Kaposi Sarcoma in Calabar, Southern Nigeria
Maurice Asuquo,1 Aniefon Umana,1 Otei Otei,1 Imabasi Bassey,2 Godwin Ebughe2
ABSTRACT
Objectives: There has been an increase in the prevalence of Kaposi sarcoma (KS) with the emergence of Human Immunodeficiency Virus (HIV).
Methods: Patients with histologic diagnosis of KS seen in the University of Calabar Teaching Hospital, Calabar between January 2007 and December 2008 were studied. Diagnosis of HIV was based on enzyme linked immunosorbent assay (ELISA).
Results: In total, 15 patients (10 males, 5 females, M: F=2:1) presented with KS and accounted for 33.0% of total skin malignancy and ranked second after squamous cell carcinoma, 42.0%. Their ages ranged from 5 and 60 years (mean 37.5 years). Twelve patients (M=8, F=4), 80%, were HIV seropositive, while 3 (M=2, F=1) were HIV seronegative. The lower limb was the commonest affected site, 57.9%.
Conclusion: The most common clinical type was HIV related KS. Ignorance, sociocultural beliefs, poverty, late presentation were underlying issues.
From the 1Department of Surgery, University of Calabar Teaching Hospital, Calabar, Nigeria 2Department of Pathology, University of Calabar Teaching Hospital, Calabar, Nigeria.
Received: 15 Jan 2009
Accepted: 25 Jan 2009
Address correspondence and reprint request to: Dr Maurice Asuquo, Department of of Surgery, University of Calabar Teaching Hospital, Calabar, Nigeria.
E-mail: mauefas@yahoo.com
.INTRODUCTION
A Hungarian dermatologist Moritz Kaposi first described Kaposi sarcoma in 1872. There are 4 clinical variants of the disease: classic, African (endemic), immunosuppression (transplant) associated and Acquired Immuno Deficiency Syndrome (AIDS)-associated KS with identical histologic features.1 This tumour was endemic in Africa even before the advent of HIV.2 Since the emergence of HIV infection, there has been a steady increase in the prevalence of KS world wide.3,4 This study sought to identify the current clinical pattern, challenges of management of KS in our region.
Methods
All the patients with clinical evidence of KS had histopathological evaluation of biopsy specimen to confirm the diagnosis. The period of study was between January 2007 and December 2008. This was compared with total skin malignancy seen during the same period as part of our prospective study of malignant skin tumours. Serology test for HIV antibodies were performed using the Enzyme Linked Immuno Sorbent Assay (ELISA). CD4 cell count was by the dyna bead method and patients with counts <200 cells/dl were offered anti retroviral therapy in addition to chemotherapy (Dactinomycin/vincristine), while those with counts >200 cells/dl had chemotherapy. Viral load studies were not available. Vascular markers study by immunohistochemistry for confirmation of CD31, CD34 and factor VIII were not available in our centre. An in situ hybridization study for herpes simplex virus type 8 in biopsy specimen was also not available. Evaluation of response was clinical and categorized into no regression, partial regression and complete regression.
RESULTS
In total, 15 patients (10 males, 5 females) with a male to female ratio of 2:1 presented with KS. This accounted for 33.0% of skin malignancies seen in the same period and ranked second following squamous cell carcinoma (SCC), 42.0%), others were melanoma 13%, basal cell carcinoma 5%, metastatic carcinoma 5% and dermatofibrosarcoma protuberans 2%. They ranged in age from 5 and 60 years (mean 37.5 years). Twelve patients (M=8, F=4), 80%, were HIV positive, their ages ranged from 5 and 60 years (mean 35.6 years) and 3 (M=2, F=1), 20% were HIV negative, and their ages ranged from 19 and 58 years (mean 45 years), Table 1.
Table 1: Age/ Gender/ Serology distribution
Age Range |
Gender |
Total (%) |
|||
|
M |
F |
|
||
|
Sero +ve |
-ve |
Sero +ve |
-ve |
|
1 – 10 |
1 |
|
|
|
1( 6.7) |
11 – 20 |
|
1 |
|
|
1( 6.7) |
21 – 30 |
|
|
2 |
|
2 (13.3) |
31 – 40 |
4 |
|
1 |
|
5 (33.3) |
41 – 50 |
3 |
|
|
|
3 (20.0) |
51 – 60 |
|
1 |
1 |
1 |
3 (20.0) |
Total |
8 |
2 |
4 |
1 |
15 (100) |
They were all heterosexuals. Most had topical herbal treatment for periods that ranged from 3 months, and 2 years (mean 9 months). Some patients presented in grotesque picture with fungating lesions (figures 1 and 2).

Figure 1: Kaposisarcoma (seronegetive)

Figure 2: Kaposisarcoma (HIV seropositive)
These lesions were dressed with honcrivine (honey and acriflavine) and antibiotics administered based on sensitivity. The common isolates were pseudomonas, proteus, and E coli.
Table 2 shows the site distribution of the lesions. The lower
limb, Figure 1 ranked first 11 (57.9%), 9 seropositive, 2 seronegative. The upper limb was involved in 2 patients (seropositive-1, Figure 2 and seronegative-1). Two groin lesions found were lymphadenopathy in seropositive patients; Figure 3 shows section of lymphoid tissue with proliferating vascular channels with slit like appearance.
Table 2: Site Distribution of KS
Region |
Sero positive |
Sero negative |
Total(%) |
Head/ Neck |
2 |
|
2 (10.5) |
Upper Limb |
1 |
1 |
2 (10.5) |
Trunk |
1 |
|
1 (5.3) |
External genitalia |
1 |
|
1 (5.3) |
Groin |
2 |
|
2 (10.5) |
Lower Limb |
9 |
2 |
11 (57.9) |
|
|
|
100 |
Three patients were HIV seronegative; one received a ray amputation for a localised toe lesion with destruction of the bone. The site healed and there was no evidence of new lesion within the 6 months of follow up. Two patients received cytotoxic chemotherapy (Dactinomycin, vincristine) with partial regression of nodules. They were lost to follow up after 3-5 months
(Table 3a)
Table 3a: Treatment/ Outcome
Sero negative (n=3)
No. of Patients |
Surgery |
Cytotoxic chemotherapy |
Outcome/ (follow up) |
1 |
Ray amputation (toe lesion with bony destruction) |
- |
Healed (6 months) no new lesion
|
2 |
|
Dactinomycin and Vincristine |
Partial regression of nodules. Lost to follow up (3 months) |
|
|
Vincristine/ Dactinomycin |
Partial regression of nodules (5 months) |
The results were generally poor for the HIV seropositive patients, 6 patients were lost to follow up after diagnosis. Two patients received cytotoxic chemotherapy (Dactinomycin/vincristine) and antiretroviral drugs with no regression of nodules, 3 who received cytotoxic chemotherapy had partial regression of nodules. All the patients were lost to follow up after 4-5 months of follow up. Patients were lost for fear of stigmatization, sociocultural reasons, and inability to afford drugs. There was one hospital mortality. (Table 3b)
Table 3b: Sero positive (n=12)
No. of Patients |
Surgery |
Cytotoxic chemotherapy |
ARV therapy |
Outcome/ (follow up) |
6 |
_ |
_ |
_ |
Lost to follow up |
3 |
_ |
Vincristine/ Dactinomycin |
_ |
Partial regression of nodules (4-5 months)
|
2 |
_ |
Vincristine/ Dactinomycin |
Yes |
No regression of nodules (4 months)
|
1 |
_ |
_ |
– |
Fatal |
DISCUSSION
Kaposi sarcoma is a common malignancy in our region. It ranked second in frequency, 33.0% after SCC 42.0%. In the United states, skin cancer is the most frequent diagnosed cancer; of these, approximately 80% are basal cell carcinoma and 20% are SCC, the second most common skin cancer.5 In Africa, several studies reveal the preponderance of SCC and in Tanzania, KS is the second most common dermatologic malignancy.6,7 There are regional differences in the prevalence of KS with lower figures recorded in the northern Nigeria. In Kano, northern Nigeria, KS was the 4th most prevalent malignant skin tumour (8%)8 and Maiduguri, northeastern Nigeria 16%.9 The annual hospital incidence in the present study was 7.4 cases per year when compared to our previous of 5.5 cases per year.2 Pitche et al in Togo10 reported an annual incidence of 8.5 cases per year, Kagu et al in Maiduguri, northeastern Nigeria 10 cases per year.11 However, Mbah et al in Sokoto,12 Northwestern Nigeria reported an average hospital incidence of 2.5 cases per year.
Eighty percent of the patients were HIV seropositive and 20% seronegative. This is at variance with an earlier publication in this centre that suggested that KS was not related to HIV infection.13 This current clinical pattern is in keeping with reports from Nigeria and other countries inflicted with HIV epidemic: Mohhamed et al in Kano, northern Nigeria (HIV positive 59.3%, negative
40.7%),14 Mbah et al in Sokoto, northeastern Nigeria (HIV positive 59.3%, negative 40.75),12 and Pitche et al in Lome, Togo (HIV positive 78.5%, negative 21.5%).10 All our patients were heterosexuals; however, HIV was acquired through mainly homosexual contact in Sao Paulo, Brazil where HIV positive patients were 25.2%. 15
The male: female ratio in this report was 2:1. Onunu et al in Benin, south western Nigeria reported M: F ratio of 1.6:1.16 This is contrary to previous Nigerian studies that reported the occurrence of KS exclusively in men.13 Wabinger et al reported in endemic KS a M : F ratio of 15:117. The prevalence of HIV related KS is increasing in Nigeria with the increase in the number of women being diagnosed with this form of KS, probably owing to more females having HIV disease.16, 18
The HIV patients were younger (mean 35.6 years) when compared to the HIV negative (45 years). Kagu et al northeastern Nigeria 11 reported a median age of 37 years and Pitche et al in Togo10 33.8 years. HIV related KS has been known to affect younger patients than the endemic type. In Nigeria, there is a downward shift in mean age from earlier account due to the changing pattern of KS with HIV positive being more frequent than negative.14
The predominant site affected was the lower limb with some presenting in grotesque picture of fungating lesions (Figure 1).
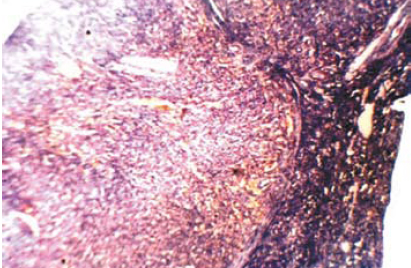
Figure 3: H&Ex40 Kaposi Sarcoma sections shows lymphoid
tissue with proliferating vascular channels with slit like appearance
Ignorance, sociocultural factors, and poverty were notable factors as all the patients had prior topical herbal treatment before presentation and this accounted for the late presentation.
Other reports attest to the lower limb as the commonest affected site.2, 3,12
Some patients were lost to follow up after the diagnosis of HIV infection for fear of stigmatisation. Others were lost due to poverty, as they could not afford to pay for drugs. Endemic KS responds to chemotherapy while AIDS related KS might not and has a poor prognosis.19, 20 This underscores the need for prevention. The facility for measuring the viral load and differences in viral genome is not available in our centre; this could have explained the differences in response to chemotherapy in the HIV subset. Radiation therapy provides excellent results with few side effects in all types of KS.21 None of our patients had radiotherapy, as this facility is not available in our centre. Those referred were unwilling because of cost.
CONCLUSION
In conclusion, HIV related KS is the most common clinical type in our region. Ignorance, sociocultural beliefs, poverty were underlying issues.
ACKNOWLEDGMENTS
The authors report no conflict of interest and no funding has been received in this work.
1. Antman K, Chang Y. Kaposi’s sarcoma. N Engl J Med 2000; 342:1027-1038.
2. Asuquo ME, Ogunkeyede A, Bassey EE, Ebughe G. Kaposi sarcoma: Changing trend in Calabar, southeastern Nigeria. Ann Afr Med 2008; 7:98-101.
3. Mandong BM, Chirdan LB, Anyebe AO, Mannaseh AN. Histopathological review of Kaposi’s sarcoma in Jos: A 16-year review. Ann Afr Med 2004; 3: 174-176.
4. Oyango JF, Njiru A. Kaposi’s sarcoma in a Nairobi Hospital. East Afr Med J 2004; 81:120-123.
5. Gross MD, Monroe M. Skin cancer. Squamous cell carcinoma eMedicine Dermatology [Journal serial online] 2006. Available at http://www.eMedicine.com/ent/topic 26.htm
6. Yakubu A, Mabogunje A. Skin cancer in Zaria, Nigeria. Trop Doct 1995; 25 (suppl.):63-67.
7. Amir H, Kwesiagbor G, Hirgi K. Comparative study of superficial cancer in Tanzania. East Afr Med J 1992; 69:88-93.
8. Ochicha O, Edino ST, Mohammed AZ, Umar AB. Dermatological malignancies in Kano, Northern Nigeria. A histopathological review. Ann Afr. Med 2004; 3:188-191.
9. Nggada HA, Na’aya HU, Ali N. A histopathological analysis of malignant tumours of the skin in University of Maiduguri Teaching Hospital, Nigeria. Highland Med Res J 2003; 1:38-40.
10.Pitche PT, Kombate K, Owono F, Tchangai-Walla K. Kaposi’s sarcoma in a hospital setting in Lome (Togo): A study of 93 cases. Int J Dermatol 2007; 46s1:42-44.
11.Kagu MB, Nggada HA, Garandawa HI, Askira BH, Dorusinmi MA. AIDS- associated Kaposi’s sarcoma in Northeastern Nigeria. Singapore Med J 2006; 47: 1069-1074.
12.Mbah N, Abdulkareem IH, Panti A. AIDS-Associated Kaposi’s sarcoma in Sokoto, Nigeria. Niger J Clin Pract 2008; 11:181-184.
13.Otu AA. Kaposi’s sarcoma, clinical immunological and therapeutic considerations. Niger Med Pract 1990; 19:87-92.
14.Mohammed AZ, Nwana EJC, Mannaseh AN. Changing patterns of Kaposi’s sarcoma in Nigeria. Trop Doct 2005; 35:168-169.
15.Yoshioka MC, Alchorne MM, Porro AM, Tomimon-Yamashita J. Epidemiology of Kaposi’s sarcoma in patients with acquired immunodeficiency syndrome in Sao Paulo, Brazil. Int J Dermatol 2004; 43: 643-647.
16.Onyango JF, Njiru A. Kaposi sarcoma in a Nairobi Hospital. East Afr Med J 2004; 81:120-123.
17. Wabinger HR, Parkin DM, Wabwire-Mangen F. Cancer in Kampala, Uganda in 1989-1991: Change in incidence in the era of AIDS. Int J Cancer 1993; 54:26-36.
18.Onunu AN, Okoduwa C, Eze EU, Adeyekun AA, Kubeyinje EP, Schwarz RA. Kaposi’s sarcoma in Nigeria. Int J Dermatol 2007; 46:264-267.
19.Asuquo ME, Okereke-Okpa I, Achor G. African Kaposi sarcoma-Florid lesion in a Nigerian male in South Eastern equatorial rain forest: A case report. Niger Med Pract 2006; 50:72-76.
20.Stein ME, Lacher J, Spencer D, Bezmoda Wr. Chemotherapy for AIDS- related and endemic African Kaposi’s sarcomain Southern Africa. Int J Dermatol, 1995; 34:729-732.
21.Stein ME, Lacher J, Spencer D, Margolus L, Bezwoda WR. Variants of Kaposi’s sarcoma in South Africa. A retrospective analysis (1980-1992). Acta Oncol 1996; 35:193-199.