Serum Leptin and Insulin Hormone Level in Recurrent Pregnancy Loss
Rayah S. Baban,1 Noor M. Ali,2 Hala A. Al-Moayed3
doi:10.5001/omj.2010.57
ABSTRACT:
Objective: To measure serum leptin and insulin levels in women with recurrent pregnancy loss using modified methods of High Performance Liquid Chromatography (HPLC), and to examine their influence on recurrent loss at different pregnancy trimesters.
Methods: A case control study was conducted from, 1 September 2008 to 30 December 2009 in the Obstetric and Gynecological Department-Al-Khadimiya Teaching Hospital. HPLC technique with new modified method was used to estimate serum leptin and insulin hormones in samples of women with recurrent pregnancy loss (patients group, n=64) and healthy pregnant women at the end of the third gestational trimester as a control group (n=51).
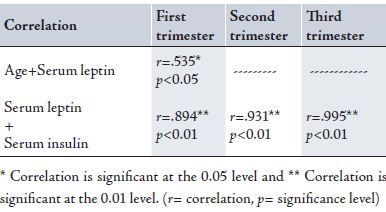
Results: Both serum leptin and insulin levels were high in women with pregnancy loss in their three trimesters. A significant correlation was found between age (r=0.535, p<0.018) and serum total leptin in women with RPL during the first trimester. Also, a highly significant correlation was found between serum total leptin and insulin in women with RPL during the first, second and third trimesters (r=0.894, r=0.931, and r =0.995) respectively. The number of women who lost their pregnancy during the first trimester was higher than those losing during other trimesters.
Conclusion: It can be concluded that recurrent pregnancy loss in women at different trimester is associated with endocrine abnormalities where serum leptin and insulin levels increase in a different way compared with normal healthy pregnant women.
From the 1Department of Chemistry and Biochemistry, College of Medicine, Al-Nahrain University; 2Medical Research Unit, College of Medicine, Al-Nahrain University; 3Department of Gynecology and Obstetrics, College of Medicine, Al-Nahrain University, Baghdad-Al-Khadimiya, P.O.Box 70036.
Received: 11 Apr 2010
Accepted: 03 Jun 2010
Address correspondence and reprint request to: Dr. Rayah S. Baban, Department of Chemistry and Biochemistry, College of Medicine, Al-Nahrain University, Baghdad-Al-Khadimiya, P.O.Box 70036.
E-mail: r_baban@hotmail.com
INTRODUCTION
Recurrent pregnancy loss (RPL) is one of the most frustrating and difficult areas in reproductive medicine because the etiology is often unknown and there are few evidence-based diagnostic and treatment strategies. It differs from infertility and classically refers to the occurrence of three or more consecutive losses of clinically recognized pregnancies prior to the 20th week of gestation.1 The American Society for Reproductive Medicine defines RPL defines it as two or more failed pregnancies (documented by ultrasound or histopathological examination) and suggests some assessment after each loss with a thorough evaluation after three or more losses.2 While some physicians recommend evaluation after the loss of two pregnancies, and others will not begin a workup until the loss of at least three pregnancies.3
Originally, leptin is one of the metabolic hormones that is identified as an adipocyte-derived protein. For years, it was regarded as an exclusive regulator of satiety and energy homeostasis. Its role in pregnancy was later suggested by the findings that plasma levels during gestation are greater than in nongravid individuals and that is synthesized within the fetoplacental unit.4
Leptin is a hormone intimately related to pregnancy, its concentration is much higher during pregnancy than that of non-pregnant women and found to increase progressively during the first two trimesters followed by a slight decline thereafter.5
Dysregulation of leptin metabolism and/or function in the placenta as well as insulin may be implicated in the pathogenesis of various disorders during pregnancy, such as recurrent miscarriage, gestational diabetes, intrauterine growth retardation, and preeclampsia.3 These hormones are secreted into the maternal and to a lesser extent into the fetal bloodstream where they act as placental signals and nourish the fetus, making them possible candidates for the endocrine control of the placenta.6
Li et al. in 2006 proposed that high levels of insulin which is considered as a condition of insulin resistance (IR) is a key factor behind the link between PCOS/obesity and the risk of spontaneous abortion.7 While other previous studies have shown that using metformin may reduce the risk of pregnancy loss in PCOS women.8 While IR is a baseline predictor of clinical efficacy of metformin used for improving fertility performance.9
This study aims to examine the effect of some of the metabolic hormones such as insulin and leptin in women with recurrent pregnancy loss at different trimesters.
METHODS
This is a case control study conducted during the period from 1 September 2008 to 30 December 2009 in the Obstetric and Gynecological Department-Al-Khadimiya Teaching Hospital. 64 women with pregnancy loss at different trimesters were introduced in this study compared with 51 healthy pregnant women with no previous abortion prior to delivery (end of their third trimester).10
Each patient was considered as having recurrent pregnancy loss if they had recurrent miscarriage more than three times. Any patient with hormonal diseases such as progesterone deficiencies (serum progesterone not less than 0.15 ng/ml) which support early pregnancies, hypothyroidism and hyperthyroidism,7 diabetes mellitus during the current pregnancy or before, hypertension, uterine fibroid, were on medication (aspirin ….etc) during current pregnancy or had experienced pregnancy loss because of pathological causes were excluded from the study. 10 ml of venous blood was aspirated from each patient at the time of pregnancy loss and from the control subjects. Ethical approval and patient permission was obtained from the local ethics committee and to conduct the study.
Serum leptin and insulin were measured using High Performance Liquid Chromatography (HPLC), Shimadzu (Kyoto, Japan) which consisted of a system controller model SCL-10 AVP, a degasser model DGU-12A, two liquid delivery pumps model LC-8AVP, UV-Visible detector model SPD-10AVP, and injector model SIL-10A, equipped with 20 µl sample loop. The HPLC system was interfaced with a computer via a Shimadzu class-VP5 chromatography data system program supplied by the manufacturer; Epson LQ-300 printer model P852A (Japan).
All samples and standard solutions were chromatographically analyzed with ODS column using gradient mobile phase 30% acetonitrile, 70% water, flow rate 1ml/min and UV-VIS detection at wavelength 233 nm in order to estimate serum leptin.11
For estimating serum insulin, samples were analyzed using C18 column, gradient mobile phase consisting of a mixture of 74 % of 0.2M Sodium Sulfate adjusted at pH 4.5 and 26% of acetonitrile.12 The flow rate was 1.2 ml/min at wavelength 214 nm. The normal reference ranges for serum leptin and insulin are 7.36±3.73 ng/ml, 2-25 µIU/ml respectively.
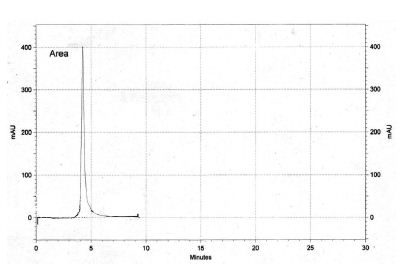
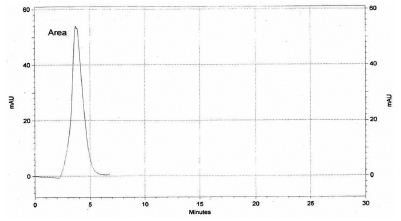
Figs. 1 & 2 represent chromatograms for leptin and insulin hormones in patients sera measured by HPLC. In addition to the negative family history of diabetes mellitus for the patient and control groups, serum glucose level was examined to confirm their inclusion in this study. Estimation of glucose was performed using the enzyme spectrophotometric method (Biomérieux kit) at 510 nm. The normal glucose reference range is 65-110 mg/dl.
Data are presented as means ± SD (standard deviation) using SPSS version 13.0. Regression was used to establish linear equations for insulin and leptin standard curves. Correlation was considered to be significant when p<0.05.
Figure 1: Patient’s serum leptin chromatogram measured by HPLC.
Figure 2: Patient’s serum insulin chromatogram measured by HPLC.
RESULTS
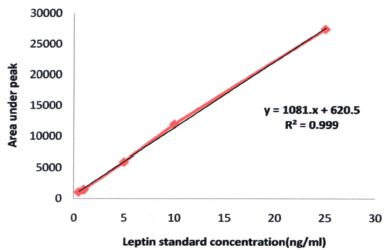
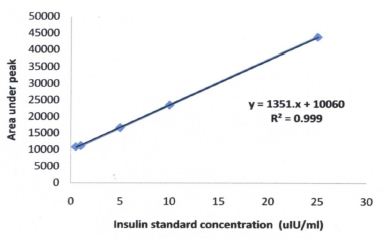
HPLC method with modification was used to evaluate leptin and insulin levels in patients and control group’s sera. As shown in Fig. 3, Leptin standard concentration curve (ng/ml) with its linear equation y=1081.0x+620.5 and R2=0.999 conducted from the area under the peak formed using the range of leptin standard concentration (0-30 ng/ml). While Fig. 4 shows insulin standard concentration curve with the linear equation y=1351.0x+10060 and R2=0.999 when the area under the peak formed with standard concentration range of 0-30 µIU/ml.
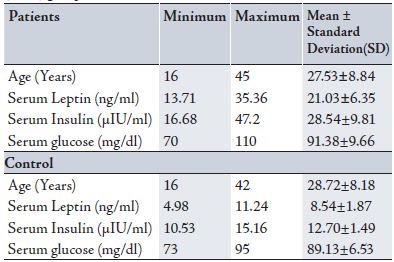
Table 1 demonstrates the mean±SD age of patients (27.53±8.84 years) which was almost comparable with the mean age for the control group (28.72±8.18 years). Patients mean serum leptin and insulin were elevated more than their normal reference ranges (7.36±3.73 ng/ml, 2-25 µIU/ml) mentioned in their kits leaflets respectively (DRG Diagnostics, Germany) and Selected Laboratory Tests according to American Medical Association.13 Also, it was found that the patients’ serum glucose was within normal range because they were selected not to be diabetic, nor hypertensive or have any other diseases. Regarding the control group, serum leptin, insulin and glucose were all within normal limits compared to the patients’ levels.
Table 1: Mean±standard error for patients (n=64) and control (n=51) groups
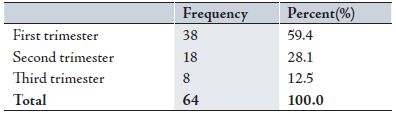
The highest percentage of recurrent pregnancy loss was found among women in their first trimester (59.4%), whereas it was 28.1% for women in the second trimester was. However it was much less in women during their third trimester (12.5%). (Table 2)
Table 2: Patients distribution according to their time of loss
The mean±SE of patients’ serum leptin and insulin were subdivided according to the trimester at the time of pregnancy loss. Both serum leptin and insulin were elevated especially during the first and third trimesters compared to the second trimester. All the patients had normal serum glucose when they were examined at the time of pregnancy loss. (Table 3)
Table 3: Descriptive analysis for patients group in the three trimesters.

A significant correlation was found between age (r=0.535, p<0.018) and serum total leptin in women with RPL during the first trimester. While no correlation was found between age and serum total leptin or insulin in women with RPL during the second or third trimesters. Also, there was a highly significant correlation between serum total leptin and insulin in women with RPL during the first, second and third trimesters (r=0.894, p<0.01; r=0.931, p<0.01; and r=0.995, p<0.001) respectively. (Table 4)
Table 4: Correlations between different variables in patients with recurrent pregnancy loss at there trimesters of pregnancy.
* Correlation is significant at the 0.05 level and ** Correlation is significant at the 0.01 level. (r= correlation, p= significance level)
Figure 3: Leptin standard concentration curve (ng/ml)
Figure 4: Insulin standard concentration curve (µIU/ml)
DISCUSSION
Both cases and controls were taken from Al-Khadimiya teaching hospital, so they were comparable in terms of socioeconomic status. Patients in this study were classified as having unexplained recurrent pregnancy loss (RPL) which was associated with endocrine abnormalities. These abnormalities were obvious in their leptin and insulin levels, with significantly higher levels than the levels found in the control group.
Also in this study, age was considered another factor that might affect recurrent pregnancy loss, (Table 1). This study aimed to identify the effect of age factor on leptin and insulin levels in women with unexplained recurrent pregnancy loss. The mean age of women who experienced pregnancy loss during the second trimester was lower than those who experienced pregnancy loss in the first and third trimesters, (Table 3). The results showed that there was a significant positive correlation between age and serum total leptin levels in women who had experienced pregnancy loss during the first trimester, (Table 4). It should be noted that due to scarcity of studies related to this subject, no comparison could be deduced.
David et al. in 2007 studied serum leptin concentrations and its correlation with gestational age between healthy pregnant and control women.3 They concluded that leptin is a hormone intimately related to the pregnancy, and its concentrations increases during pregnancy. They also found that leptin concentration in pregnant women was much higher than that of age-matched non-pregnant women. Another study by Žaneta et al. found an elevation in maternal serum total leptin levels during pregnancy with alterations particularly during the second and third trimesters of pregnancy. They mentioned that the occurring physiological hyperleptinaemia is not associated with decreased food intake or reduced metabolic activity in pregnant women.
However, it was considered as a state of leptin resistance comparable to the condition in obesity. Therefore, they suggested that this elevation with alteration in leptin level to be an indicator for the cessation of pregnancy naturally either at term or due to pathology at any time during gestation.10 Regarding the metabolic effects of leptin, Reitman et al. in 2001 reported that human pregnancy, like obesity (another condition characterized by high leptin levels), is a leptin-resistant state. Thus, the hyperleptinaemia could be a compensatory response. In addition, they hypothesized another possibility that the placental leptin could have a paracrine role in maintaining pregnancy or in preparation for parturition in normal pregnancy.14
Kim et al. also explained that this manner of leptin elevation could be due to patients’ body weight, as the serum leptin level is dependent on body weight.15
Delia et al. in 2006 reported that circulating maternal total leptin levels are substantially elevated during pregnancy. They explained that this is due to the gradual increase of the body mass index throughout gestation which combines with an increase in estradiol levels that stimulate leptin production from adipocytes.16
While Masayo et al. in 2003 also found that the serum leptin levels during pregnancy were significantly higher than levels in non-pregnant women, and increased from the first to the third trimester. Leptin levels were lower in puerperal women than in pregnant women, and were the same as seen in non-pregnant women.
In addition, they mentioned that BMI did not necessarily reflect body fat mass in pregnant women, and the remarkable increase of the serum leptin level during pregnancy was not explicable by an increase of fat mass alone. They also suggested that the increase of leptin during pregnancy is caused by production in the placenta.17 Hence Sagawa et al. in 2002 concluded in their study that maternal plasma leptin levels are not correlated with body mass index.18 Therefore, the changes in BMI during pregnancy trimesters was not taken into consideration in this study because it depends on feeding status.
Another finding in this study was the increase in serum insulin level in women with RPL during the three trimesters, (Tables 1,3). Serum insulin in these patients was increased in the same way that the total leptin was increased. The elevation in insulin level during pregnancy seems to be affected by the same process that stimulates leptin production from adipocytes. Delia et al. also suggested that this result reflects a condition of insulin resistance, which is in turn associated with leptin resistance.16
It can be hypothesized that in recurrent pregnancy loss with unexplained reason, leptin hormone plays an opposite role of paracrine. It plays an autocrine role resulting in the loss of pregnacy. However, this hypothesizes needs further investigation particularly on placental leptin levels and its receptors in both healthy pregnant women and unexplained recurrent pregnancy loss in women at different trimesters.
CONCLUSION
Overall, recurrent pregnancy loss in women at different trimesters is associated with endocrine abnormalities where serum leptin and insulin levels increase in a different way from the increased levels in normal healthy pregnant women. Since insulin elevation during pregnancy seems to be affected by the same process that stimulates leptin production from adipocytes, both may serve as markers for detecting and monitoring pregnancy complications specially if cases of RPL have no specific medical cause for pregnancy loss, and can be termed as idiopathic or unexplained RPL.
There was no significant correlation between study patients’ age and their leptin levels when pregnancy loss occurred during the second and the third trimesters, while it was found that there was a significant correlation when loss occurred during the first trimester. Because of insufficient number of studies conducted to determine the effect of age on recurrent pregnancy loss at any trimester, there is also a lack of explanation for this finding. However, it can be concluded that in addition to its endocrine mode of action, leptin can also through a paracrine mechanism. Further studies on leptin and its receptors in addition to the other biochemical parameters included in this study in different age groups of women with RPL during the three trimesters are required to strengthen this conclusion.
Generally, since most pregnancy losses occurred during the first trimester, it is highly recommended that leptin and insulin hormone evaluation tests are provided within 12-14 weeks of gestation to prevent pregnancy loss.
ACKNOWLEDGEMENTS
The authors reported no conflict of interest and no funding was received on this work.
-
Recurrent Pregnancy Loss. American Society for Reproductive Medicine. http://www.asrm.org/Literature/mainlit.html. 2010.
-
Practice committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss. Fertil Steril 2008; 89 (6):1603.
-
Grattan D, Ladyman S, Augustine R. Hormonal induction of leptin resistance during pregnancy. Physiology & Behavior.2007; 91 (4): 366-374.
-
De Mouzon Sylvie H, Jacques L; Patrick C. The known and unknown of leptin in pregnancy.2006; 194(6), pp. 1537-1545.
-
Yamada M, Matsuzaki T, Iwasa T, Shimizu F, Tanaka N, Ogata R, et al. Serum Leptin levels in women throughout life; Relationship to body mass index and serum estradiol levels. Japan Society of Reproductive Endocrinology. 2003; 8:55-60.
-
Toth B, Fischl A, Scholz C, Kuhn C, Friese K, Karamouti M, et al. Insulin and leptin receptors as possible new candidates for endocrine control in normal and disturbed human pregnancy. Molecular Human Reproduction 2009; 15(4):231-239.
-
Tian L,Shen H, Lu Q, Robert J, Wang N, Wang J. Insulin Resistance Increases the Risk of Spontaneous Abortion after Assisted Reproduction Technology Treatment.The Journal of Clinical Endocrinology & Metabolism. 2006; 92(4) 1430-1433.
-
Glueck CJ, Wang P, Goldenberg N, Sieve-Smith L. Pregnancy outcomes among women with polycystic ovary syndrome treated with metformin. Hum Reprod.2002; 17 (11):2858–2864
-
Eisenhardt S, Schwarzmann N, Henschel V, Germeyer A, von Wolff M, Hamann A, et al. Early effects of metformin in women with polycystic ovary syndrome: a prospective randomized, double-blind, placebo-controlled trial. J Clin Endocrinol Metab. 2006; 91 (3):946–952.
-
Žaneta K, Gražina D, Zita K. Serum leptin levels in pregnant women and umbilical cord: relationship to mother and neonate anthropometry. ACTA Medica Lituania. 2004; 11(3):26-30.
-
Bushra H. Biochemicaland clinical study of polycystic ovary syndrome and the effect of clomiphene citrate on hormones, leptin and trace elements. MSc. Thesis. College of Science. Al-Nahrain University. 2002. pp. 39.
-
. A simple HPLC method for the simultaneous analysis of insulin and ovomucoid. Pharmazie. 2003; 58(11): 793-795.
-
Iverson CL, Christiansen S, Flanagin AF, Fontanarosa PB, Glass RM, Gregoline B, et al. AMA Manual of Style: A Guide for Authors and Editors. 10th ed. New York, NY: Oxford University Press; 2007. Pp.798.
-
Reitman ML, Bi S, Marcus-Samuels B, Gavrilova O. Leptin and its role in pregnancy and fetal development – an overview. Biochemical Society Transactions 2001; 29, part 2: 68-72.
-
Kim KH, Kim YJ, Lee S, Oh SW, Lee K, Park Y,et al. Evaluation of plasma leptin levels & BMI as predictor of postpartum weight retention. Indian J Med Res. 2008 ;128(5):595-600
-
Alexe D, Syridou G, Petridou E. Determinants of Early Life Leptin Levels and Later Life Degenerative Outcomes. Clinical Medicine & Research. 2006; 4(4): 326 -335.
-
Masayo Y, Toshiya M., Takeshi I. et al. Serum Leptin Levels in Women throughout Life; Relationship to Body Mass Index and Serum Estradiol Levels. Japaneas journal of reproductive endocrinology.2003; 8: 55-60.
-
Sagawa N, Yura S, Itoh H, Mise H, Kakui K, Korita D,et al. Role of leptin in pregnancy--a review.Placenta. 2002; Apr; 23 Suppl A:S80-6.
How to cite this article
Baban RS, Ali NM, Al-Moayed HA. Serum Leptin and Insulin Hormone Level in Recurrent Pregnancy Loss. OMJ 2010 July; 25(3):203-207.
How to cite this URL
Baban RS, Ali NM, Al-Moayed HA. Serum Leptin and Insulin Hormone Level in Recurrent Pregnancy Loss. OMJ [Online] 2010 July; 25(3):203-207. Available at http://www.omjournal.org/OriginalArticles/FullText/201007/FT_SerumLeptinandInsulin.html