A Rare Case of Brunneroma Duodenum causing Gastric Outlet Obstraction
Manjula Dhinakar,1 Dhia J. Allaya,2 Viswanathan Golash3
Dhinakar M. OMJ. 25, 44-46 (2010); doi:10.5001/omj.2010.11
ABSTRACT
A case of Brunneroma causing gastric outlet obstruction is presented with radiological, endoscopical findings which was removed laparoscopically.
From the 1Department of Radiology, Sultan Qaboos Hospital, Salalah, Sultanate of Oman; 2Department of Gastroenterology, Sultan Qaboos Hospital, Salalah, Sultanate of Oman; 3Department of Surgery, Sultan Qaboos Hospital, Salalah, Sultanate of Oman.
Reviewed: 20 Sep 2009
Accepted: 19 Oct 2009
Address correspondence and reprint requests to Dr. Manjula Dhinakar,Department of Radiology, Sultan Qaboos Hospital, Salahlah, Sultanate of Oman.
E-mail: arudhiman@yahoo.co.in
INTRODUCTION
Brunner gland adenoma, also known as Brunneroma or polypoidal Hamartoma, is a rare benign, proliferative lesion from the Brunner ‘s glands of the duodenum accounting for 10.6% of the benign tumors of the duodenum. They present as symptomatic tumors with duodenal/gastric outlet obstruction or with haemorrhage. This is a case report highlighting the clinical presentation, radiological, pathological features and therapy.
CASE REPORT
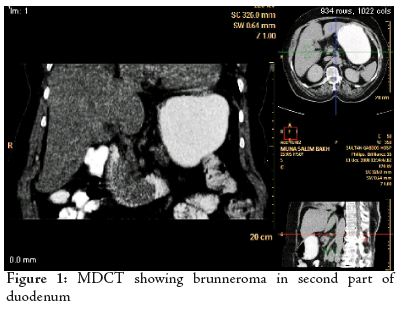
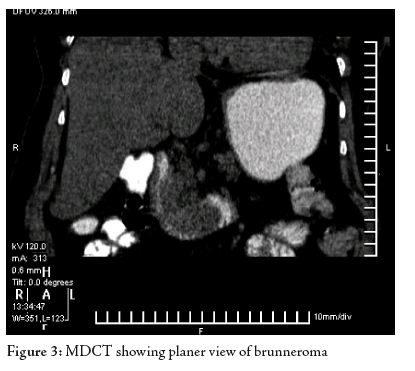
A 56 yr old female patient presented with features of on-and-off vomiting especially with solid food. She was very much at ease with liquid food. She had treatment with antacids and h2-blockers. Her symptoms of vomiting worsened. Her vital signs were normal. The blood parameters were within normal limits. The physical examination revealed no remarkable findings. The abdomen was soft. Upper endoscopy was planned to evaluate the sgastric outlet obstruction. Upper Endoscopy revealed a suspicious lesion in the duodenum with lobulated red colour tumor with smooth surface. Biopsy was not confirmatory and MDCT-Scan was planned. The CT-Scan with contrast showed a well defined large, smooth intraluminal hypodense lesion in the duodenum Occupying the 2nd and 3rd parts. (Figs. 1,2,3)
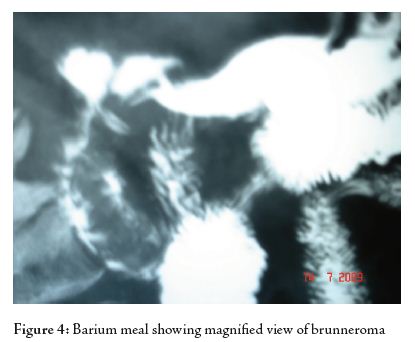
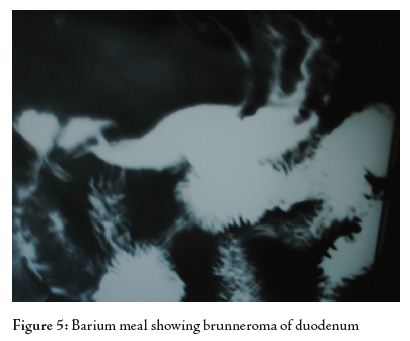
A propable diagnosis of benign lesion was considered after double contrast Barium study of the stomach and duodenum. There was a large polypoidal filling defect mass seen in the region of the duodenum. Endoscopic resection was not possible due to the broad base of the lesion. Laparoscopic surgery was performed and a polypoidal lesion was removed from the Posterior wall of the duodenum. The histopathology showed the smooth surface of the Tumor measuring about 5 x 2.5 x 1.4cms, (Figs. 4,5). No erosions or ulcers were seen. The cut surface showed grey red colour resembling the nodules. Microscopic examination showed Brunner’s gland hamartoma. The patient was discharged on the 10th postoperative day. The patient had successful laparoscopic treatment and was free of symptoms subsequently. Repeat study with Contrast revealed no mass lesion in the duodenum and showed normal transition.
DISCUSSION
Brunner’s glands consist of submucosal mucin-secreting glands located exclusively in the duodenum. They extend from the pylorus distally for a variable distance, usually at the first and second portions of the duodenum, and less frequently, stopping at the third and fourth portions.
Brunner’s glands secrete an alkaline fluid composed of viscous mucin, whose function appears to protect the duodenal epithelium from acid chyme of the stomach. It is a tumor without malignant predisposition. The malignant type is rare. Fujimaki et al. reported recently one patient with a focus atypical gland.1
Brunner’s gland adenoma is a rare tumor of the duodenum. These lesions are most commonly located in the duodenal bulb and clinical manifestations are variable. In symptomatic patients, the most common manifestations are GI hemorrhage and duodenal obstruction. Brunner’s gland adenoma that causes clinical symptoms is composed of hyperplastic Brunner’s glands and contains mostly an admixture of glandular, adipose, and muscular tissues, as was the case in the studied case.2
In barium examination, the findings are often nonspecific because there is usually a sessile or pedunculated polypoid-filling defect in the duodenal bulb. CT-Scan is promising as reported by Gourtsoyaiannis et al.3 It is still controversial whether asymptomatic Brunner’s gland tumors found incidentally needs surgical removal.3,4 Some people think that it needs no treatment, whereas others hold that endoscopic excision should be performed in order to prevent complications. Duodenal intussusception has been reported only in two patients, due to the fixation of the duodenum to the posterior abdominal wall.4 There are also reports of patients who complained of diarrhea owing to duodenal motor disturbances.5 There have been several reports that Brunner’s gland tumors could give rise to acute profuse bleeding, resulting in hypovolemic shock in patients.2,4,6,7
CONCLUSION
Symptomatic Brunner’s gland tumors, in the most accepted point of view, usually need surgical treatment. When the tumor is small or pedunculated, endoscopic polypectomy is the first choice. Open surgical excision is reserved for cases where snaring has failed or when tumor is too large.8,9 In this case, preoperative endoscopic biopsy gave a negative result, the lesion picked up well with MDCT and Double contrast Barium meal and the endoscopic snaring failed because of the larger size of the brunneroma, which was covered by a thick intact duodenal mucosa and the biopsy was not often deep enough to reach the submucosal tumor tissue. In the reported case, gastric outlet obstruction, was the presenting feature in the patient who had successful laparoscopic treatment and was free of symptoms postoperatively.
ACKNOWLEDGEMENTS
The author reported no conflict of interest and no funding has been received on this work.
-
Matsumoto T, Lida M, Matsui T, Yao T, Fujishima M. A Large Brunner gland adenoma removed by endoscopic polpectomy. Endoscopy 1990 Jul; 22(4):192-193.
-
Tan YM, Wong WK. Giant Brunneroma as an unusual cause of upper gastrointestinal hemorrhage: report of a case. Surg Today 2002; 32(10):910-912.
-
Gourtsoyaiannis NC. Radiological Appearences of Brunner gland Hamartoma. Eur J Radiology 1990 Dec; 11(3):188-190.
-
Peetz ME. Brunnergland Hyperplasia. Am Surgical Journal of Gastroenterology 1989 Jul; 55(7):474-477.
-
Fujimaki E, Nakamura S, Sugai T, Takeda Y. Brunner’s gland adenoma with a focus of p53-positive atypical glands. J Gastroenterol 2000; 35(2):155-158.
-
Levine JA. Clinical presentation and pathological features of Brunner gland Hamatoma of 27 cases. Am J Gastroenterol 1995 Feb; 90(2):290-294.
-
Wagholikar GD, Dhingra S, Krishnani N, Kapoor VK. Large Brunneroma presenting with bleeding. Department of Surgical Gastroenterology Indian J Gastroenterol 2002 Sep-Oct; 21(5):201-202.
-
Kang BK, Park NS, Jin DH, Ahn TH, Park MB, Lee KJ, et al. Endoscopic resection of a giant duodenal Brunner’s gland adenoma. [Article in Korean] Gastroenterol 2008 Aug; 52(2):106-109.
-
Rocco A, Borriello P, Compare D, De Colibus P, Pica L, Iacono A, et al. Large Brunner’s gland adenoma: case report and literature review. World J Gastroenterol 2006 Mar; 12(12):1966-1968.