Precipitating and Relieving Factors of Migraine Headache in 200 Iraqi Kurdish Patients
Ehsan K. Al-Shimmery
doi:10.5001/omj.2010.59
ABSTRACT
Objectives: To study the precipitating and relieving factors of migraine headache in a group of Iraqi Kurdish patients including the effect of fasting in Ramadan, and to estimate the percentage of family history of migraine.
Methods: A series of 200 migraine cases from different parts of the Kurdistan region in the North of Iraq attending the out-patient Neurology clinic at Rizgary Teaching Hospital and a private Neurology clinic at Erbil City was carried out between October 2007 and May 2008 were reviewed. The precipitating factors and relieving factors for migraine headache were registered and tabulated to be compared with others. Case definition of migraine was based on the International Headache Society (IHS) criteria.
Results: 33% of the patients were aged between 30-39 years, while 40.5% of patients experienced their first attack aged between 20-29 years. Stress or psychological upset was the commonest triggering factor (80%), followed by increasing physical activity (68%), change in weather (65.5%), and in relation to fasting (65%). Fasting in Ramadan was a triggering factor for headaches in 65% of patients. However, there was no significant association between the triggering factors with regards to sex difference. Relief of migraine in the studied sample was achieved using NSAIDs in 50% of patients, and sleep (45.5%). Hence, 61% of the study population had positive family history of migraine, 32.5% of them reported maternal history of migraine.
Conclusion: Psychological upset, stress and excessive physical activity were the commonest triggering factors of migraine headache, while NSAID was the commonest relieving factor of migraine in this population. Family history was present in 61% of migraine patients based mainly from maternal root.
From Neurology Unit, Department of Medicine, Hawler College of Medicine, Erbil, Iraq.
Received: 14 Feb 2010
Accepted: 30 Mar 2010
Address correspondence and reprint request to: Dr. Ehsan K. Al-Shimmery,Neurology Unit, Department of Medicine, Hawler College of Medicine, Erbil, Iraq.
E-mail: eshimmery@yahoo.com
INTRODUCTION
Migraine is an intense and chronically repeated headache that is commonly limited to one side of the head, but can occur as a generalized throbbing headache with extension down to the neck or even the body. Clinically, there are many variant forms but migraine without aura (previously common migraine) is the commonest form. Migraine headaches can affect many people and women are slightly more susceptible than men. It is the second most common cause of headache, affecting approximately 15% of women and 6% of men.1
There are several and varied potential headache precipitating factors (triggers). Triggers are not stereotyped for every migraine patient and not necessarily the same for different attacks in the same person. Sometimes triggers can be as a result of a combination of many factors. For example, a stressful day at work followed by lack of sleep or oversleeping the next morning could trigger a migraine. Other known factors are thought to be alcohol (especially red wine) and dehydration. The major groups of precipitating factors are; dietary (missing meals), stress, environmental (weather changes), hormonal (menses in women), head trauma, smoking, crying, sexual activity, smoke, smell, medications, sleep disturbances, as well as physical and emotional factors.1- 6
Fasting during Ramadan or elective fasting in other days associated with disturbed sleep at night or heavy work throughout the day may induce a migraine attack at the end of the day, which is principally related to hunger, dehydration, and sometimes due to the effect of caffeine withdrawal as drinks containing caffeine are commonly consumed by the studied population.2,6,7,8,9
However, there is no clear proof that certain dietary elements my trigger migraine headache but some patients have reported some dietary elements such as chocolate and cheese to be a cause of headache, but this can sometimes be part of food cravings and not the real cause of headache during the attack.3,4,5
Environmental triggers reported include bright or flickering lights, bright sunlight, glare, overuse of computers, loud sounds, pollution, strong smells, e.g. perfume, gasoline, chemicals, smoke-filled rooms, various food odors, travel-related stress, high altitude, flying, weather changes, and washing hair without subsequent good drying can also trigger intense migraine attacks.1,5,10,11
In a previous study conducted in Iraq which also included 200 migraine patients, the precipitating factors were physical activity and psychological upset in almost 82% of the patients, while specific foods and drinks were the precipitating factors in 19% of the patients, menses in 73% of female patients. While sleep was a relieving factor in 93.5%, and they also found that pregnancy relieved migraine headache in 36 female patients.12
Climacteric factors (final menstrual period) such as menstruation, ovulation, oral contraceptives, hormone replacement therapy (HRT), and menopause can all trigger migraine attacks in women.1
Patients with migraine tended to perform few maneuvers to relieve the headache which include pressing and applying cold stimuli to the painful site, going to sleep, changing posture, sitting or reclining in bed (using more pillows than usual to lay down), isolating themselves, using symptomatic medication, inducing vomiting, changing diet and becoming immobile during the attacks.13
This study discusses some of the triggering factors of migraine headache and their percentage in 200 Iraqi Kurdish patients including physical activity, psychological upset, menses, specific food and or drinks, changes in weather, lights, contraceptive pills and pregnancy, smells such as smoke or odors particularly perfumes and gasoline, and this study also intends to determine the effect of Ramadan fasting on migraines. This study also focuses on the most common medical and nonmedical relieving factors for migraine headache in the studied population, in addition to the estimation of the percentage of family history in Kurdish population.
METHODS
A review of 200 migraine cases triggered from various factors and relieving factor of migraine was performed in this study. Patients who regularly attend the outpatient’s neurology clinic at Rizgary Teaching Hospital and the neurology private clinic visitors in Erbil city, Kurdistan Region, Iraq between October 2007 and May 2008 comprised the study population. The case definition of migraine was based according to the criteria of the HIS.14
The inclusion criteria included patients who fulfilled the above mentioned definition of migraine, aged between 12 to 70 years and are Muslims, in order to also study the effect of fasting.
An interview was carried out by the researcher using a designated questionnaire which included general information about the patient and enquired about specific triggering and relieving factors of migraine, including the effect of fasting in Ramadan and family history of migraine. Patients were included in this study only once free verbal informed consent was given. The research committee at the College of Medicine/ Hawler University approved the study protocol.
Patients were excluded from the study if they had: (a) headaches thought to be related to trauma or injuries; (b) complicated neurological problems, i.e. underlying brain or systemic illness related to their headaches; (c) recent onset of headaches, i.e. less than one month prior to the study.
Patients were stratified by migraine type, age, and duration of illness. The data was entered into a computer using the Microsoft Excel (2003) computer program, and the results expressed by tables showing the percentages of each of the above mentioned factors. The Chi square test of association was used to compare between the males and female proportions. While the Fisher exact test was used (instead of Chi square) when the expected count of the 2X2 table was less than 5. A p value of ≤ 0.05 was considered statistically significant.
RESULTS
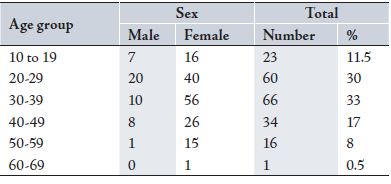
Table 1 shows the demographic distribution of the studied sample at presentation, 33% of the patients were aged between 30-39 years, while 30% were aged between 20-29 years.
Table 1: Age groups and Sex distribution of the studied sample
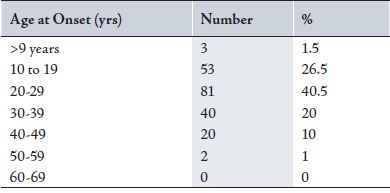
Table 2 shows the age at onset of migraine headache in the studied population. The results show that 40.5% of the patients experienced their first attack aged between 20-29 years, while 26.5% of patients had their first symptoms of migraine during adolescence (10-19 years), and 20% of patients had their migraine aged between 30-39 years.
Table 2: Age at onset of migraine headache
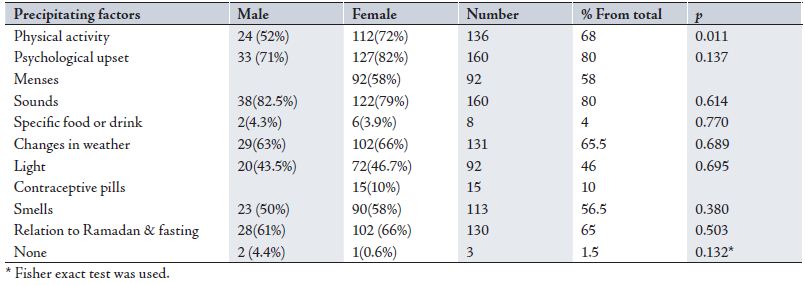
Table 3 shows different triggering factors reported by the 200 migraine patients. Stress or psychological upset were the commonest triggering factors (80%), followed by physical activity (68%), change in whether (65.5%), relation to fasting (65%), smells such as smoke or odors (56.5%), menses in women (50%) in addition women using contraceptive pills also had more migraine attacks (10%), other factors such as lights (40%) which can also be an exaggerating factor for already present headaches. All are important factors that can establish the diagnosis of migraine, and avoidance of such factors is part of migraine management. However, the results found no significant association between any of these triggering factors with regards to sex difference.
Table 3: Precipitating or triggering factors of migraine in the studied sample
* Fisher exact test was used.
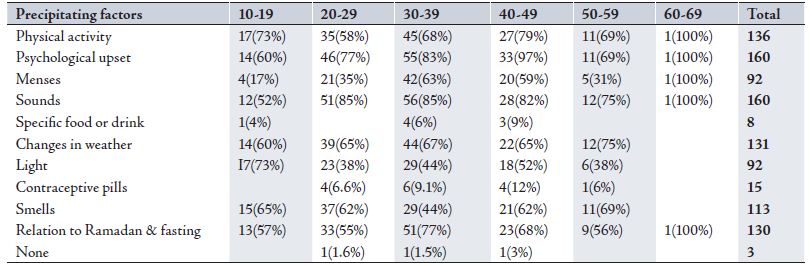
Table 4 shows the percentage of different triggering factors of migraine in relation to age. Increase in physical activity and psychological upset as precipitating factors showed similar results in different age groups, while menses precipitating migraine attacks was more prone in patients between 30-49 years and was reported by older women as a previous trigger before menopause. Sounds, lights, changes in weather, smells such as smoke and perfumes were triggers affecting all age groups. Specific food and drinks were uncommon triggers in the studied population. Hence, fasting during Ramadan and other days of the year was a trigger which was equally presented in all age groups.
Table 4: Precipitating factors in relation to age
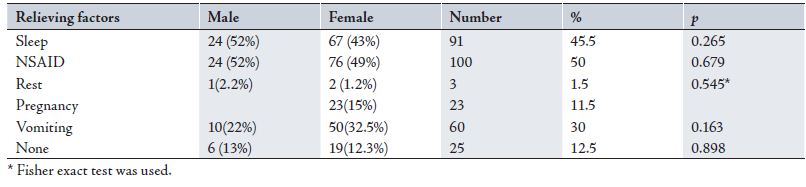
Table 5 shows the frequently medical and non-medical relieving factors of migraine in this study, where NSAIDs were the commonest migraine headache relieving factors (50%) in the studied population, followed by sleep (45.5%), vomiting (30%) and pregnancy in women (11.5%). On the other hand, a few patients (12.5%) reported that the migraine disappeared without any remedy but this is mostly reflective of early migraine headache attacks. There was no significant association between males and females in terms of the relieving factors of migraine headache.
Table 5: Relieving factors of migraine
* Fisher exact test was used.
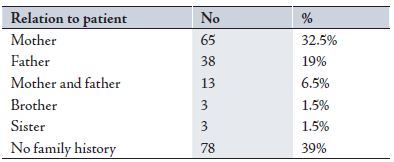
Table 6 shows that 61% of the studied population had positive family history of migraine, while 32.5% of them reported maternal history of migraine, and 19% reported paternal history. While 6.5% of the patients reported of family history of migraines from both mother and father.
Table 6: Family history of migraine
DISCUSSION
This study attempted to register the most common triggering factors of headache attacks in 200 migraine Iraqi Kurdish patients, the results showed that most patients exhibited multiple triggering and relieving factors for their headache attacks, and since all the studied group were Muslims the questioner included the effect of fasting during the holy month of Ramadan and other days of the year.
The patients sample included 200 patients, 77% were females and 23% were males. Initially, this was not an epidemiological study to examine sex prevalence in migraine patients but still migraine usually affects approximately 15% of women and only 6% of men.1
Psychological upset and emotional stress such as depression, anxiety, anger were the commonest triggering factors (80%) in this study, many other studies have reported similar findings.3,6,10,11,12 While physical activity and hard work were reported by 68% of patients as one of the triggering factors of migraine attacks. Similar results have been reported by Khalid et al. in his study in which he described the clinical features of migraine in 200 Iraqi patients (82%).12 However, this finding is contradictory to the findings of Ierusalimschy and Fukui et al. who described that 20% and 13% of their studied samples respectively relates their migraine attacks to physical activity.3,6
Many evidence suggests that there is a relation between migraine and the female sex hormones and these may be indicated by the fact that women with migraine outnumber men by at least a 2:1 ratio and many of patients’ attacks started at menarche and throughout the period of menses.15 Menses and related hormonal disturbances was a triggering factors for migraine attacks in 58% of women in the studied population, most commonly reported by women at aged between 30-49 years, nearly the same has been reported by Fukui and to a less extent by Ierusalimschy.6 However, Khalid et al. reported higher proportion (73%). It may be worth considering that some women are shy to mention such facts during the interview and this is part of the social background, particularly when they are accompanied by their fathers or brothers during the interview.3
Contraceptive pills were reported by 10% of women in the current study as a triggering factor for migraine attacks, this fact is strongly affected by the social background in different populations, since few women are using pills in these societies because of the concept of having large families or using other easier modes of contraception.
Loud sounds were one of the commonly mentioned triggering factors for migraine attacks, especially when the patients walk amongst crowds or at parties, it is also one of aggravating factors for headache intensity and patients usually avoid hearing sounds during the attacks.1 80% of the sample reported that loud sounds triggered their migraine attacks, it was reported in nearly the same proportions in all age groups and in both males and females, however to a lesser extent in the younger group who reported that loud sounds was unlikely to trigger migraine.
Change in weather to extreme cold or worm was also reported by 65.5% of the patients as a trigger of migraine attacks and was presented equally between males and females, but was reported more frequently in the older age group, (Table 4). However, fewer cases have been reported by Ierusalimschy and Robbins, 47% and 43% respectively.3,11 A significant association between changes in weather and migraine has been reported by Zivadinov et al. (OR 1.75, 95% CI 1.27, 2.41) in their studied sample, the reason for the higher percentage in the current study could be attributed to the fact that Iraq is a tropical country having changeable extreme climates.10
Smells such as perfumes, smoke, and different odors were reported as triggering factors for migraine attacks in 56.5% of the studied population, but most commonly in females than males, however the difference was not statistically significant, and similar values were expressed in all age groups, (Tables 3,4). Weather changes, smells, and lights can be differentiating triggering factors for migraine from tension headache type.5 Fukui et al. reported that 34% of his patients’ migraine attacks were triggered by smells.6
Specific foods and drinks were not commonly reported as triggering factors for migraine in the studied sample (4%). However, controlled trials suggest that alcohol (particularly red wine) and caffeine withdrawal are the most important nutritional precipitating factors of migraine.1,2,3 In fact, alcohol and red wine are not commonly consumed by Kurdish population and especially women. The importance of chocolate and cheese has been doubted as triggers for migraine attacks and there is no scientific evidence that they precipitate migraine attacks.2
Migraine attacks have been thought to be increased during the fasting in the holy month of Ramadan by 65% of patients, and there is a lot of evidence to suggest that missing meals, dehydration and caffeine withdrawal would precipitate migraine attacks especially in the first few days of fasting and sometimes throughout the month of Ramadan in severe migraine patients. This renders some patients to stop fasting for the whole month, this fact has been proven by others studies in different populations.1,2,3,6,8,9,11
Sensitivity to light was described by 46% of the patients, most commonly mentioned by very young patients (73%), and distributed nearly equally between the two sexes. Similar results have also been reported in other studies.1,5,11
15% of female patients in the studied sample reported that when they are pregnant they get relief from migraine attacks, in fact the fluctuation of estrogen levels at menarche, menstruation, pregnancy, and menopause may increase or change the prevalence of migraine attacks in women. The sustained high estrogen levels during pregnancy frequently result in headache relief.1,12,16
Sleep and NSAIDs were reported terminate migraine attacks by both males and females in the studied sample (50%). Sleep has been described by many authors as a relieving factor for migraine attacks. However, excess sleep or sleep deprivation are thought to initiate migraine attacks.1,12,13,17
The aspect of family history of migraine in the Kurdish population has not been previously explored. This factor was elaborated in the current studied population. The results showed that 61% of patients had clear family history of migraines; maternal root of inheritance was the commonest (32.5%), while paternal family history was described by 19% of the patients. Ottman et al. reported that family history was not commonly reported in interviews for migraine.18 A sevenfold increase in risk of having migraine in adolescents with positive family history has been reported by Charles et al.19 While Qureshi showed that 70% of pediatric migraine has familial origin.20
CONCLUSION
Overall, migraines in the Kurdish population did not present major differences in terms of the causes and relief modes compared to other populations, however the results showed that migraines were related to excess physical activity and family history, this can be most likely attributed to high consanguineous marriages in this population.
ACKNOWLEDGEMENTS
The author reported no conflict of interest and no funding was received on this work.
-
Raskin NH. Headache. In: Kasper DL, Braunwald E, Fauci A,Hauser S, Longo D, Jameson JL, editors. Harrison’s Principles of Internal Medicine. 17th ed. New York (NY): McGraw-Hill 2008 CD.
-
Holzhammer J, Wöber C. Alimentary trigger factors that provoke migraine and tension-type headache. Schmerz. 2006;20(2):151-9.
-
Ierusalimschy R, Moreira Filho PF. Precipitating factors of migraine attacks in patients with migraine without aura. Arq Neuropsiquiatr. 2002 ;60(3-A):609-13.
-
Yara Dadalti Fragoso; Regina Carvalho; Fernanda Ferrero; Darcya Maria Lourenço; Erica Regina Paulino, Crying as a precipitating factor for migraine and tension-type headache. 2003;121(1):31-33.
-
Spierings EL; Ranke AH; Honkoop PC, Precipitating and aggravating factors of migraine versus tension-type headache. Headache 2001; 41(6): 554-8.
-
Fukui PT, Gonçalves TR, Strabelli CG, Lucchino NM, Matos FC, dos Santos JP, et al. Trigger factors in migraine patients. Arq Neuropsiquiatr. 2008 Sep;66(3A):494-9.
-
Chew NK, Tan CT, Chong HT, Chan YH, Chong KR, Lam H, et al. Ramadan headache; Neurol J Southeast Asia 2001; 6 : 13 – 17
-
Awada A, al Jumah M. The first-of-Ramadan headache. Headache. 1999;39(7):490-3.
-
Abdulbari B., Abdulaziz A., Mohammed B.Do fasting and life style eating habits in Ramadan affect headache? Nutrition & Food Science 2007; 37:6:427 – 433.
-
Zivadinov R, Willheim K, Sepic-Grahovac D, Jurjevic A, Bucuk M, Brnabic-Razmilic O, et al. Migraine and tension-type headache in Croatia: a population-based survey of precipitating factors. Cephalalgia. 2003 Jun; 23(5):336-43.
-
Robbins L; Precipitating Factors in Migraine: A Retrospective Review of 494 Patients. Headache: 2005; 34 (4): 214 – 216.
-
Mussa KI, Sulyman AN, Abdul-Zehra IK. Migraine a clinical study of 200 Iraqi patients. Neurosciences 2003; 8 (1): 71-72
-
Bag B, Karabulut N. Pain-relieving factors in migraine and tension-type headache: International Journal of Clinical Practice 2005; 59(7): 760-763.
-
Olesen J. The international classification of headache disorders. 2nd ed. (ICHD-II). Rev Neurol (Paris) 2005; 161: 689-691.
-
Silberstein SD, Merriam GR. Sex hormones and headache. J Pain Symptom Manage. 1993; 8(2):98-114.
-
Silberstein SD. The role of sex hormones in headache. Neurology.1992; 42 (3 Suppl 2):37-42.
-
Bag B, Karabulut N. Pain-relieving factors in migraine and tension-type headache. Int J Clin Pract. 2005; 59(7):760-3.
-
Ottman R; Hong S, Lipton RB. Validity of family history data on severe headache and migraine. Neurology; 1993; 43(10): 1954-1960.
-
James A. C., B. L. Peterlin, Alan M. R., Steven L. L., Marielle A. K. and Fred D. S. Favorable outcome of early treatment of new onset child and adolescent migraine-implications for disease modification.The Journal of Headache and Pain 2009; 10(4): 227-233.
-
Faiqa Q, Donald L. Managing headache in the pediatric emergency department. Clinical Ped. Emergency 2003; 4 (3):159-170.
How to cite this article
Al-Shimmery EK. Precipitating and Relieving Factors of Migraine Headache in 200 Iraqi Kurdish Patients. OMJ 2010 July; 25(3):212-217.
How to cite this URL
Al-Shimmery EK. Precipitating and Relieving Factors of Migraine Headache in 200 Iraqi Kurdish Patients. OMJ [Online] 2010 July; 25(3):212-217. Available at http://www.omjournal.org/OriginalArticles/FullText/201007/FT_PrecipitatingandRelievingFactors.html.