A Case Report of Basal Ganglia Calcification - A Rare
Finding of Hypoparathyroidism
Ramen C. Basak
Basak R. OMJ. 24, 220-222 (2009); doi:10.5001/omj.2009.43
ABSTRACT
Physiological intracranial calcification occurs in about 0.3-1.5% of cases. It is asymptomatic and detected incidentally by neuroimaging. Pathological basal ganglia calcification is due to various causes, such as: metabolic disorders, infectious and genetic diseases. Hypoparathyroidism and pseudohypoparathyroidism are the most common causes of pathological basal ganglia calcification. Besides tetany and seizures this condition is presented by parkinsonism and dementia. Such parkinsonism does not respond to drugs containing levodopa. Infections (toxoplasmosis, rubella, cytomegalovirus, cysticercosis, AIDS) give multiple and asymmetric intracranial calcification. Inherited and neurodegenerative diseases cause symmetrical, bilateral basal ganglia calcification which is not related to metabolic disorders. Since adequate treatment of hypoparathyroidism may lead to marked clinical improvement, serum concentration of calcium, phosphorus, and parathyroid hormone (PTH) is suggested to be determined in all individuals with calcification of the basal ganglia to rule out hypoparathyroidism.
From the Department of Internal Medicine, KKGH, Hafr Al Batin, Saudi Arabia.
Received: 09 Mar 2009
Accepted: 21 April 2009
Address of Correspondence: Dr. Ramen Chandra Basak, King Khaled General Hospital, Hafr-Al-Batin, KSA.
E-mail: basakrc@yahoo.com
INTRODUCTION
Hypoparathyroidism is an endocrine disorder caused as result of congenital disorders, iatrogenic causes (eg, drugs, removal of the parathyroid glands during thyroid or parathyroid surgery, radiation), infiltration of the parathyroid glands (eg, metastatic carcinoma, Wilson’s disease, sarcoidosis), suppression of parathyroid function such as in hypomagnesemia, HIV/AIDS, or idiopathic mechanisms. Idiopathic Hypoparathyroidism is diagnosed when all the possible causes of hypoparathyrodism are ruled out. Hypoparathyroidism by any cause is well known to basal ganglia calcification in most of the patients. It is also well known that extensive intracranial calcification caused by hypoparathyrodism is rare. This report presents a case of idiopathic hypoparathyroidism which presented with extensive intracranial calcification.
CASE REPORT
A 40-year-old Egyptian male school teacher presented in the emergency department of King Khaled General Hospital, Hafr-Al Batin, KSA with a new-onset generalized tonic-clonic seizure and tongue bite. The patient did not have a history of hypocalcemia, seizures, psychiatric disorders or obvious cognitive impairments. On examination, Chvostek’s and Trousseau’s signs were positive. Fundoscopy was normal. He had no dysmorphic features. Investigations revealed that his serum calcium was 5.1mg% (N 8-10.5 mg %), PTH 1.2 (N 15 - 62 pg/ml), phosphate 7 mg% (N 2.5 – 5 mg %), magnesium 1.2 mg% (1-1.4 mg %) with normal albumin, alkaline phosphatase and renal function test. CT scan revealed basal ganglia calcification. Contrast enhanced spiral CT performed showed bilateral extensive nonenhancing hyper dense calcification involving the thalamus, dentate nuclei, putamen, globus pallidus, caudate nucleus and cerebellum. (Fig. 1, Fig. 2) With these investigations, after ruling out of other causes of hypoparathyrodism the possibility of idiopathic hypoparathyrodism was suggested. The patient was treated with intravenous calcium gluconate, oral calcium carbonate (CaCo3) 600 mg thrice a day and alfacalcidol 1µg daily.
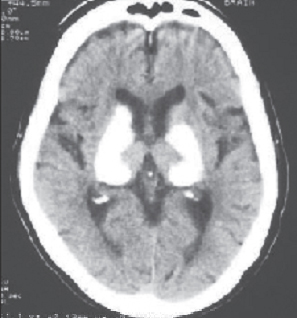
Figure 1. Extensive Calcification of the Basal Ganglia
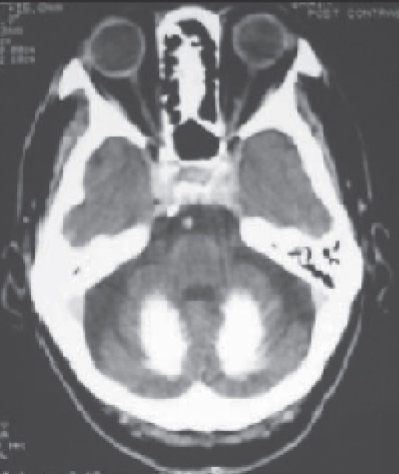
Figure 2. Calcification of the Cerebellum
DISCUSSION
Hypoparathyroidism is an endocrine disorder caused as a result of congenital disorders, iatrogenic causes, infiltration of the parathyroid glands, suppression of parathyroid function, or idiopathic mechanisms.1 In these cases either there will be apparent deficiency of PTH secretion or end-organ failure.2 Idiopathic hypoparathyroidism is an uncommon condition of unknown etiology. Acquired and congenital hypoparathyroidism would have either normal or undetectable PTH levels with hypocalcaemia whereas in idiopathic hypoparathyroidism both calcium and PTH levels are low. 2 In pseudo hypoparathyroidism PTH levels will be high with hypocalcaemia. In pseudopseudohypoparathyroidism with increased PTH level both serum calcium and phosphorus levels are normal.2 Prevalence of hypoparathyroidism is equal in men and women and occurs in all age groups. A literature review of the clinical presentations of basal ganglia calcification revealed that there are diverse presentations, the most common including seizures, mental deterioration, and disorders of cerebellar or extra-pyramidal function. Movement disorders, chorea, or parkinsonism are present in 20 - 30% of patients with basal ganglia calcification, while some patients are asymptomatic.3
Radiologically hypoparathyroidism causes calcification most often in bilateral basal ganglia.4 The most common site is often globus pallidus.5 Calcification can also occur in the cerebellum, sub cortical white matter, corona radiata and the thalamus. Cerebral deposition of calcium occurs in many pathological brain processes. Calcification, particularly of the basal ganglia, is associated with hypoparathyroidism of any type and, rarely, with other metabolic diseases; as a familial trait; and sporadically, without abnormal calcium metabolism (BOX). The emergence of CT has led to the finding that sporadic calcification is the most common form, present in up to 1.5% of all brain scans.6
Brain calcinosis syndrome (BCS) is usually defined as bilateral calcium accumulation in the brain parenchyma, most often within the basal ganglia. Various terms have been used to describe intracranial calcification including calcification(s) of the basal ganglia, basal ganglia calcification(s), Fahr syndrome, intracranial calcification, pallidal calcification, and striopallidodentate calcinosis. More than 50 reported clinical conditions have been associated with BCS, including sporadic entities and the heredofamilial conditions. Before CT, 70% to 80% of brain calcification detected on plain skull radiography was associated with hypoparathyroidism.7 However, about 80% of patients with BCS have no disturbances of calcium or phosphorus metabolism, and most patients with BCS have no clinical symptoms. Therefore, physiological calcinosis, probably related to aging, is the most common cause of BCS.8,9,10,11,12
The immediate treatment for all types is calcium supplement with supplementation
of PTH in cases of acquired hypoparathyroidism. Also one has to treat
symptomatically for the seizures and other changes. This disease has a good
prognosis if detected early and treated.13
Since adequate treatment of hypoparathyroidism may lead to marked clinical
improvement, determination of serum calcium, phosphorus, and parathyreoid
hormone is mandatory in all individuals with calcification of the basal ganglia
to rule out hypoparathyroidism.
Causes of Symmetrical Calcification of the Basal Ganglia (BOX)
Physiological
Hypoparathyroidism (various causes including
pseudohypoparathyroidism)
Hyperparathyroidism
Familial idiopathic cerebral calcification (Fahr’s syndrome)
Birth anoxia
Carbon monoxide intoxication
Lead poisoning
Tuberous sclerosis
Cockayne’s syndrome
Postinfectious
Acquired immunodeficiency syndrome (especially in children)
Radiation therapy
Methotrexate therapy
Kearns-Sayre syndrome and other mitochondrial diseases
Familial encephalopathies
Down syndrome
CONCLUSION
Since adequate treatment of hypoparathyroidism may lead to marked clinical improvement and due to its rarity, it is warranted to do serum concentration of calcium, phosphorus, and parathyroid hormone in all individuals with calcification of the basal ganglia to rule out hypoparathyroidism.
ACKNOWLEDGEMENTS
The authors reported no conflict of interest and no funding has been received on this work.
-
Girija AS. Idiopathic hypoparathyroidism with extensive intracranial calcification associated with kinesogenic choreoathetosis. J Assoc Physicians India. 2000;48:938-9.
-
Hypoparathyroidism, pseudohypoparathyroidism, pseudopseudohypo-parathyroidism, chapter metabolic and endocrine disease of the skeleton.by J.B.Vogler III and J.H.Kim -Diagnostic Radiology 4th edition, volume three.
-
Koller WC, Cochran JW, Klawans HL. Calcification of the basal ganglia: computerized tomography and clinical correlation. Neurology 1979;29:328-33.
-
Fulop M, Zeifer B. Extensive brain calcification in hypoparathyroidism. Am J Med Sci. 1991;302: 292-5.
-
Vakaet A, Rubens R, de Reuck J, vander Eecken H. Intracranial bilateral symmetrical calcification on CT-scanning. Clin Neurol Neurosurg. 1985;87:103-11.
-
Riley DE, Lang AE Bradley WG, Daroff RB, Fenichel GM, Marsden CD. Neurology in clinical practice. Boston: Butterworth-Heinemann; 2000:1927-8.
-
Löwenthal A, Bruyn GW. Calcification of the striopallidodentate system. In: Vinken PJ, Bruyn GW, eds. Handbook of Clinical Neurology. Amsterdam, the Netherlands: North-Holland Publishing Co; 1968:703-25.
-
Harrington MG, Macpherson P, McIntosh WB, Allam BF, Bone I. The significance of the incidental finding of basal ganglia calcification on computed tomography. J Neurol Neurosurg Psychiatry. 1981;44:1168-70.
-
Kazis AD. Contribution of CT scan to the diagnosis of Fahr’s syndrome. Acta Neurol Scand. 1985;71:206-11.
-
Fenelon G, Gray , Paillard F, Thibierge M, Mahieux F, Guillani A. A prospective study of patients with CT detected pallidal calcifications. J Neurol Neurosur Psychiatry. 1993;56:622-25.
-
Murphy MJ. Clinical correlations of CT scan-detected calcifications of the basal ganglia. Ann Neurol. 1979;6:507-11.
-
Cohen CR, Duchesneau PM, Weinstein MA. Calcification of the basal ganglia as visualized by computed tomography. Radiology. 1980;134:97-9.
-
Litvin Y, Rosler A, Bloom RA.Extensive cerebral calcification in hypoparathyroidism. Neuroradiology. 1981;21:271-2.