Diagnostic Value of Electrocardiographic T Wave Inversion in Lead aVL in Diagnosing Coronary Artery Disease in Patients with Chronic Stable Angina
Hatem L. Farhan,1 Kowthar S. Hassan,1 Ali Al-Belushi,1 Mansour Sallam,2 Ibrahim Al-Zakwani,3
Farhan HL, et al. OMJ. 25, 124-127 (2010); doi:10.5001/omj.2010.33
ABSTRACT
Objectives:The clinical value of T wave inversion in lead aVL in diagnosing coronary artery disease (CAD) remains unclear. This study aims to investigate the correlation between aVL T wave inversion and CAD in patients with chronic stable angina.
Methods:Electrocardiograms (ECGs) of 257 consecutive patients undergoing coronary angiography were analyzed. All patients had chronic stable angina. All patients with secondary T wave inversion had been excluded (66 patients). The remaining 191 patients constituted the study population. Detailed ECG interpretation and coronary angiographic findings were conducted by experienced cardiologists.
Results:T wave inversion in aVL was identified in 89 ECGs (46.8%) with definite ischemic Q-ST-T changes in different leads in 97 ECGs (50.8%). Stand alone aVL T wave inversion was found in 27 ECGs (14.1%) while ischemic changes in other leads with normal aVL were identified in 36 ECGs (18.8%). The incidence of CAD was 86.3%. Single, two- and multi-vessel CAD were found in 38.8%, 28.5% and 32.7% of cases respectively. The prevalence of left main, left anterior descending, left circumflex and right coronary arteries were 4.7%, 61.2%, 29.3% and 44.5%, respectively. T wave inversion in aVL was found to be the only ECG variable significantly predicting mid segment left anterior descending artery (LAD) lesions (Odds Ratio 2.93, 95% Confidence Interval 1.59-5.37, p=0.001).
Conclusion: This study provides new information relating to T wave inversion in lead aVL to mid segment LAD lesions. Implication of this simple finding may help in bedside diagnosis of CAD typically mid LAD lesions. However, further studies are needed to corroborate this finding.
From the 1Department of Medicine, Sultan Qaboos University, Al-Khod, Sultanate of Oman, 2Department of Medicine, Cardiology Unit, Sultan Qaboos University, Al-Khod, Sultanate of Oman, 3Department of Pharmacology, Sultan Qaboos University, Al-Khod, Sultanate of Oman
Received: 27 Dec 2009
Accepted: 09 Feb 2010
Address correspondence and reprint request to: Dr. Mansour Sallam, Consultant Cardiologist, Department of Medicine, Sultan Qaboos University, Post Box 35, P C 123 Al-Khod, Sultanate of Oman.
E-mail:mansoursallam@yahoo.com
Farhan HL, et al. OMJ. 25, 124-127 (2010); doi:10.5001/omj.2010.33
INTRODUCTION
The electrocardiogram (ECG) is a simple and non-invasive bedside diagnostic tool with a well-established role in the diagnosis of coronary artery disease (CAD). Many studies have found that the admission of ECG provides important prognostic information in patients admitted with chest pain. For instance, T wave inversion in anterior or inferior location and or ST-segment depression has been associated with high incidence of CAD.1-11 However, little is known about the prognostic significance of the lead aVL as a predictor for CAD in patients with chronic stable angina. In terms of the scope of this study, this issue has not been addressed before.
Accordingly, the objective of this study is to assess the ability of T wave inversion in lead aVL to predict CAD in patients with chronic stable angina admitted for coronary angiography at the Sultan Qaboos University Hospital, Oman.
This was a prospective observational study conducted in patients admitted at the hospital or referred from secondary hospitals with documented CAD as proved by non invasive test (ECG, echocardiography, treadmill exercise, myocardial perfusion imaging or multisided CT scan coronary angiography) requiring invasive coronary angiography. The study population was composed of patients admitted in a 5-month period between December 2008 to April 2009.
All patients referred for coronary angiography with no absolute contraindication
aged > 18 years old were included in this study.12
The exclusion criteria included clinical situations that may result in secondary
aVL lead T wave inversion and or ST segment depression from analysis as Bundle
branch block either left or right, aortic stenosis, left ventricular hypertrophy
and strain and paced ventricular rhythms.13
Out of the 257 patients enrolled in this study, 66 were excluded because they met the exclusion criteria (left bundle branch block 23, right bundle branch block 8, aortic stenosis 18, left ventricular hypertrophy and strain caused by hypertension 16 and paced ventricular rhythm in one patient).
The study population comprised of the remaining 191 patients. Old myocardial infarction either STEMI or NSTEMI was documented in 49 patients (25.7%).
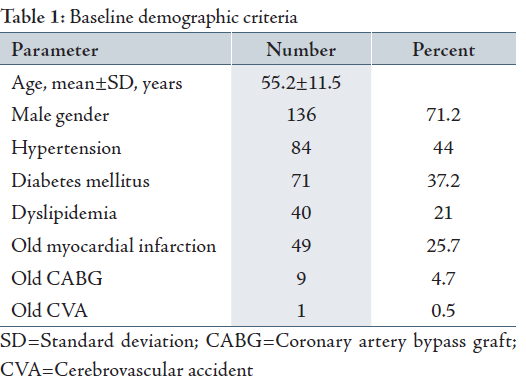
In terms of demographic and clinical data, the baseline characteristics of the patients with respect to gender, mean age, and risk factors for CAD are depicted in Table 1. Patients enrolled in this study were predominantly males (71.2%), with a mean age of 55.2±11.5 years with multiple risk factors for coronary artery disease. The incidence of hypertension was very high (84 patients, 44%) as well as diabetes mellitus (71 patients, 37.2%) reflecting high risk patients for CAD.
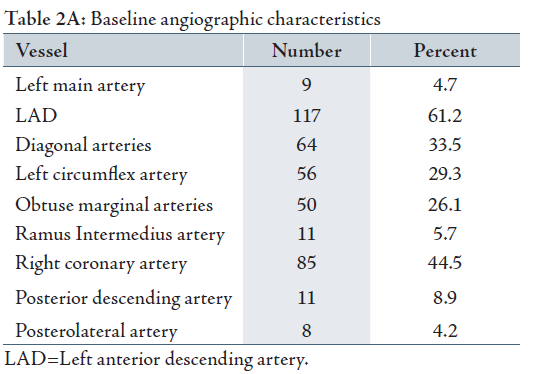
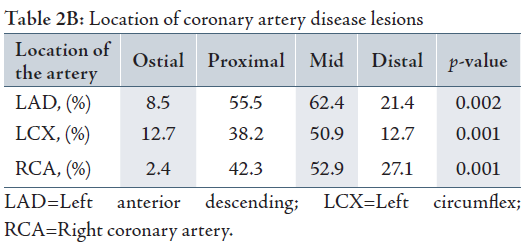
Angiographic characteristics are detailed in Tables 2A and 2B. The incidence of CAD in the studied population was 86.3%, other coronary angiograms proved evidence of normal coronaries except 3 angiograms that demonstrated slow flow (1.57%) and another one (0.5%) with myocardial bridge. Single, two and multivessel CAD was found in 38.8%, 28.5% and 32.7% respectively. The prevalence of left main, left anterior descending, left circumflex and right coronary arteries were 4.7%, 61.2%, 29.3% and 44.5% respectively. Table 2B detailed lesion location in all main vessels.
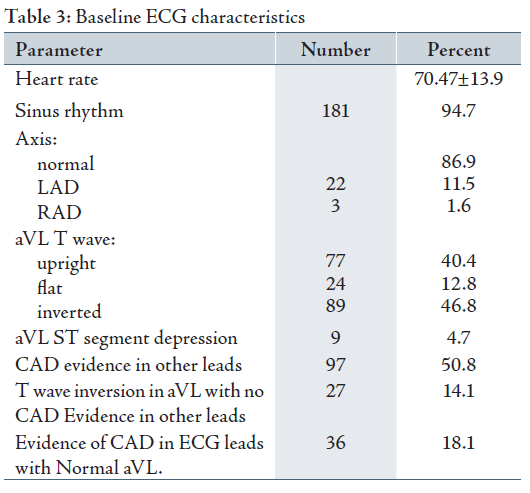
The baseline ECG characteristics according to ST changes suggestive of CAD are listed in Table 3. There were 89 patients (46.8%) who had T wave inversion in aVL and only 9 patients (4.7%) had ST depression in aVL. Overall, ECG changes suggestive of CAD were noticed in 97 patients (50.8%) with stand alone T wave inversion in lead aVL found in 27 ECGs (14.1%) while ischemic changes in other leads with normal aVL were identified in 36 ECGs (18.8%).
The ECG has been established in medical literature as an applicable and reproducible non‑invasive diagnostic tool for assessing myocardial ischemia. 14 In the setting of acute coronary syndrome, several ECG findings help to localize the occlusion site of the LAD coronary artery with respect to its major branches as ST segment elevation in lead aVR was found to be very useful in identifying LAD occlusion proximal to first septal perforator. 15,16
Until now, it is to the authors’ understanding that the value of lead aVL in diagnosing CAD in patients with chronic stable angina has not yet been addressed in literature. Wellens syndrome refers to “LAD coronary T-wave syndrome”, the criteria of which includes history of anginal chest pain, normal or minimally elevated cardiac enzyme levels, and finally, ECG changes without Q waves with deep inversion of the T-wave in the precordial leads.17,18,19 In contrast to Wellens syndrome, this study addressed patients with chronic stable angina and relevance of lead aVL in diagnosis of CAD. Given into account the increasing frequency of CAD and limited health resources, it is crucial to identify patients with increased risk for cardiac events for further intervention.
In evaluating the prognostic value of lead aVL T wave inversion in patients with chronic stable angina; after excluding secondary etiologies that may alter the T wave polarity such bundle branch block, left ventricular out flow tract obstruction, hypertension with strain pattern and paced ventricular rhythms, the results from this study showed that T wave inversion in lead aVL significantly predicts LAD lesion typically mid segment.
On ECG ischemic changes, pathological Qs and or ST-T changes suggestive of CAD were identified in 50.8% of all ECGs. The baseline coronary angiographic data proved evidence of obstructive CAD in 86.7% of patients. In the presence of obstructive CAD, there was higher prevalence of left anterior descending artery lesions (61.2%) especially in mid segments (62.4%). Lead aVL T wave inversion was the only abnormal finding that predicted mid LAD lesions (odds ratio 2.931955, 95% confidence interval 1.59-5.37, p=0.001). Despite the fact that there was a trend to predict proximal LAD lesions, it did not however reach statistical significance (p=0.066).
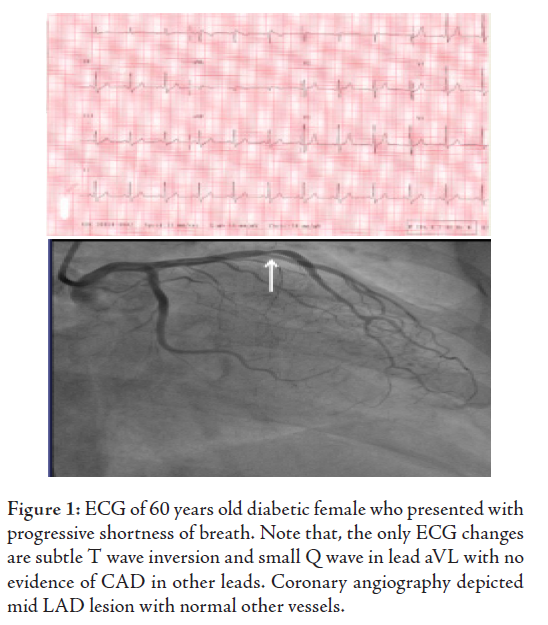
In terms of the prevalence of T wave inversion in lead aVL, interestingly, T wave inversion in lead aVL found in 46.8%, flat and upright T wave seen in 12.8% and 40.4% respectively. Neither flat nor upright T wave in such lead predicted CAD. More interestingly, stand alone T wave inversion in lead aVL was found in 27 ECGs (14.1%) with no pathological Qs and or ST-T changes in other leads, all these ECGs have been described as normal ECG by the referring physicians. (Fig. 1)
Other ECG ischemic changes in lead aVL: In this series, significant (more than 1 mm) ST segment depression in lead aVL denoting CAD was found in 4.7% of the study population with no statistical correlation with the diagnosis of CAD. The mechanism by which why only T wave inversion in lead aVL predicts CAD, namely mid LAD lesions as opposed to ST segment depression and or pathological Qs or even flat T wave in the same lead is beyond the scope of this study.
This study confirmed the prognostic value of T wave inversion in lead aVL with coronary artery disease typically mid left anterior descending artery lesions in patients with chronic stable angina in absence of secondary ST-T changes. Such undemanding findings add important information to the medical field especially to general practitioners during routine check up or cardiac risk assessment before non cardiac surgery.
The authors reported no conflict of interest and no funding has been received on this work.
-
Engelen DJ, Gorgels AP, Cheriex EC, De Muinck ED, Ophuis AJ, Dassen WR, et al. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute myocardial infarction. J Am Coll Cardiol. 1999;34:389-395.
-
Cannon CP, McCabe CH, Stone PH et al. The electrocardiogram predicts one-year outcome of patients with unstable angina and non-Q wave myocardial infarction: results of the TIMI III Registry ECG Ancillary Study. J Am Coll Cardiol. 1997; 30:133-40.
-
Nyman I, Areskog M, Swahn E et al. Very early risk stratification by electrocardiogram at rest in men with suspected unstable coronary heart disease. J Int Med. 1993; 234:293-01.
-
Okada M, Yotsukura M, Shimada T, et al. Clinical implications of isolated T wave inversion in adults: electrocardiographic differentiation of the underlying causes of this phenomenon. J Am Coll Cardiol. 1994; 24:739-745.
-
de Zwaan C, Bar FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982; 103:730-736.
-
Rhinehardt J, Brady WJ, Perron AD, et al. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. 2002; 20:638-643.
-
Chatterjee K, Harris A, Davies G, et al. Electrocardiographic changes subsequent to artificial ventricular depolarization. Br Heart J. 1969; 31:770-779.
-
Predictive Value of the Electrocardiogram in Acute Coronary Syndromes N.A.Mark Estes III and Deeb N. Salem JAMA. 1999; 281(8):753-754.
-
Gorgels AP, Vos MA, Mulleneers R, de Zwaan C, Bar FW, Wellens HJ. Value of electrocardiogram in diagnosing the number of severely narrowed coronaries in rest angina pectoris. Am J Cardiol. 1993; 72:999-1003.
-
The ECG in acute coronary syndromes: new tricks from an old dog Gurm and Topol. Heart. 2005; 91:851-853.
-
Tamura A, Kataoka H, Mikuriya Y, Nasu M. Inferior ST segment depression as a useful marker for identifying proximal left anterior descending artery occlusion during acute anterior myocardial infarction. Eur Heart J. 1995; 16: 1795-1799.
-
ACC/AHA Guidelines for Coronary Angiography: Executive Summary and Recommendations. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) Developed in collaboration with the Society for Cardiac Angiography and Interventions. Patrick J, David P, Anne-Marie A, Gregory J. etal. Circulation. 1999; 99:2345-2357.
-
Kligfield P, Gettes L, Bailey JJ, et al: Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part I: The Electrocardiogram and its Technology: A Scientific Statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2007; 115:1306.
-
Diderholm E, Andrén B, Frostfeldt G, et al. ST depression at entry indicates severe coronary lesions and large benefits of an early invasive treatment strategy in unstable coronary artery disease: the FRISC II ECG substudy. Eur Heart J. 2002; 23:41-49
-
Tamura A, Kataoka H, Mikuriya Y, Nasu M. Inferior ST segment depression as a useful marker for identifying proximal left anterior descending artery occlusion during acute anterior myocardial infarction. Eur Heart J. 1995; 16: 1795-1799.
-
Quyyumi AA, Crake T, Rubens MB, Levy RD, Rickards AF, Fox KM. Importance of “reciprocal” electrocardiographic changes during occlusion of left anterior descending coronary artery. Studies during percutaneous transluminal coronary angioplasty. Lancet. 1986; 1:347-350.
-
de Zwaan C, Bar FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. Apr 1982; 103(4 Pt 2):730-736.
-
Nisbet BC, Zlupko G. Repeat Wellens’ Syndrome: Case Report of Critical Proximal Left Anterior Descending Artery Restenosis. J Emerg Med. Apr 2 2008.
-
Movahed MR. Wellens’ syndrome or inverted U-waves? Clin Cardiol. Mar 2008; 31(3):133-134.