845-850.
- 25. Ouzaid I, Al-qahtani S, Dominique S, Hupertan V, Fernandez P, Hermieu JF, et al. A 970 Hounsfield units (HU) threshold of kidney stone density on non-contrast computed tomography (NCCT) improves patients’ selection for extracorporeal shockwave lithotripsy (ESWL): evidence from a prospective study. BJU Int 2012 Dec;110(11 Pt B):E438-E442.
- 26. Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, Gallucci M; Working Party on Lithiasis, European Association of Urology. Guidelines on urolithiasis. Eur Urol 2001 Oct;40(4):362-371.
- 27. Patel T, Kozakowski K, Hruby G, Gupta M. Skin to stone distance is an independent predictor of stone-free status following shockwave lithotripsy. J Endourol 2009 Sep;23(9):1383-1385.
- 28. Jeong US, Lee S, Kang J, Han DH, Park KH, Baek M. Factors affecting the outcome of extracorporeal shock wave lithotripsy for unilateral urinary stones in children: a 17-year single-institute experience. Korean J Urol 2013 Jul;54(7):460-466.
- 29. Dretler SP, Polykoff G. Calcium oxalate stone morphology: fine tuning our therapeutic distinctions. J Urol 1996 Mar;155(3):828-833.
- 30. Otnes B. Crystalline composition of urinary stones in recurrent stone formers. Scand J Urol Nephrol 1983;17(2):179-184.
- 31. Argüelles-Salido E, Campoy-Martínez P, Aguilar-García J, Podio-Lora V, Medina-López R. Prediction of the energy required for extracorporeal shock wave lithotripsy of certain stones composition using simple radiology and computerized axial tomography. Actas Urol Esp 2014 Mar;38(2):115-121.
- 32. Geng JH, Tu HP, Shih PM, Shen JT, Jang MY, Wu WJ, et al. Noncontrast computed tomography can predict the outcome of shockwave lithotripsy via accurate stone measurement and abdominal fat distribution determination. Kaohsiung J Med Sci 2015 Jan;31(1):34-41.
- 33. Mostafavi MR, Ernst RD, Saltzman B. Accurate determination of chemical composition of urinary calculi by spiral CT. J Urol 1998;159(3):673-675.
- 34. Al- Marhoon MS. Shareef O, Al – Habsi IS, Al-Balushi AS, Mathew JK, Venkiteswaran KP. Extracorporeal shockwave lithotripsy success rate and complications: initial experience at Sultan Qaboos University Hospital. Oman Med J 2013;28(4):255-259.
- 35. Ammar AF. Shock wave lithotripsy for medium to large renal pelvic stone without ureteral stent. Iraqi Postgrad Med J 2009;8(2):181-183.
- 36. Sahin C, Tuncer M, Yazıcı O, Horuz R, Çetinel AC, Eryıldırım B, et al. Do the residual fragments after shock wave lithotripsy affect the quality of life? Urology 2014 Sep;84(3):549-554.
- 37. Polat F, Yeşil S, Ak E, Farahvash A, Karaoğlan U, Biri H, et al. Safety of ESWL in elderly: evaluation of independent predictors and comorbidity on stone-free rate and complications. Geriatr Gerontol Int 2012 Jul;12(3):413-417.
- 38. Nomikos MS, Sowter SJ, Tolley DA. Outcomes using a fourth-generation lithotripter: a new benchmark for comparison? BJU Int 2007 Dec;100(6):1356-1360.
- 39. Pareek G, Armenakas NA, Panagopoulos G, Bruno JJ, Fracchia JA. Extracorporeal shock wave lithotripsy success based on body mass index and Hounsfield units. Urology 2005 Jan;65(1):33-36.
- 40. Gomha MA, Sheir KZ, Showky S, Abdel-Khalek M, Mokhtar AA, Madbouly K. Can we improve the prediction of stone-free status after extracorporeal shock wave lithotripsy for ureteral stones? A neural network or a statistical model? J Urol 2004 Jul;172(1):175-179.
- 41. Faridi MS. Rahman MdJ, Mibang N, Singh AK, Singh RS, Singh KS. Outcome of extracorporeal shock wave lithotripsy for upper ureteric calculi- experience from North-East Indian City. IOSR Journal of Dental and Medical Sciences. 2016;15(6):108-111.
- 42. Robert M, Marotta J, Rakotomalala E, Muir G, Grasset D. Piezoelectric extracorporeal shock-wave lithotripsy of lower pole nephrolithiasis. Eur Urol 1997;32(3):301-304.
- 43. Naguib M, Eliwa A, Seleem M, Abdulwahab K, Elsayed E, Abdulmaksood M, et al. PD23-06 Outcome of Mini-PCNL versus extracorporeal shock wave lithotripsy in treatment of single lower calyceal stone 10-20 mm with favourable lower calyceal anatomy: a prospective randomized study. J Urol 2016;195(4):507-508.
- 44. El-Nahas AR, El-Assmy AM, Mansour O, Sheir KZ. A prospective multivariate analysis of factors predicting stone disintegration by extracorporeal shock wave lithotripsy: the value of high-resolution noncontrast computed tomography. Eur Urol 2007 Jun;51(6):1688-1693, discussion 1693-1694.
- 45. Musa AA. Use of double-J stents prior to extracorporeal shock wave lithotripsy is not beneficial: results of a prospective randomized study. Int Urol Nephrol 2008;40(1):19-22.
- 46. Argyropoulos AN, Tolley DA. Ureteric stents compromise stone clearance after shockwave lithotripsy for ureteric stones: results of a matched-pair analysis. BJU Int 2009 Jan;103(1):76-80.
- 47. Mohayuddin N, Malik HA, Hussain M, Tipu SA, Shehzad A, Hashmi A, et al. The outcome of extracorporeal shockwave lithotripsy for renal pelvic stone with and without JJ stent–a comparative study. J Pak Med Assoc 2009 Mar;59(3):143-146.
- 48. Salem S, Mehrsai A, Zartab H, Shahdadi N, Pourmand G. Complications and outcomes following extracorporeal shock wave lithotripsy: a prospective study of 3,241 patients. Urol Res 2010 Apr;38(2):135-142.