Hamman first described spontaneous pneumomediastinum (SPM) in 1939.1 It is also known as spontaneous mediastinal emphysema and is characterized by free air in the mediastinum with the absence of known underlying disease. Pathologically, it is explained by the Macklin phenomenon, which is alveolar rupture due to high intra-alveolar pressures, low perialveolar pressures, or both, resulting in air dissection along bronchoalveolar sheaths and to the mediastinum.2
SPM is known to be triggered by emesis, asthma, cough, physical activity, choking, defecation, and drug abuse. Findings on presentation may include chest pain, dyspnea, cough, odynophagia, subcutaneous emphysema, neck swelling, and pneumothorax.3
Pneumorrhachis was first reported in 1977 by Gordon et al,2 and was given the name pneumorrhachis in 1987.3 It is described as air in the spinal canal and can be divided into internal, intradural, or external pneumorrhachis. Air is not normally seen in the spinal canal, and air entry can be from penetrating injuries (trauma, iatrogenic causes) or events leading to increased intrathoracic pressure such as vomiting, coughing, sneezing, or barotrauma-related lung injuries.
Pneumorrhiachis is commonly seen with pneumomediastinum as per literature review as no definite epidemiological correlate is available. As there is no fascia between the posterior mediastinum and the retropharyngeal and epidural space, air can freely diffuse into the epidural space via the posterior surface due to lower resistance. The anterior vascular bundle offers a higher resistance to the free air.
Rarely, there are symptoms associated with pneumorrhachis, and therefore there are no international guidelines for the management of this finding.4 However, one patient with massive pneumomediastinum with associated pneumorrhachis underwent laminectomy due to the neurological symptoms.5
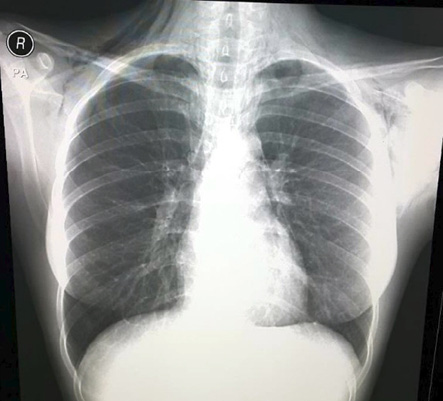
Figure 1: Subcutaneous emphysema in the neck and chest of a 21-year-old female.

Figure 2: Chest computed tomography revealed subcutaneous pneumomediastinum (red arrow).
Case report
A 21-year-old Omani female with no known comorbidities presented to our casualty unit with a two-day history of cough, shortness of breath, and wheezing. She had a history of sore throat two weeks before presentation that was managed conservatively.Clinically, she was not in any respiratory distress. She was afebrile and her oxygen saturation was 97% on room air. She had no clubbing, no central or peripheral cyanosis, no pallor, and no lower limb edema. Pertinent positive findings on chest examination were subcutaneous emphysema in the neck and upper chest with bilateral rhonchi on auscultation. Laboratory investigations were within normal limits.
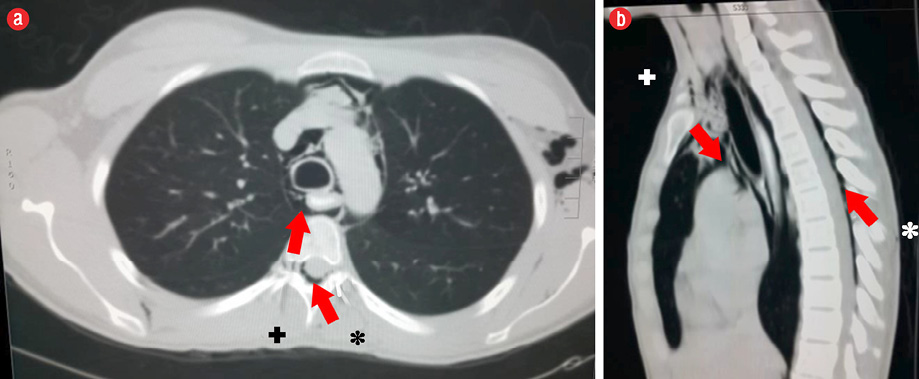
Figure 3: . (a) Axial and (b) saggital plane computed tomography imaging of the chest revealed air (+) the spinal canal extending from the pneumomediastinum (*).
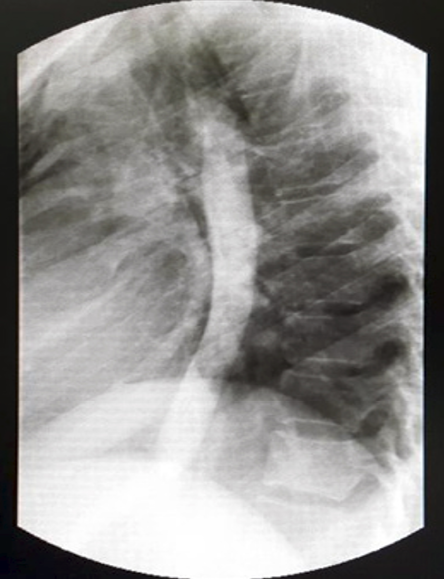
Figure 4: Gastrografin study showing no extravasation of contrast.
Routine posteroanterior chest X-ray revealed pneumomediastinum with subcutaneous emphysema in the neck and chest [Figure 1]. Based on these findings, we admitted the patient for further workup and proceeded to do computed tomography (CT) of the chest, which revealed moderate subcutaneous emphysema in the neck, axilla, and upper chest wall with significant pneumomediastinum extending to the spinal canal [Figure 2 and 3].
Esophagogastroduodenoscopy was normal. Gastrografin study followed by barium swallow showed no obvious extravasation of contrast [Figure 4].
The patient was treated conservatively with oxygen and intravenous prophylactic antibiotics. Her inpatient stay was uneventful, and she was discharged with no complications after three days.
Discussion
Pneumomediastinum was described by Laennec in 1819 while spontaneous mediastinum was described by Hamman in 1939.6 As it is a self-limiting disease and the symptoms are non-specific and vary in severity, the incidence of SPM varies between 1 in 7000 to 1 in 12 000 hospital admissions. The incidence of SPM-related hospital admissions are on the rise, most likely due to increased awareness of this condition. The availability of high-quality imaging can also be attributed to the increased diagnosis.7,8
Spontaneous mediastinum if diagnosed by chest radiograph with the exclusion of any perforation related to intrathoracic viscus, does not require further imaging by CT. However, in the event of symptomatic major aerodigestive air leak diagnostic investigations may be carried out [Figure 5]. The management is bed-rest, oxygen therapy, and analgesia as needed.8 Although much of the literature suggests that the condition is self-limiting, life-threatening complications such as tension pneumomediastinum, single or bilateral pneumothorax or tension pneumothorax, and increased pressure in the pulmonary interstitium leading to dyspnea have been described.9
Pneumorrhachis is air within the spinal canal. It is an abnormal radiological finding with causes ranging from direct trauma to the spine to iatrogenic causes such as epidural anesthesia. With improved imaging techniques, the frequency of diagnosis of pneumorrhachis has increased. Typically, patients are young males with a history of illicit drug inhalation, bronchial asthma, vomiting, coughing, or barotrauma due to elevated pressures from air travel or diving. The imaging modality of choice is CT.10
In 9.5% of cases of pneumomediastinum, pneumorrhachis was observed.11 Pneumorrhachis in patients with SPM is usually with few symptoms directing towards the definitive diagnosis. Like pneumomediastinum, the disease resolves spontaneously in 98% of patients.11
A survey of 48 cases with pneumorrhachis secondary to SPM found that in 98% of cases the condition was self-limiting with no neurological findings.11 One study concluded that pneumorrhachis due to dissection of a SPM has a benign course requiring no treatment.12 A separate study agreed that pneumorrhachis is asymptomatic and the air is absorbed back into the blood directly without any evidence of recurrence, and therefore conservative management is sufficient.10
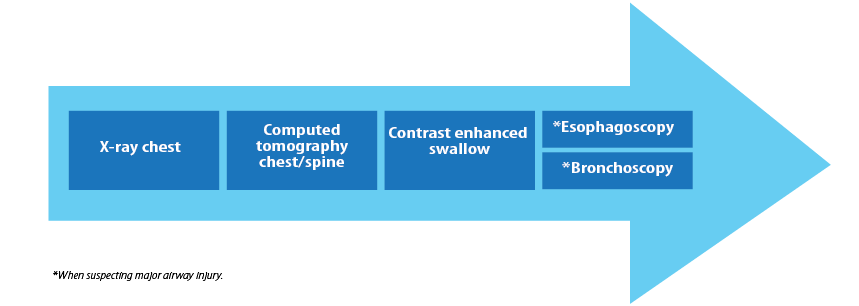
Figure 5: Investigation algorithm: the normal set of investigations done for spontaneous mediastinum.
Conclusion
Our case reiterates the findings of the literature regarding SPM being a diagnosis made after the exclusion of life-threatening conditions of the aerodigestive tract. The availability of improved imaging has led to over-diagnosis and over management of this benign self-limiting condition. However, a high index of suspicion can lead to prompt diagnosis, fewer investigations, and appropriate symptomatic treatment with fewer days in the hospital. Pneumorrhachis is a rare but increasingly common radiological finding seen with SPM, and conservative management is usually sufficient. However, management must be tailored to the patient’s presentation and symptom severity.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp 1939;64:1-21.
- 2. Gordon IJ, Hardman DR. The traumatic pneumomyelogram. A previously undescribed entity. Neuroradiology 1977 Apr;13(2):107-108.
- 3. Newbold RG, Wiener MD, Vogler JB III, Martinez S. Traumatic pneumorrhachis. AJR Am J Roentgenol 1987 Mar;148(3):615-616.
- 4. Aujayeb A, Doe S, Worthy S. Pneumomediastinum and pneumorrhachis: a lot of air about nothing? Breathe 2002 Jun;8(4):331-334 .
- 5. Ripley DP, Wilson EJ, Meller MT, Cowlam S. Pneumorrhachis: a rare complication of diabetic ketoacidosis. Diabet Med 2009 May;26(5):566-567.
- 6. Al Mufarrej F, Bader J, Gharagozloo F, Tempesta B, Strother E, Margolis M. Spontaneous mediastinum: diagnostic and therapeutic interventions. J Cardiothorac Surg 2008 Nov 3;3:59.
- 7. Caceres M, Ali SZ, Braud R, Weiman D, Garrett HE Jr. Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann Thorac Surg 2008 Sep;86(3):962-966.
- 8. Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: a benign curiosity or a significant problem? Chest 2005 Nov;128(5):3298-3302.
- 9. Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944;23:281-358 .
- 10. Oertel MF, Korinth MC, Reinges MH, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J 2006 Oct;15(Suppl 5):636-643.
- 11. Belotti EA, Rizzi M, Rodoni-Cassis P, Ragazzi M, Zanolari-Caledrerari M, Bianchetti MG. Air within the spinal canal in spontaneous pneumomediastinum. Chest 2010 May;137(5):1197-1200.
- 12. Drevelengas A, Kalaitzoglou I, Petridis A. Pneumorrhachis associated with spontaneous pneumomediastinum. Eur J Radiol 1994 May;18(2):122-123.