It is more than 100 years since the first usage of X-ray. In the early days of its implementation, there was no vision about its potential harms,1,2 including various dermatoses, cataract, hematological disorders, and cancer,3 which necessitates considering radiation protection (RP) strategies such as the ‘as low as reasonably achievable’ (ALARA) principle.4 For all medical imaging procedures, there are three basic principles: justification, optimization, and dose limits.5 The optimization concept has been refined as a result of increasing knowledge about radiation effects.6–8 RP has been one of the main concerns since the early days of radiography9,10, and as the technology of medical imaging is continuously under revolution, the regulations needed for its safe usage is an important issue.11 Assessing the knowledge of healthcare personnel working with radiation and holding RP courses might be beneficial in reducing patient and staff exposure to ionizing radiation.12–15 Interventional cardiologists are among the top two professionals most likely to receive high radiation doses in routine examinations.16 The Word Health Organization1 recommends continuous training and regular refresher courses and state that specific training in interventional radiology is required in addition to basic training.17 The International Commission on Radiological Protection (ICRP) states that interventional procedures are complex and tend to be operator dependent. It is particularly important that individuals performing examinations are adequately trained in both RP clinical techniques and knowledge.18
As a good clinical practice needs good knowledge, attitude, and practice (KAP) and as they are practically interdependent, several factors such as sex, education and practice age, and hospital type and geographical region might affect good practice.
This study aimed to assess the KAP level of RP among interventional radiology staff using a validated questionnaire. The findings of this study might help to develop educational policies for radiation workers at different levels of specialty.
Methods
A simple questionnaire survey consisting 30 multiple-choice format (which was previously validated)19 was distributed in 2014–2015 in northern (13.0%), western (10.0%), eastern (2.0%), central (16.0%) regions, and the capital of Iran (59.0%). Ten panelists including four medical physicists, one nuclear medicine specialist, one occupational health specialist, and one epidemiologist were advised and helped to calculate content validity ratio, which the acceptance level was > 0.62. The finalized questionnaire was used in a pilot study including 15 employees in interventional radiology departments using a four-week retest design to check the reliability and validity of the questionnaire. Pearson’s correlation coefficient was estimated, which showed high overall reliability of final version of questionnaire (r = 0.81, p < 0.001).
Table 1: Demographic characteristics of respondents regarding radiation protection knowledge score.
|
Sex |
|
|
0.130 |
|
Male |
48.9 |
22.4 |
|
|
Female |
43.2 |
23.1 |
|
|
Educational age |
|
|
0.860 |
|
≤ 15 |
48.5 |
24.2 |
|
|
> 15 |
49.1 |
17.3 |
|
|
Practice age |
|
|
0.400 |
|
≤ 15 |
47.4 |
24.8 |
|
|
> 15 |
44.5 |
18.8 |
|
|
Hospital type |
|
|
0.160 |
|
Educational |
43.6 |
23.2 |
|
|
Non-educational |
52.4 |
16.9 |
|
|
Private clinic |
49.2 |
23.0 |
|
|
Region |
|
|
0.010 |
|
Capital |
41.7 |
22.0 |
|
|
Center |
45.2 |
24.0 |
|
|
East |
61.5 |
22.4 |
|
|
North |
58.4 |
22.4 |
|
SD: standard deviation
The goals, methodology, and protocols of the project were clarified to the participants who were healthcare personnel working professionally with radiation as department secretaries, radiology technologists, nurses, and physicians in educational (69.0%), non-educational (8.0%), and private health clinics (23.0%). The participants were assured of the obscurity and confidentiality of the collected data. The administered questionnaire had a demographic information section including age, sex, academic degree, job title, educational age (time since graduation) as well as a general RP section about wearing lead aprons during examinations, film badges, dose limits for occupational exposure, the ALARA principle, and participation in RP training courses over recent years. This questionnaire was designed to assess KAP of RP. The collected data were analyzed using SPSS Statistics (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc.) with one-way ANOVA. A p-value < 0.050 was considered statistically significant.
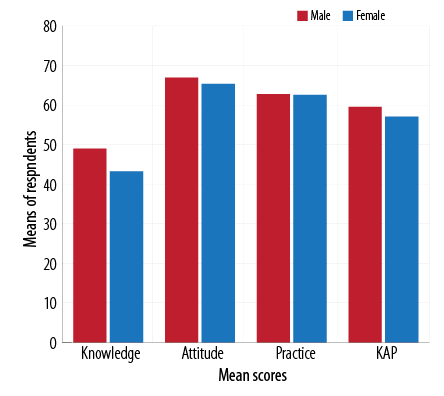
Figure 1: Mean knowledge, attitude, practice (KAP) scores, and overall KAP score regarding radiation protection between sexes.
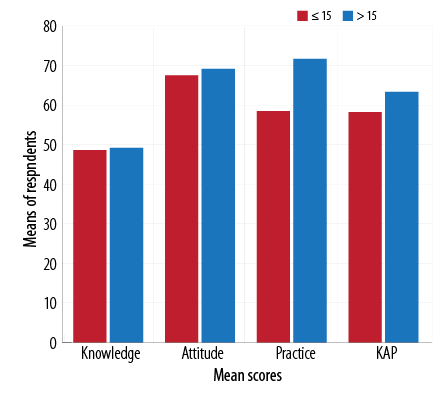
Figure 2: Mean knowledge, attitude, practice (KAP) scores, and overall KAP score regarding radiation protection and educational age (years since graduation).
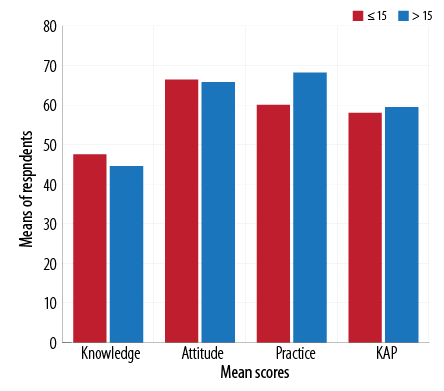
Figure 3: Mean knowledge, attitude, practice (KAP) scores, and overall KAP score regarding radiation protection and practice age.
Table 2: Demographic characteristics of respondents regarding radiation protection attitude score.
|
Sex |
|
|
0.260 |
|
Male |
66.8 |
19.6 |
|
|
Female |
65.3 |
20.5 |
|
|
Educational age |
|
|
0.570 |
|
≤ 15 |
67.4 |
20.4 |
|
|
> 15 |
69.1 |
14.4 |
|
|
Practice age |
|
|
0.830 |
|
≤ 15 |
66.4 |
19.9 |
|
|
> 15 |
65.7 |
18.5 |
|
|
Hospital type |
|
|
0.820 |
|
Educational |
66.6 |
21.2 |
|
|
Non-educational |
65.0 |
13.4 |
|
|
Private clinic |
66.6 |
18.3 |
|
|
Region |
|
|
0.110 |
|
Capital |
63.7 |
21.8 |
|
|
Center |
70.7 |
15.0 |
|
|
East |
79.3 |
9.2 |
|
|
North |
70.4 |
16.9 |
|
SD: standard deviation.
Table 3: Demographic characteristics of respondents regarding radiation protection practice score.
|
Sex |
|
|
0.330 |
|
Male |
62.7 |
17.9 |
|
|
Female |
62.5 |
17.2 |
|
|
Educational age |
|
|
< 0.001 |
|
≤ 15 |
58.4 |
17.8 |
|
|
> 15 |
71.6 |
13.4 |
|
|
Practice age |
|
|
< 0.001 |
|
≤ 15 |
60.0 |
17.9 |
|
|
> 15 |
68.1 |
14.2 |
|
|
Hospital type |
|
|
0.010 |
|
Educational |
60.9 |
17.1 |
|
|
Non-educational |
75.3 |
12.8 |
|
|
Private clinic |
64.0 |
18.3 |
|
|
Region |
|
|
0.070 |
|
Capital |
61.4 |
18.0 |
|
|
Center |
69.1 |
15.7 |
|
|
East |
56.6 |
7.2 |
|
|
North |
66.0 |
19.4 |
|
SD: standard deviation.
Results
Two-hundred and five questionnaires were collected from different geographical regions of Iran. The detailed scores of knowledge, attitude, practice, and overall KAP score regarding sex, educational and practice age, and type of hospital and geographical region of participants are given in Figures 1–5, respectively. The RP knowledge score of participants is presented in Table 1. The analysis of the relationship between sex and RP knowledge showed no significant difference between male and female protection knowledge (p = 0.130), as well as educational age (p = 0.860). There was no significant difference in the mean scores of RP knowledge and practice age (p = 0.400) and likewise, between RP knowledge and hospital type (p = 0.160). A comparison of means revealed a statistically significant difference between RP knowledge and geographical region (p = 0.010). Furthermore, RP knowledge score in northern Iran (mean = 58.4) was significantly higher (p = 0.010) than the capital (mean difference = 16.7).
The mean RP attitude scores are given in Table 2. Statistical analysis showed no significant difference between RP attitude and sex (p = 0.260), educational age (p = 0.570), practice age (p = 0.830), hospital type (p = 0.820), and geographical region (p = 0.110). The detailed scores of the participants RP practice are listed in Table 3. There was no significant difference between RP practice and sex (p = 0.330) and region (p = 0.070). RP practice score in those with > 15 educational age was significantly higher than those with ≤ 15 educational age (p < 0.001). In the group with practice age (years’ experience) > 15, the RP practice score was significantly higher than the group with practice age ≤ 15 (p < 0.001). The RP practice score in non-educational clinics was higher than educational hospitals and private clinics [Table 3].
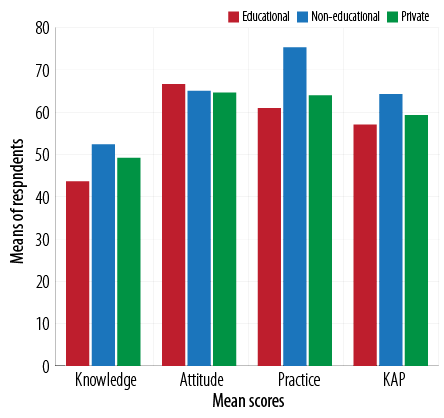
Figure 4: Mean knowledge, attitude, practice (KAP) scores, and overall KAP score regarding radiation protection between hospital types.
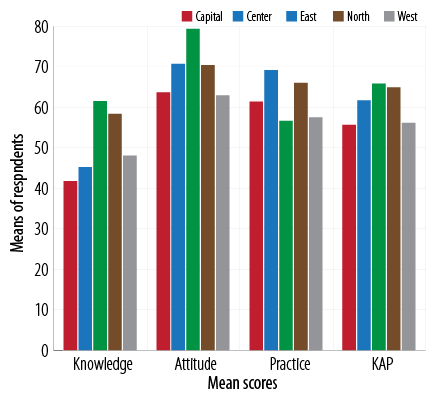
Figure 5: Mean knowledge, attitude, practice (KAP) scores, and overall KAP score regarding radiation protection between geographical regions.
The scores of participant RP KAP are given in Table 4. Statistical analysis showed a difference in mean scores between RP KAP and educational age (p = 0.030), but no significant difference between RP KAP and sex (p = 0.470), practice age (p = 0.530), and hospital type (p = 0.200). The mean score of RP KAP in the eastern region of Iran was significantly higher than the other geographical regions.
Table 4: Demographic characteristics of respondents regarding radiation protection knowledge attitde practice (KAP) score.
|
Sex |
|
|
0.470 |
|
Male |
59.5 |
16.0 |
|
|
Female |
57.0 |
16.3 |
|
|
Educational age |
|
|
0.030 |
|
≤ 15 |
58.1 |
17.4 |
|
|
> 15 |
63.3 |
9.4 |
|
|
Practice age |
|
|
0.530 |
|
≤ 15 |
57.9 |
16.7 |
|
|
> 15 |
59.4 |
13.3 |
|
|
Hospital type |
|
|
0.200 |
|
Educational |
57.0 |
16.8 |
|
|
Non-educational |
64.2 |
7.6 |
|
|
Private clinic |
59.2 |
15.3 |
|
|
Region |
|
|
0.030 |
|
Capital |
55.6 |
17.1 |
|
|
Center |
61.7 |
13.4 |
|
|
East |
65.8 |
9.3 |
|
|
North |
64.9 |
14.0 |
|
SD: standard deviation.
Discussion
Radiology examinations have an essential role in diagnosis. Radiation has been demonstrated to have adverse biological effects, that vary by the duration of exposure and dose,20–22 which has shown an increased occurrence of cancer, shortening of longevity, birth defects, and cataracts.23 The main principles for RP are time, distance, and shielding,24 which should be carefully controlled. During an interventional cardiac catheterization procedure, an interventional cardiologist receives about 0.004–0.016 rem/case25, nurses receive 0.8–1.6 rem/year, and technologists about 0.2 rem/year in an interventional radiology department,26 which is mainly due to patient scatter. Modern cardiac interventional methods produce effective doses of 4–21 mSv and 9–29 mSv, respectively, and are therefore high-risk for radiation exposure,27 which cause RP to be an occupational concern. The continuous trend towards more complex interventional examinations leads to greater exposure to staff and patients. According to the American College of Cardiology, the dose limit for occupational exposure for medical staff is 5 rem/year for the whole body, and no one should receive a cumulative exposure of more than 1 rem × age (or 50 rems).28 Radiology technologists are expected to have more in-depth knowledge on different aspects of radiation and should play a consultant role to the physicians in choosing a proper imaging modality with minimal radiation risk.29 Besides, one should consider the importance of good practice as well as adequate knowledge and attitude to reduce public dose due to imaging modalities. These items depend on several factors such as educational level and current policies for training personnel as well as the available accessories needed for good practice with an acceptable dose to the patient. Considering only one center to evaluate, such a multi-parametric problem might lead to a misunderstanding of several aspects of RP.
We found no significant difference between RP KAP and gender, which is in agreement with a study by Fatahi-Asl et al.30 Arslanoglu et al,12 showed that more female (39%) than male doctors (19%) believed that abdominal magnetic resonance imaging exposes patients to ionizing radiation.
It has previously shown that personnel with a basic science background had better RP awareness levels.31 Staff educational age is one of the factors that influence occupational exposures. Prabhat et al,32 confirmed the relationship between educational age and appropriate KAP level regarding RP. The KAP level was higher in interns and the least in third-year students.32 One study found a significant difference in knowledge between young radiographers (less than three years of experience) and older radiographers, with the former having a higher score. This might be due to the freshness of younger staff.13 However, in our study, no significant difference was observed between RP knowledge and educational age, which might be due to continuous training courses. RP practice score in those with an educational age > 15 years was significantly higher than in those ≤ 15 years. Mojiri et al,33 explained that the radiographers with fewer years’ work experience have less knowledge about the adverse effects of radiation. So, there is an actuarial relationship between awareness about dose limit and radiographers’ educational level.33 A study performed by Svenson et al,34 among Swedish practitioners with 5–25 years experience had higher levels of KAP than those with more or fewer years experience. Su et al,35 confirmed that with increasing age RP knowledge gets significantly worse. Rahman et al,36 demonstrated that the number of correct answers in those with more than 10 years experience in contrast to those with less 10 years experience was 45% vs. 56%, respectively.
We found a relationship between participants practice age and their RP performance. Older staff (practice age > 15) had better radiation safety practice than younger ones (practice age ≤ 15). With increasing age and employment period, radiation safety practice also gets significantly better. The existence of a statistically significant relationship between practice age and RP performance showed that a few radiographers with low experiences have less practical information about radiation safety. Although they were recently educated, they had insufficient knowledge of radiation effects. This means that formal continuous training is necessary for younger radiological technologists.
RP practice in non-educational clinics was significantly (p = 0.010) better than educational hospitals. This might be due to the students in educational hospitals, which might violate the general discipline of the hospital and interfere with experienced staff professional work. The relationship between the geographical region of hospitals and knowledge and RP KAP was statistically significant in our study. Knowledge and RP KAP in northern Iran was significantly better than the capital. This might be due to existing policies in the educational organization in those regions, which enforce personnel to attend these courses and limit their working shifts to have enough time to review basic items and learn new skills.
Conclusion
RP continues to be an important concern in the everyday practice of all medical professionals. Education and practice age, sex, and type of hospital and geographical region have their effects towards KAP of interventional radiology staff regarding RP. Based on our findings, a fundamental effort to provide more robust education and acquire greater RP KAP in interventional radiology departments is required. Many of the radiation-related harms for both interventionalists and patients can be easily prevented by having proper KAP and continuous training.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Szarmach A, Piskunowicz M, Świętoń D, Muc A, Mockałło G, Dzierżanowski J, et al. Radiation safety awareness among medical staff. Pol J Radiol 2015;80:57-61.
- 2. S Leung R. Radiation Protection of the Child from Diagnostic Imaging. Curr Pediatr Rev 2015;11(4):235-242.
- 3. Kraska A, Bilski B. Narazenie pracowników ochrony zdrowia na promieniowanie jonizujace a hipoteza hormezy radiacyjnej. Med Pr 2012;63(3):371-376.
- 4. Geijer H. Radiation dose and image quality in diagnostic radiology. Optimization of the dose-image quality relationship with clinical experience from scoliosis radiography, coronary intervention and a flat-panel digital detector. Acta Radiol Suppl 2002; 43(427):1-43.
- 5. Crane GD, Abbott PV. Radiation shielding in dentistry: an update. Aust Dent J 2016 Sep;61(3):277-281.
- 6. Berkhout WE. [The ALARA-principle. Backgrounds and enforcement in dental practices]. Ned Tijdschr Tandheelkd 2015 May;122(5):263-270.
- 7. Morris ND, Thomas PD, Rafferty KP. Personal radiation monitoring service and assessment of doses received by radiation workers (2004): Australian radiation protection and nuclear safety agency. 2004 [cited 2013 October]. Available from: http://www.arpansa.gov.au.
- 8. Leyton F, Canevaro L, Dourado A, Castello H, Bacelar A, Navarro MT, et al. Radiation risks and the importance of radiological protection in interventional cardiology: A systematic review. Rev Bras de Cardiol Invasiva 2014;22(1):87-98.
- 9. Matsuda M, Suzuki T. Evaluation of lead aprons and their maintenance and management at our hospital. Journal of anesthesia 2016 Jun;30(3):518-21.
- 10. Morgan KZ, Turner JE. Principles of radiation protection. A textbook of health physics. In: Robertson JS, editors. The Quarterly Review of Biology;1968;58(6):1128-1129.
- 11. Holmberg O, Czarwinski R, Mettler F. The importance and unique aspects of radiation protection in medicine. Eur J Radiol 2010 Oct;76(1):6-10.
- 12. Arslanoğlu A, Bilgin S, Kubal Z, Ceyhan MN, İlhan MN, Maral I. Doctors’ and intern doctors’ knowledge about patients’ ionizing radiation exposure doses during common radiological examinations. Diagn Interv Radiol 2007 Jun;13(2):53-55.
- 13. Paolicchi F, Miniati F, Bastiani L, Faggioni L, Ciaramella A, Creonti I, et al. Assessment of radiation protection awareness and knowledge about radiological examination doses among Italian radiographers. Insights Imaging 2016 Apr;7(2):233-242.
- 14. Alavi SS, Dabbagh ST, Abbasi M, Mehrdad R. Medical radiation workers’ knowledge, attitude, and practice to protect themselves against ionizing radiation in Tehran Province, Iran. J Educ Health Promot 2017 Jun;6:58.
- 15. Alavi SS, Taghizadeh Dabbagh S, Abbasi M, Mehrdad R. Radiation protection knowledge, attitude and practice (RP-KAP) as predictors of job stress among radiation workers in Tehran Province, Iran. Iran Red Crescent Med J 2016 Jun;18(10):e29394.
- 16. Rehani MM. Training of interventional cardiologists in radiation protection–the IAEA’s initiatives. Int J Cardiol 2007 Jan;114(2):256-260.
- 17. World Health Organization. Efficacy and radiation safety in interventional radiology. Geneva: World Health Organization; 2000.
- 18. Valentin J. Avoidance of radiation injuries from medical interventional procedures. Ann ICRP 2000;30(2):7-67.
- 19. Moshfegh S, Hasanzadeh H, Jadidi M, Mirmohammadkhani M, Bitarafan-Rajabi A, Abedelahi A, et al. Evaluation of knowledge, attitude and practice of personnel in operating room, ERCP, and ESWL towards radiation hazards and protection. Middle East Journal of Rehabilitation and Health Studies. 2017;4(3):e12354.
- 20. Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A 2003 Nov;100(24):13761-13766.
- 21. Lee CI, Haims AH, Monico EP, Brink JA, Forman HP, Diagnostic CT. Diagnostic CT scans: Assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 2004 May;231(2):393-398.
- 22. Hauptmann M, Mohan AK, Doody MM, Linet MS, Mabuchi K. Mortality from diseases of the circulatory system in radiologic technologists in the United States. Am J Epidemiol 2003 Feb;157(3):239-248.
- 23. Karjodkar F. Textbook of Dental and Maxillofacial Radiology. 2nd ed. New Delhi: Jaypee Brothers; 2011.
- 24. Statkiewicz-Sherer MA, Visconti PJ, Ritenour ER, Haynes K. Radiation protection in medical radiography. 6th ed. St. Louis: Mosby; 2018.
- 25. Zorzetto M, Bernardi G, Morocutti G, Fontanelli A. Radiation exposure to patients and operators during diagnostic catheterization and coronary angioplasty. Cathet Cardiovasc Diagn 1997 Apr;40(4):348-351.
- 26. Renaud L. A 5-y follow-up of the radiation exposure to in-room personnel during cardiac catheterization. Health Phys 1992 Jan;62(1):10-15.
- 27. Bakalyar DM, Castellani MD, Safian RD. Radiation exposure to patients undergoing diagnostic and interventional cardiac catheterization procedures. Cathet Cardiovasc Diagn 1997 Oct;42(2):121-125.
- 28. Limacher MC, Douglas PS, Germano G, Laskey WK, Lindsay BD, McKetty MH, et al; American College of Cardiology. ACC expert consensus document. Radiation safety in the practice of cardiology. J Am Coll Cardiol 1998 Mar;31(4):892-913.
- 29. Ramanathan S, Ryan J. Radiation awareness among radiology residents, technologists, fellows and staff: where do we stand? Insights Imaging 2015 Feb;6(1):133-139.
- 30. Fatahi-Asl J, Tahmasebi M, Karami V. The protection knowledge and performance of Radiographers in some hospitals of Ahvaz County. Jentashapir Journal of Health Research 2013;4(5):405-412.
- 31. Shah AS, Begum N, Nasreen S, Khan A. Assessment of radiation protection awareness levels in medical radiation science technologists-a pilot survey. Journal of Postgraduate Medical Institute (Peshawar-Pakistan) 2007;21(3):169-172.
- 32. Prabhat MPV, Sudhakar S, Kumar BP, Ramaraju. Knowledge, attitude and perception (KAP) of dental undergraduates and interns on radiographic protection-A questionnaire based cross-sectional study. Journal of Advanced Oral Research. 2011;2(3):45-50.
- 33. Mojiri M, Moghimbeigi A. Awareness and attitude of radiographers towards radiation protection. J Paramed Sci 2011;2(4).
- 34. Svenson B, Söderfeldt B, Gröndahl H. Knowledge of oral radiology among Swedish dentists. Dentomaxillofac Radiol 1997 Jul;26(4):219-224.
- 35. Su WC, Huang YF, Chen CC, Chang PS. Radiation safety knowledge of medical center radiological technologists in Taiwan. Radiat Oncol (NYNY) 2000;50(2):1-3.
- 36. Rahman N, Dhakam S, Shafqut A, Qadir S, Tipoo FA. Knowledge and practice of radiation safety among invasive cardiologists. J Pak Med Assoc 2008 Mar;58(3):119-122.