Severe Intraoperative Hypercapnia Complicating an Unsual Malfunction of the Inner Tube of a Co-axial (BAIN'S) Circuit
Youssef Emam Youssef, Godwill Iyasere
Youssef EY, et al. OMJ. 25, (2010); doi:10.5001/omj.2010.46
ABSTRACT
The Bain's co-axial circuit system is fully established in general anaesthesia practice. It is favoured for its light weight and suitability for head and neck surgery. However, there are numerous published reports of malfunction of the inner tube of the Bain's co-axial circuit, with potentially lethal complications for the patient. This report presents a case in which a patient connected to a reused Bain's circuit (Datex-Ohmeda) developed severe hypercapnia in the early intraoperative period due to unusual defect of the inner tube. This report tests and outlines the integrity of co-axial circuits and also reviews the available literature.
From the Department of Anesthesia and ICU, Sultan Qaboos Hospital, Sultanate of Oman.
Received: 09th Jan 2010
Accepted: 02 Mar 2010
Address of Corresponding author: Dr. Godwill Iyasere, Senior Consultant, Department of Anesthesia and ICU, Sultan Qaboos Hospital, Salalah, Sultanate of Oman.
E-mail: osarobo46@yahoo.com
Youssef EY, et al. OMJ. 25, (2010); doi:10.5001/omj.2010.46
INTRODUCTION
The Bain's co-axial circuit system is fully established in general anaesthesia practice.1 It is favoured for its light weight and suitability for head and neck surgery. However there are numerous published reports of malfunction of the inner tube of the Bain's coaxial circuit, with potentially lethal complications for the patient.
We present a case in which a patient connected to a reused Bain's circuit (Datex-Ohmeda) developed severe hypercapnia in the early intraoperative period because of an unusual defect on the inner tube. The tests of integrity of co-axial circuits are outlined and the literature is reviewed.
A 31 year old female patient, weighing 70 kg, ASA 2, was scheduled for total thyroidectomy. Preoperative assessment revealed acceptable pulmonary function, complete blood count and renal function. There was no significant tracheal compression or deviation. Haemodynamic parameters, body temperature and thyroid function test were within normal limits.
The patient received premedication comprising of pethidine 75mg and phenergan 25mg intramuscularly 1 hour preoperatively. Induction of anaesthesia was accomplished with intravenous fentanyl 100 mcg, thiopentone sodium 300 mg and succinylcholine 100 mg; the trachea was intubated with a 7mm reinforced tube and connected to an Ohmeda anaesthesia machine via a Datex- Ohmeda specification of Bain's co-axial circuit. Anaesthesia was maintained with infusions of propofol (2-4mg kg -1), atracurium besylate (0.4mg kg -1) and 60% Nitrous Oxide in Oxygen. Vital signs monitored included blood pressure, pulse oximetry, electrocardiogram and end tidal carbon dioxide (ETCO2).
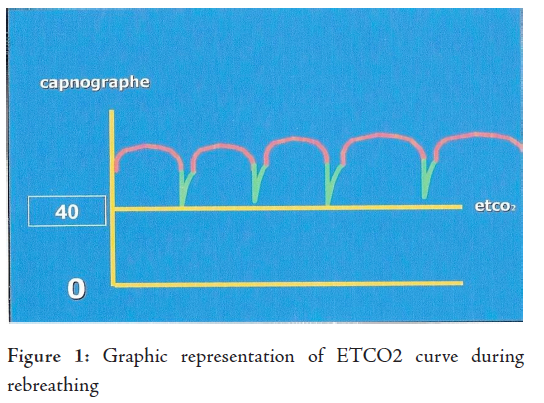
Initial parameters were normal, with an ETCO2 of 38 mmHg. After a few minutes, the rise of ETCO2 to 55mmHg necessitated checking the delivered gas flows, chest expansion and auscultation; nothing abnormal was detected. The capnograph sensor was changed; even then the end tidal carbon dioxide tension continued to rise, with an upward shift of the inspiratory carbon dioxide (IMCO2) baseline indicating rebreathing. After 30 minutes, the ETCO2 rose to 75 mmHg. The patient's arterial blood gas estimation showed severe hypercapnia and respiratory acidosis in a well oxygenated patient.
(pH 7.080; pCO2 95.3; pO2160.0; HCO3 27.6; O2Sat 98.2%) The haemodynamic parameters and body temperature remained normal. After confirming normal ventilator performance the coaxial circuit was changed. The ETCO2 curve began a dramatic fall towards the normal range of 40 mmHg and a return of baseline IMCO2 towards zero. Repeat arterial blood gas estimation was normal.
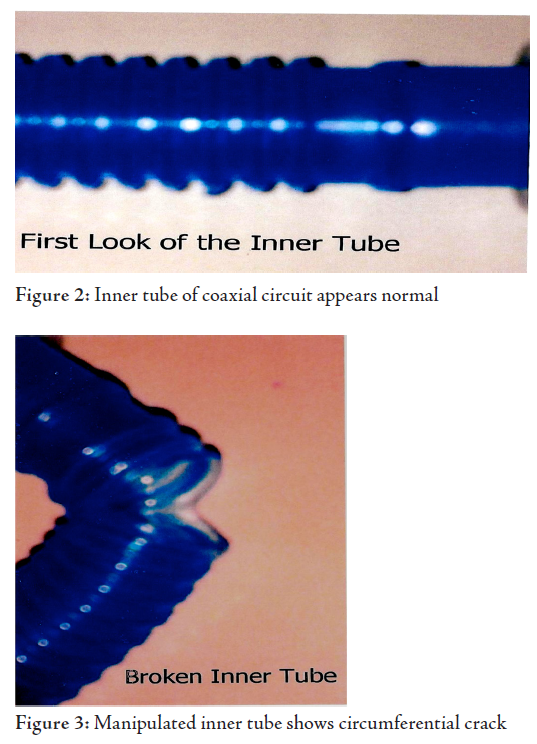
The surgery was completed and the patient was extubated with no adverse post operative event. Further visual examination of the faulty co-axial circuit did not reveal any defect in both outer transparent and inner coloured tubings, the attachments were well fixed at both the machine and patient ends. In order to explore the inner tube, the outer tube's distal connection was detached. A 2-3cm circumferential laceration of the inner tube was detected about 10 cm from the patient end of the circuit. This crack was otherwise invisible with normal assemblage of the circuit.
Bain's coaxial circuit was conceived and introduced into anaesthesia practice in 1972 by Bain and Spoerel.1 The inner, coloured tube which carries inspiratory gases may become faulty. Any disconnection or breech of its integrity increases the dead space breathing profoundly, followed by hypercapnia and its complications.
The circuits, usually supplied sterile, are reused after washing and drip dried. Due to cost considerations, it is common practice in most units to reuse these circuits. Early reports of malfunctioning of the inner tube soon came after its introduction into practice. Hanallah and Rosales in 1974 reported avulsion of the inner tube of a reused Bain's circuit with significant dead space breathing and hypercapnia, however, overt signs of hypercapnia were absent except for suspicious increase in blood loss.2 There are several other reports implicating detachment of the inner tube and consequent hypercarbia within the first hour of anaesthesia.3,4,5
Obstruction to flow through the inner tube of a coaxial circuit, due to compression, twisting or kinking is reported as gas flow failure to the patient end before induction of anaesthesia.6,7,8 Berner reported of a disconnection in the metallic part of the anaesthesia machine.9 His patient developed profound hypercapnia into the postoperative period. However, this present report, rare in the literature, is that of a malfunction of the inner tube resulting from a laceration of its wall and consequent dead space breathing evident in the first half hour of anaesthesia.
Hypercapnia induces catecholamine release. The patient may present with tachycardia, arrhythmias, excessive sweating, hypertension and peripheral vasodilatation which may result in excessive intraoperative blood loss. Berner reported haemodynamic changes, pupillary dilatation, hyperkalaemia and severe respiratory acidosis.9 Whereas Ghai et al. reported two cases of intraoperative arrhythmias.4 The patient in our report did not manifest these catecholamine responses of hypercapnia, probably due to masking by the depth of anaesthesia, or due to a delayed response. Neural and respiratory consequences of hypercapnia may be masked by anaesthesia, and cardiovascular complications are erroneously associated with light planes of anaesthesia. Other causes of intraoperative hypercapnia, including hypoventilation, poor soda lime function and malignant hyperpyrexia must be excluded.
Detection of any co-axial circuit malfunction is recommended in several tests:
several tests: -Visual inspection of tubings for obvious disruption and detection of gas flow obstruction.
This tests the low pressure system and the integrity of the inner tube. With the coaxial circuit connected to the anaesthetic machine and the patient end open, fresh gas flow of oxygen is set at 1L min-1 and the adjustable pressure limiting (APL) valve closed. Oxygen is then flushed via bypass through the circuit. Collapse of reservoir bag, by the creation of a Venturi effect, indicates an intact inner tube. Any defect in line will produce a negative result.
Foex-Crampton Smith Manouever 11
This occlusion test, which is more comprehensive, assesses the gas flow line from the flow meters of the machine to the patient end of the circuit. With oxygen flow at 2 liters min -1 the patient end of the inner tube is occluded briefly for 2 to 3 seconds using the forefinger.12 A positive test is indicated by descent of the rotameter bobbin due to back pressure; with removal of the finger, the bobbin ascends to its original position. Any breech of integrity gives a negative result. The possible accidental occlusion of the outer tube of the circuit may nullify the test with false results. Hence, Ghani suggested the use of the plunger of a 3 ml syringe to occlude the inner tube more precisely.13 With Ghani's method the movement of the rotameter bobbin is accompanied by a hissing sound on removal of the plunger. Intersurgical coaxial circuits now come with dedicated occlusion devices.
In our tests we found the 3 ml plunger is suitable for the Intersurgical Bain's circuit but inadequate for Ohmeda coaxial circuit, for which the plunger of a 5 ml syringe was more fitting, because of its larger tube diameter. Szypula et al. in their comparison of the two tests, found the occlusion test more sensitive than the Pethick test.14
Even though the reused circuits are washed without dismantling any components, the potential for damage from poor handling exists, especially as deterioration of plastic material is known to occur with constant exposure to anaesthetic gases. However, we could not explain the selective laceration of the inner tube in this case. Traumatic damage, if it is, would be expected to have affected the outer tube preferentially. However, it is important to note that even a new unused circuit has been implicated in a report of inner tube malfunction.7
CONCLUSIONThis report highlighted a case of severe hypercapnia due to dead space rebreathing complicating an unusual damage to the inner tube of a co-axial circuit.
The hidden potential for catastrophic complications which may result from a malfunction of the inner tube mandates a thorough check, test of patency and integrity of the inner tube of any coaxial circuit before use. The occlusion test is now recommended over the Pethick test by some associations.15
The reliance on cardiovascular manifestations of hypercapnia may delay correctional intervention as catecholamine response may be obtunded in deep anaesthesia. End tidal carbon dioxide monitoring is vital for early detection of hypercapnia. Jouan et al.
suggested that arterial blood gas should be checked in a patient with unexplained tachycardia and noncompliance with the ventilator in the presence of adequate and that liberal use of muscle relaxants is recommended.3
Overall, careful handling of circuits by experienced staff may prevent damage that may be costly to life. The rotational use of these circuits is recommended, with intervening periods of rest. Furthermore, the manufacturers should consider using more resilient material for the inner tube of co-axial circuits.
The authors reported no conflict of interest and no funding was received on this work.
-
Bain JA, Spoerel WE. A streamlined anaesthetic system. Cand Anaes Soc J 1972; 19:426.
Hanallah R, Rosales K. A hazard connected with re-use of the Bain's circuit: A case report. Cand Anaes Soc J 1974; 21:511-513.
Jouan ZT, Jawan B, Lee JH. Hypercarbia induced by detachment of inner fresh gas delivery tube of Bain circuit- a case report. Acta Anaesthesiol Sin 1995; 33(2):129-132.
Ghai B, Makkar JK, Bhati A. Hypercarbia and arrhythmias resulting from faulty Bain circuit: A report of two cases. Anesth Analg. 2006; 102:1903-1904.
Jellish WS, Nolan T, Kleinman B. Hypercapnia related to a faulty adult coaxial breathing circuit. Anesth Analg. 2001; 93(4):973-974.
Garg R. Kinked inner tube of coaxial Bain circuit-need for corrugated inner tube. J Anesth 2009; 23:306.
Gooch C, Peutrell J. A faulty Bain circuit. Anaesthesia 2004; 59: 618
Inglis MS. Torsion of inner tube- letter to editor. Br. J.Anaesth 1980; 52:705
Berner MS. Profound hypercapnia due to disconnection within an anaesthetic machine. Can J Anaesth 1987; 34:622-626.
Pethick SL. Letter to the editor. Can Anaesth Soc J 1975; 22:115.
Foex P, Crampton Smith A. A test for co-axial circuits. Anaesthesia 1977; 32:294.
Salt R. A test for coaxial circuits: a warning and a suggestion (letter). Anaesthesia 1977; 32:675.
Ghani GA. Safety check for the Bain Circuit. Can Anaesth Soc J 1984; 31:487-488.
Szypula KA, Ip JK, Bogod D, Yentis SM. Detection of inner tube defects in co-axial circle and Bain breathing systems: a comparison of occlusion and Pethick tests. Anaesthesia 2008; 63:1092-1095.
Checking Anaesthetic Equipment 3. The Association of Anaesthetists of Great Britain and Ireland: AAGBI, 2004.