Changing Patterns of Blood Borne Sepsis in Special Care Baby Unit, Khoula Hospital
Bhaskar Gupta, Eisa El Amin
Gupta B, et al. OMJ. 25, 100-103 (2010); doi:10.5001/omj.2010.28
ABSTRACT
Objectives: Infection is a frequent and important cause of morbidity and mortality in neonatal units all over the world. Over the years, there has been a shift in the microorganisms responsible for neonatal septicemia. This study aims to analyze the changing patterns of blood borne organisms in the neonatal unit.
Methods:This retrospective study was undertaken at the neonatal intensive care unit of Khoula Hospital in Muscat, Sultanate of Oman to analyze the incidence of blood borne sepsis and its changing pattern from 1997-2000.
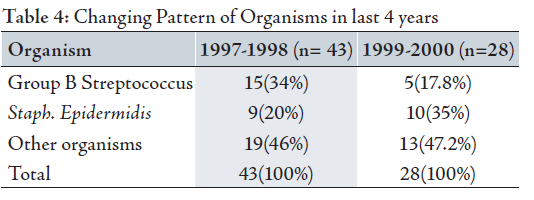
Results: Out of a total 2181 admissions to the neonatal intensive care unit, 71 (3.25%) babies had positive blood culture. A reduction in the incidence of blood borne sepsis with changing patterns of organisms was seen over the period of four years with incidence of Group B Streptococcus declining from 34% in 1997-1998 to 17.8% in 1999-2000 and the incidence of CONS (Staphylococcus epidermidis) increasing from 20% in 1997-1998 to 35% in 1999-2000.
Conclusion: Overall, due to survival and prolonged hospitalization of extremely low birth weight babies who need frequent invasive procedures, and the use of powerful antibiotics, the incidence of Staphylococcus epidermidis which was previously thought to be non pathogenic has increased over the years in neonatal intensive care units.
From the Department of Pediatrics, Special Care Baby Unit, Khoula Hospital, Muscat Sultanate of Oman.
Received: 01 Feb 2010
Accepted: 20 Mar 2010
Address correspondence and reprint request to: Dr. Bhaskar Gupta, Department of Pediatrics, Special Care Baby Unit, Khoula Hospital, P.O. Box 90 Code 116, Muscat Sultanate of Oman.
E-mail: brg30363@omantel.net.om
Gupta B, et al. OMJ. 25, 100-103 (2010); doi:10.5001/omj.2010.28
INTRODUCTION
Infections are a frequent and important cause of morbidity and mortality in neonatal units. As many as 2% of fetuses are infected in utero and up to 10% of infants are infected in the first month of life.1 The incidence of sepsis in neonatal period is 1-10 per 1000 live births with a mortality rate as high as 15-20%.2 Premature babies present with early and fulminant disease.
The common organisms responsible are Group B Streptococcus , Gram negative enteric organisms particularly E.Coli , other organsims such as Staphylococcus Streptococcus > Listeria Monocytogens Hemophilus influenza, gram negative rods such as Klebsiella, Pseudomonas, Serratia and Proteus 1 In Western literature, gram positive organisms were more than twice as common as gram negative until 1943, but between the years 1958 to 1965, gram negative organisms were responsible for more than 75% of cases. In the recent years, Gram positive organisms have gained importance in neonatal intensive care units. This is due to the frequent invasive procedures and to the fact that previously thought nonpathogenic organism like Staphylococcus epidermidis are now considered pathogenic.3 Also, the use of powerful antibiotics against known organism have paved the way for others previously unknown or unimportant organisms
The incidence of group B Streptococcus has increased over the recent times. Invasive GBS sepsis occurs due to the transmission from the mother to infant during delivery and is seen in the first week of life.4 With increasing complexity of neonatal intensive care, prolonged ventilation, use of total parentral nutrition and other modalities of modern neonatology, gestationally younger and lower birthweight newborns are surviving and remaining for a longer time in an environment of high risk of infection.5
Newborns are less capable of responding to infections due to immunological deficiencies involving the reticuloendothelial system, complement, cytokines, antibody and cell mediated immunity. Also, co-existing diseases such as hyaline membrane disease, acidosis also contribute to infections.
In the neonatal intensive care unit of Khoula hospital, extreme preterm babies are being treated and with the modalities of ventilation, surfactant and Total parentral nutrition. Babies of birth weight 750 gram’s and above are supported with good survival. Due to their prolonged hospitalization, changing patterns of infections are being increasingly recognized.
This study was done to analyze the changing patterns of blood borne organisms in the unit over the period of 4 years.
This is a retrospective analysis conducted on all the babies admitted in the Special care baby unit from January 1997 to December 2000. In all babies with suspected clinical sepsis, blood culture was collected in Oxoid Signal Blood Culture BC0102M bottles. This was incubated in the laboratory at 37 degrees Celsius and then plated at 24 hours, subcultured at 48 hours and on the 7th day for growth of organisms. The data regarding the growth of organisms in blood culture was collected and analyzed. The total number of babies admitted to the unit with positive blood cultures was compared over the four year period. Also, the types of organisms and the mortality directly due to fulminant septicemia was analyzed.
RESULTSThe analysis performed for the pattern of bloodborne sepsis in the Special care baby unit at Khoula Hospital from the year 1997 to 2000 revealed changing patterns of organisms.
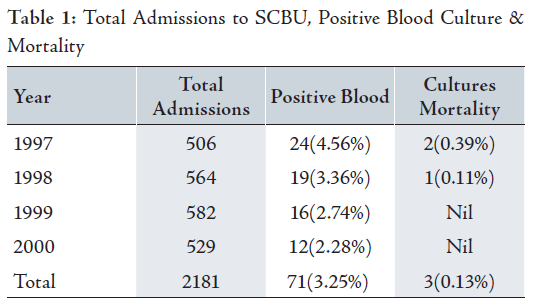
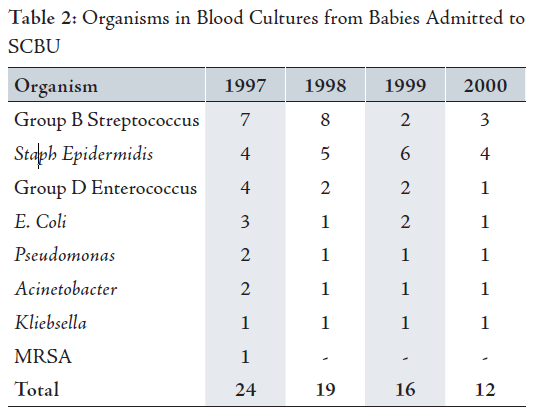
Out of the total 2181 admissions over the 4 year period, 71 (3.25%) babies had positive blood cultures. The mortality rate due to fulminant bactermia was observed in 3 (0.13%) of all admissions and this was in the year 1997 and 1998. No baby died due to fulminant bactermia during 1999-2000, (Table 1). The various organisms detected included Group B Streptococcus Staphylococcus epidermidis , Group D Enterococcus E.Coli, Pseudomonas Acinetobacter, Klebsiella and MRSA. (Table 2)
The findings suggested changing patterns of organisms in the unit over the period of 4 years. With increased awareness and administration of prophylactic antibiotics in all mothers with Group B Streptococccus, the incidence of GBS sepsis in newborns has also declined over the last 4 years.
A total of 15 (34%) babies had positive blood culture for GBS in 1997-1998 as compared to only 5 (17.8%) babies during the year 1999-2000.
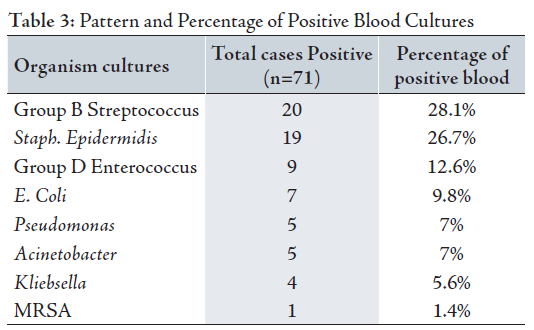
There was an increasing incidence of CONS (Staphyloccous epidermidis) which constituted 9 (20%) cases in 1997-1998 as compared to 10 (35%) cases in 1999-2000. This is mainly attributed to the policy since the year 1999 of ventilation and care of extreme preterm babies of less than 1 kg in weight. These babies need prolonged hospitalization and more invasive procedures and are thus more prone to nosocomial infections mainly CONS sepsis. (Table 3)
Other organisms constituted 19 (46%) in 1997-1998 and 13 (47.2%) in 1999-2000, suggesting an insignificant difference in their pattern over the last four years. (Table 4)
Due the implementation of strict handwashing and infection control programs implemented in SCBU only 1 (1.4%) case of MRSA was observed during this period.
Special care baby unit babies are at high risk for bloodstream infections because of their prematurity, prolonged hospitalization and frequent invasive procedures. The incidence of blood stream infection in various units varies between 4-32%. 3.25% of positive blood cultures were noted in the unit.6
The two most common bacterial pathogens in term infants in first 28 days of life were Group B Streptococcus and E.Coli which constitute 70% of systemic neonatal bacterial disease.7 These may be acquired from the mother during the intrapartum period or nosocomial acquisition. The analysis of positive blood cultures which included both preterm and term babies admitted to the unit showed that Group B Streptococcus and E.Coli accounted for 27 (38%) of cases.
Throughout the years, there has been a shift in the microorganism responsible for neonatal septicemia. This has been shown in the findings from Yale-New Haven Hospital in a study by Freedman et al.8 During 1930’s, Group A Streptococci were the predominant organisms. In the 1950’s Staphylococci became a major cause of nursery outbreaks throughout the world. Pseudomonas was also becoming more prominent during that decade due to the introduction of respiratory support systems. From the late 1950, until present E.Coli and Group B Streptococcus have been important causes of neonatal sepsis. Also, Group D Streptococci and Klebsiella have been recently observed in nurseries and account for a high proportion of antibiotic resistant organisms that colonise and infect babies in neonatal intensive care units.9
Since 1980, Coagulase negative Staphylococci collectively known as S. Epidermis have assumed considerable importance as troublesome nosocomial pathogens in the neonatal intensive care units.10 This organism is seen more commonly in premature infants who require prolonged hospitalization, total parentral nutrition, Central vascular catheters and thoracostomy tubes. Infants infected with coagulase negative Staphylococci have subtle signs of septicemia and do not develop metastatic focal infection. Treatment of these infections is also complicated by high frequency of penicillin and gentamicin resistant strains, yet most strains remain sensitive to Vancomycin. In most cases, removal of central venous catheter in conjunction with the administration of high doses of penicillin and aminoglycoside is sufficient to sterilize the bloodstream. Vancomycin should be reserved for resistant cases. In analysis performed by Gray et al. in 1995, they reported Coagulase negative Staphyloccous in 62% of first positive blood cultures obtained after 48 hours of NICU stay.11 The results from this study also demonstrated the increasing incidence of Coagulase negative Staphylococcus from 9 (20%) cases in 1997-1998 as compared to 10 (35%) cases in 1999-2000. This was mainly due to the policy of care of extreme preterm babies up to a birth weight of 750 gms who needed prolonged hospitalization and this policy was implemented from the year 1999.
The analysis conducted at the unit in khoula Hospital showed the changing pattern of organisms over the years. With GBS accounting for 34% of positive blood cultures between 1997-1998, the incidence fell to 17.8% between 1999-2000. This could be attributed to better obstetric and neonatal co-ordination, early screening and treatment of GBS positive mothers and prophylactic antibiotics in babies of mother with suspected choroamnionitis and premature rupture of membranes. David et al. in an Australian study for neonatal infections analyzed the intrapartum use of antibiotics and early onset of neonatal sepsis caused by Group B Streptococcus and found a steady fall in early onset Group B Streptococcus infections in Australia from 2 per 1000 in 1991 to 1.3 per 1000 in 1997.12 The findings from the Australian study suggest that it may be possible to reduce the incidence of Early onset Group B Streptococcus infection below 0.6 per 1000 with the use of intrapartum antibiotics alone and that this has the added advantage of reducing early onset infections caused by other organisms.13
Group D Enterococcus constituted 9 (12.6%) cases and the incidence was seen to be declining over the years between 1997-2000. However, the incidence of group D Enterococcus appears to have increased in many centers.14 Hence the clinical pattern of the disease is remarkably similar to that seen with group B Streptococci by Alexander et al. who reported that with prompt and appropriate antibiotic therapy, the prognosis appears to be good.15 Mortality was not encountered with Group D Enterococcus infections.15
Other organisms such as Psuedomonas (7%), Acinetobacter (7%) and Klebisella (5.6%) did not constitute much of the proportion of blood culture positive cases.
MRSA has been a major contributor to the nursery infections since 1980’s and MRSA outbreaks have been reported with increasing frequency in neonatal intensive care units.16 The standard control measures includes contact isolation, hand washing with chlorhexidine and detection of carriers. The population at risk for colonization or infection are infants under 1500 gms with long standing catheters, Central nervous shunts, thoracostomy tubes and those needing prolonged hospitalization.17 Only 1 (1.4%) case of MRSA blood culture was recorded. This was mainly due to strict handwashing techniques, barrier nursing and infection control policy in the unit.
CONCLUSIONThe incidence of neonatal sepsis has increased among very low birth weight and premature babies needing prolonged hospitalization.
The analysis over four a year period between 1997-2000 in the Special care baby unit showed that there was a changing pattern of organisms. During the first two years, the predominant organisms were Group B Streptococcus seen in 34% of cases, whereas over the next two years their incidence decreased to 17.8%, which is mainly attributed to increased awareness of GBS carrier mothers and use of prophylactic intrapartum antibiotics and rapid screening and treatment of babies. There was an increase in the incidence of Coagulase negative Staphylococcus over the last 4 years with 20% of cases in first two years as compared to 35 % over the next two years. This was mainly due to care of extreme preterm infants needing prolonged hospitalization and invasive procedures. There was no significant difference in the pattern of other organisms seen over the last four years. Proper implementation of infection control policies in the unit such as strict handwashing, restricting visitors, sterilization of equipments, proper waste disposal, barrier nursing and staff education on infection control methods had a definite impact on the reduction in the overall incidence of blood borne sepsis.
The authors reported no conflict of interest and no funding has been received on this work.
-
Gotoff SP. Infections of the Neonatal infant, Nelson textbook of Pediatrics, W.B Saunders Company, Philadelphia, 16th Edition 1999; 1:538-552.
-
Haque KH. Infection and immunity in the newborn, Forfar & Arenil’s Textbook of Pediatrics, Churchill Livingstone, London 4th Edition 1996; 302-310.
-
Davies PA, Gothefors L. Bacterial infections in the fetus and newborn infant. W.B Saunders, Philadelhphia 1984; 1-10.
-
American academy of Pediatrics, committee on infectious diseases and committee on fetus and newborn: Guidelines for prevention of GBS infections by chemoprophylaxis: Pediatrics 1992; 90:775-778.
-
Guerina NG. Bacterial and Fungal Infections, Manual of Neonatal care, John P Cloherty and Ann R Stark, 4th Edition 1998; 271-299.
-
Cole FS, Taeusch HW. Bacterial infections of the newborn. Schaffer & Avery’s disease of newborn . WB Saunders Philadelphia,6th Edition 1991; 35-369.
-
Schaffer A, McCracekn, Howard J, Mc Intosh K. Bacterial infections in the newborn, Schaffers textbook of Neonatology. p 350- 369.
-
Freedman RM, Ingram DC, Gross I, Ehrenkranz RA, Warshaw JB, Baltimore RS. A half century of neonatal sepsis at Yale. Am J Dis child 1981; 135:140.
-
Goldmann D, A Durbin, W A Jr, Freeman J : Nosocomial infections in a neonatal intensive care unit. J Infect Disease, 1981; 144: 449.
-
Fleer A, Verhoef J, Henandez A. Coagulase negative staphylococci as nosocomial pathogens in neonates, the role of host defense, artificial devices and bacterial hydrophobia. Am J Med 1986;161-165.
-
Gray JE, Richardson DK, Mc Cormick MC, Goldman DA. Coagulase negative staphyloccal bacteremia among very low birth weight infants : relation to admission illness severity, resource use, and outcome. Pediatarics 1995; 95:225-230.
-
Issacs D, Royle JA. Australiasian study group for Neonatal infections : Intrapartum antibiotics and early onset neonatal sepsis caused by Group B streptococcus and by other organisms in Australia: Ped Infec Dis J. 1999; 18:524-528.
-
Issacs D, Prevention of early onset Group B streptococcal infections : Screen, treat or observe? Arch Dis Child, Fetal and Neonatal edition 1998; 181-182.
-
Siegel JD, Macracken GH Jr. Group D Streptococcal infections. J Pediatric 1978; 93:542.
-
Alexander JB, Giacoia GP. Early onset neon enterococcal Group D Streptococcal infections in newborn infant. J. Pediat 1978; 489-491.
-
Battisti O, Mitchson R, Davies PA. Changing blood cultures isolates in a referral Neonatal intensive care unit. Arch Dis Child 1981; 775-778.
-
Storch GA, Rajgopalan L. Methicillin resistant staphylococcus aureus bacteremia in child. Pediat. Infect Dis 1986; 59-61.