Large Retrosternal Goitre: A Diagnostic and Treatment Dilemma
Gamal Khairy, Abdulaziz Alsaif
Khairy G, et al. OMJ. 25, (2010); doi:10.5001/omj.2010.44
ABSTRACT
Retrosternal goitre is usually referred to as enlarged thyroid gland with greater than 50% of its mass below the thoracic inlet. It has a clinical importance because its compressive symptoms may cause diagnostic problems and the selection of surgical approach is sometimes difficult. This report presents a case of shortness of breath in a young female who was treated as a case of long term asthma and was then discovered to have a huge retrosternal goitre extending down to the aortopulmonary window. The mass was resected through median sternotomy and the patient was discharged in a good condition and without further need for asthma treatment.
From Department of Surgery,Division of General Surgery, College of Medicine & King Saud University, King Khalid University Hospital
Received: 06 Mar 2010
Accepted: 02 Apr 2010
Address correspondence and reprint request to: Dr. Gamal Khairy, Associate Professor & Consultant General Surgeon, Division of General Surgery, Department of Surgery, College of Medicine & King Saud University, King Khalid University Hospital
E-mail: gkhairy@ksu.edu.sa
Khairy G, et al. OMJ. 25, (2010); doi:10.5001/omj.2010.44
INTRODUCTION
Traditionally, the term substernal goitre has been used to refer to an enlarged thyroid gland with greater than 50% of its mass below the thoracic inlet.1 It is of clinical significance because its growth between the sternum anteriorly and vertebral bodies posteriorly leads to impingment on the surrounding structures and has compressive symptoms. The incidence of substernal thyroid gland in the general population is difficult to ascertain. The repeated incidence in the general population varies from 0.02 to 0.5% based on chest X-ray screening reports.2 It accounts for 3-12% of mediastinal masses.3 This condition has a clinical importance because it presents a diagnostic dilemma with its compressive symptoms and operative difficulty as to which approach is most suitable for its management. This is a case of retrosternal goitre, where both the diagnosis and surgical treatment were difficult.
A 43 years-old female was presented to the emergency room complaining of shortness of breath. She had difficulty in breathing for 10 years and was diagnosed in a peripheral hospital as having bronchial asthma but her problem did not improve with medication. She did not notice any swelling in the neck and there were no features of hypo or hyperthyroidism. In the last week, the patient began to experience more difficulty in breathing even when lying down.
On examination, vital signs were stable. However, there was a small diffused swelling in the anterior aspect of the neck which moved when swallowing. The trachea was shifted to the right side. By percussion, there was dullness over the sternum. The patient was admitted to the medical ward for further checks.
All investigations were normal apart from the chest X-ray which showed tracheal shift. (Fig. 1)
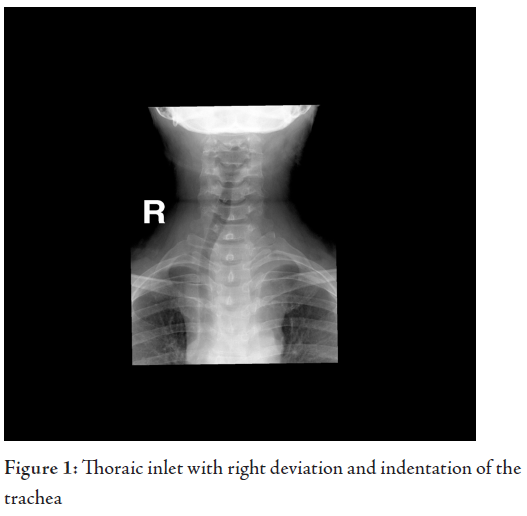
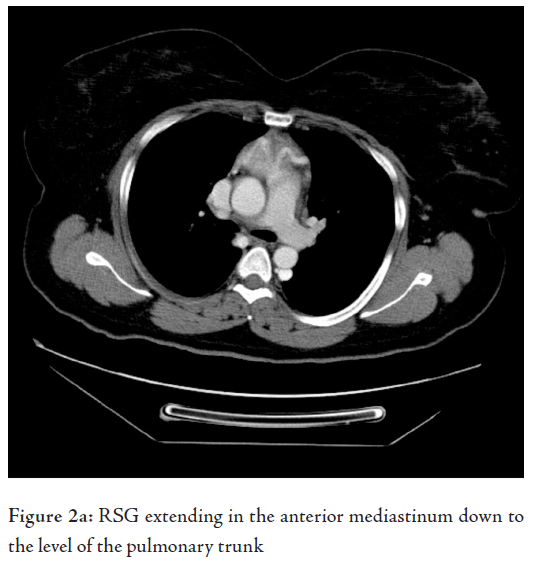
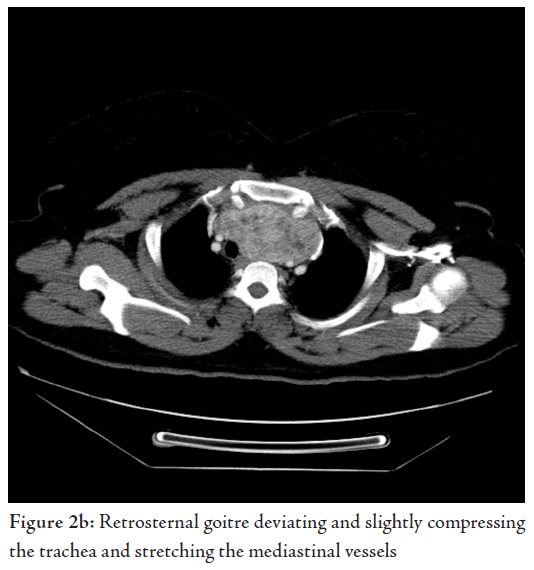
FNA showed a colloid goitre. CT scan of the neck and chest showed a large mass extending from the lower pole of the left thyroid gland down into the mediastinum, up to the level of the aortopulmonary (AP) window causing compression on the left brachio-cephalic vein with resultant engorgement of the hemiazygous venous system. There was also right deviation of the trachea and oesophagus, noted with localized luminal narrowing (Fig. 2). The patient was referred to the surgical team who discussed the case with the radiologist, the thoracic and the vascular surgeons. The latter suggested duplex for the carotids as the mass was engulfing the large vessels. Duplex scan showed normal carotid artery velocities and no significant compression by the mass. At surgery, it was difficult to deliver and resect the mass through the cervical approach only, therefore, a sternotomy was performed by the thoracic surgeon to excise the retrosternal goiter.
The carotid artery was injured during dissection of the gland from it as the latter was engulfing the artery and adherent to it.
Bleeding was controlled using vascular clamps until the vascular surgeon joined and repaired the injury. There was no residual effect from the injury. The other thyroid lobe was normal, therefore it was not removed. On the first post operative day, the patient was extubated, serum calcium was normal and she had an uneventful post operative recovery. The patient was doing well and continued follow ups in the surgical outpatient clinic for the last three years, and recently a duplex follow up two months ago was normal.
DISCUSSION
During embryonic development, thyroid tissue originating from the endoderm in the region of foramen cecum migrates through the neck to the level of the thyroid cartilage. Accessory thyroid tissue may present in the anterior, posterior or middle mediastinum. Terms such as retrosternal, substernal, intrathoracic, or mediastinal have been used to describe a goitre that extends beyond the thoracic inlet. However, there is a lack of consensus regarding the exact definition of a retrosternal goitre (RSG).4 The significant variability found in the literature regarding the clinical presentation and the surgical management of RSG can at least in some part, be explained by the different definitions employed.
In the studied patient, the swelling only involved the left lobe extending to the mediastinum. The majority of RSG are cervicomediastinal (79%), usually by extension of the left lobe of the thyroid. The rest were completely intrathoracicc (21%).2 The majority of patients present with shortness of breath or asthma like symptoms (68.8%) as was the case in the studied patient. Other modes of presentation include neck mass (75%), hoarseness of voice (37.5%), dysphagia (31.3%), stridor/wheezing (19%), or SVC obstruction (6.25%).5 The clinical presentation and the hormonal assay showed an euthyroid state in the studied patient. Thyrotoxic features were reported in less than 10% of RSG cases.6 The CT scan was the most useful tool showing the nature and extent of the lesion in the reported case. In a recent publication, the CT scan was considered the gold-standard preoperative radiological investigation.7 The mass could not be resected in the patient without sternotomy as it had extended to below the aortic arch. The cervical approach can be utilized in the majority of cases, however, cervical approach alone can increase the risks of surgery due to poor access in RSG extending to below aortic arch. For access in which the cervical approach is not adequate, intrathoracic approach should be employed including monubriotomy, full sternotomy and lateral thoracotomy. Full sternotomy (as was performed in the studied patient), has many advantages over lateral thoractomy as it has been proven that the incision can be performed quickly, reliably and with very low morbidity, providing
excellent exposure to the retrosternal portion of the gland. Moreover, it can be performed without having to reposition the patient.8,9 During surgery, the mass was extending posterior to the carotid artery engulfing it where the carotid artery was injured during dissection. This behaviour of the mass usually occurs in malignant lesions. Surprisingly, the histology suggested that it was a benign colloid goitre. In the reported series the incidence of malignancy in RSG was only 2-3%.10 Postoperatively, the patient did well with no respiratory problems. Tracheomalacia, contrary to popular belief is not a common problem and in most cases, like in this case, can be managed successfully by careful preassessment and intubation under direct vision.11 If tracheomalacia occurs in these patients, elective ventilation for few days allows a fibrous connection to develop between the tracheal wall and the surrounding structures hindering its collapse.3 The patient was discharged home comfortably without the treatment of asthma which she was receiving for 10 years.
CONCLUSION
Prognosis in RSG is very good if diagnosed and treated in the proper time. Almost all the compressive symptoms completely disappear (as was seen in this case), mortality reported is near zero and morbidity is very low.
The authors reported no conflict of interest and no funding was received on this work.
-
Newman E, Shah AR. Substernal goiter. J Surg Oncol 1995; 60:207-212.
-
Reeve TS, Rubenstein C, Rundle FF. Intrathoracic goiter: Its prevalence in Sydney metropolitan mass X-ray survey. Med J Austr 1957; 2:149-151.
-
Vadasz P, Kotsis L. Surgical aspects of 175 mediastinal goiters. Eur J Cardio-Thoracic Surgery 1998; 14:393-397.
-
Hunis CT, Gerogalas C, Mehrzad H, Tolley NS. A new classification system for retrosternal goiter based on a systemic review of its complications and management. Int J Surg 2008; 6:71-76.
-
Moran JC, Singer JA, Sardi A. Retrosternal goiter: A six-year institutional review. Am Surg 1998; 64: 889-893.
-
Hedayati N, McHenry CR. The clinical presentation and operative management of nodular and diffuse substernal thyroid disease. Am Surg 2002; 68: 245-251.
-
Grainger J, Saravanappa N, D?Souza A, Wilcock D, Wilson PS. The surgical approach to retrosternal goiters: the role of computerized tomography. Otolaryngol Head Neck Surg 2005 Jun; 132(6): 849-851.
-
Sand ME, Laws HL, McElvein RB. Substernal and intrathoracic goiter. Reconsideration of surgical approach. Am Surg 1983 Apr; 49(4):196-202.
-
Torre G, Borgonovo G, Amato A, Arezzo A, Ansaldo G, De Negri A. Surgical management of substernal thyroid gland. Laryngoscope 1998 Mar; 108(3):358-361.
-
Mach E. Management of patients with substernal goiters. Review. Surg Clin North Am 1995; 75:377-394.
-
Bennett AM, Hashmi SM, Premachandra DJ, Wright MM. The myth of tracheomalacia and difficult intubation in cases of retrosternal goiter. J Laryngol Otol 2004; 118;778-780. (Review)